Back
Poster, Podium & Video Sessions
Video
V07: Prostate, Penile, Testis & Misc. Oncology I
V07-12: Robotic Prostatectomy with Wide Excision for Locally Advanced Prostate Cancer
Sunday, May 15, 2022
8:50 AM – 9:00 AM
Location: Video Abstracts Theater
Jeffrey Vehawn*, Mouneeb Choudry, Austen Slade, Jacob Ambrose, Alejandro Sanchez, Christopher Dechet, Salt Lake City, UT
.jpg)
Jeffrey Vehawn, BA
Huntsman Cancer Institute, University of Utah
Video Presenter(s)
Introduction: Locally advanced prostate cancer (PCa) is considered as high-risk disease with a poor prognosis. In this setting, the European Association of Urology (EAU) and the National Compressive Cancer Network (NCC) guidelines recommend radical prostatectomy as part of multimodal therapy. In recent years several variations of the standard robotic-assisted radical prostatectomy (RARP) approach have been described. Our aim was to describe our modified RARP technique for locally advanced PCa patients and report perioperative and long-term oncological outcomes.
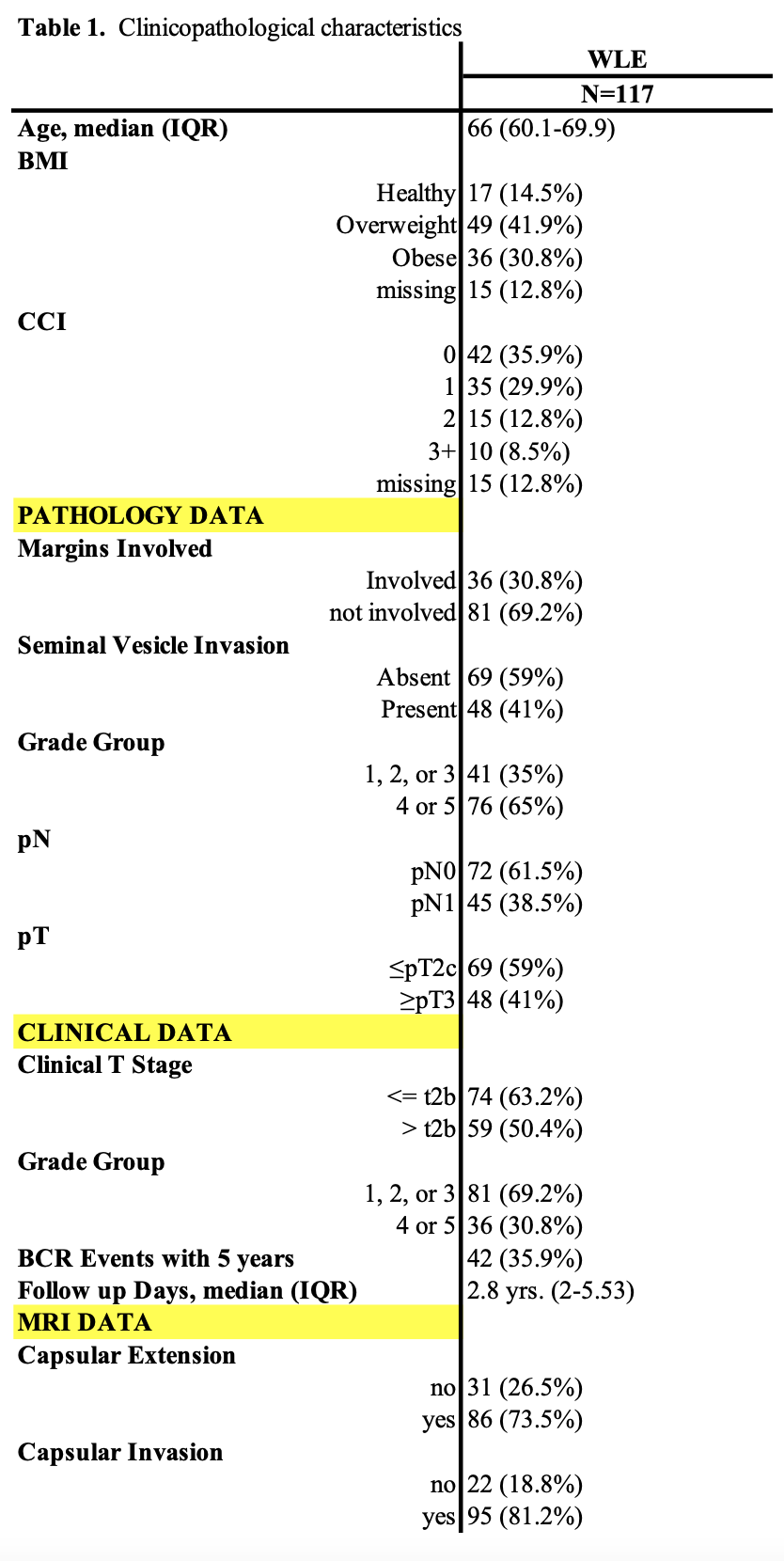
Methods: Our cohort was derived from a prospectively maintained institutional prostate cancer database. We identified 117 men with high-risk or locally advanced PCa treated with RARP (wide excision) and pelvic lymph node dissection between 2008-2018 by a single expert robotic surgeon at the Huntsman Cancer Institute. Only patients with a minimum of 2 years follow-up were included. Post-operative outcomes were analyzed in patients with complete follow-up data. Post-operative outcomes were measured using univariate cox-proportional hazard models, modeling for BCR survival in wide local excision patients.
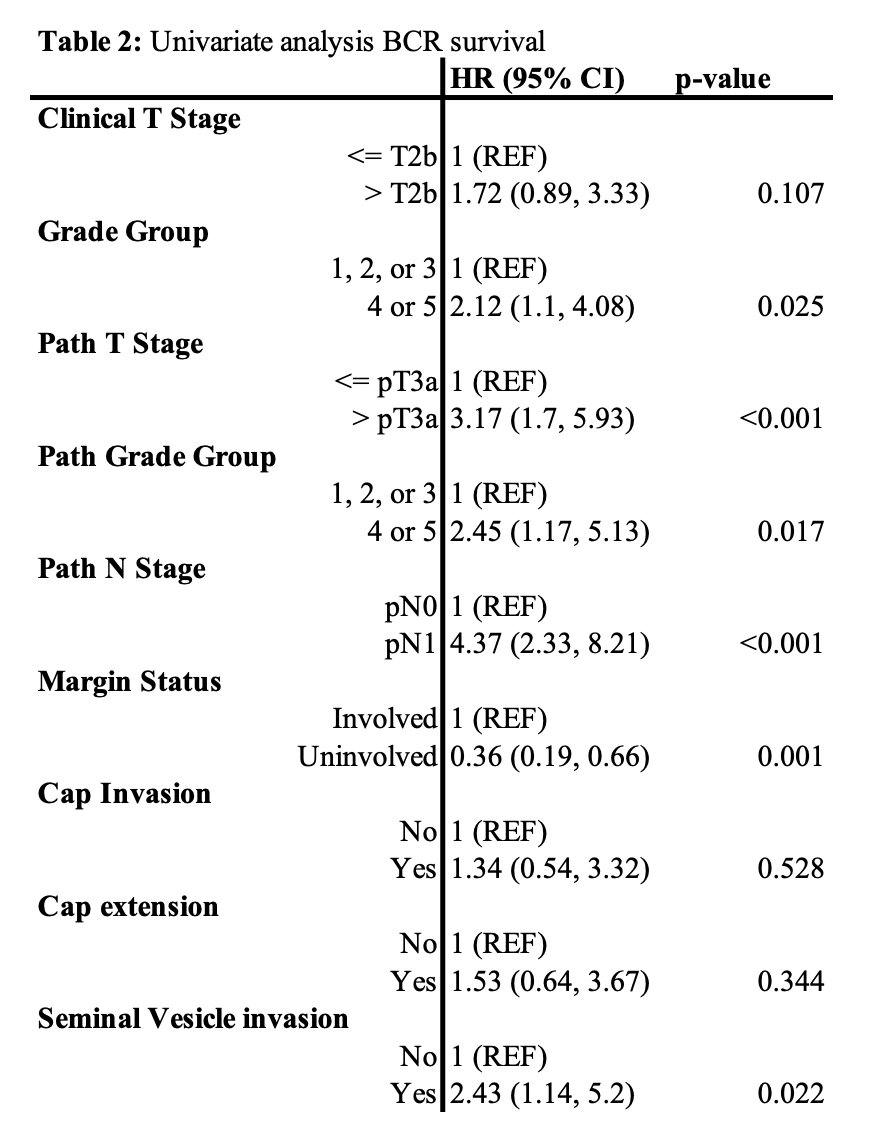
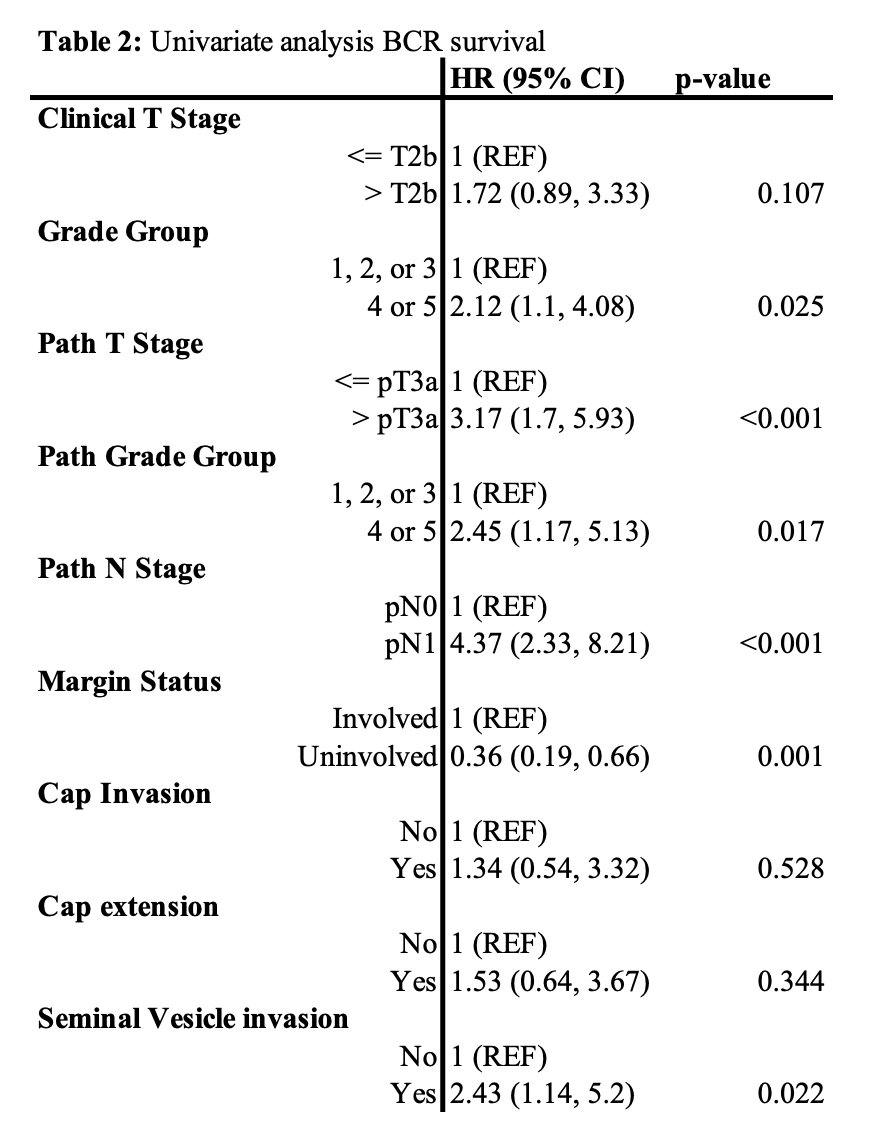
Results: The median age of men was 66 (IQR: 60.1-69.9) with a median follow-up of 2.8 years (IQR: 2-5.53). Overall, 41% of men had a pathological T-stage of =pT3 and 38.5% of men had a N-stage of pN1. 81.2% and 73.5% of patients had capsular extension and capsular invasion, respectively, on preoperative MRI. 69.2% of patients had negative surgical margins. At 5-year follow-up, 64.1% of men achieved BCR-free survival. From our univariate analysis, grade group, pathologic T- and N-stage, and margin status were all independent predictors of BCR.
Conclusions: In this study we presented a revised RARP approach for patients with locally advanced or high-risk prostate cancer. This technique is associated with good post-operative oncological outcomes and may assure biochemical control of the disease in complex PCa patients.
Source of Funding: This research was funded by the Huntsman Cancer Institute at the University of Utah.
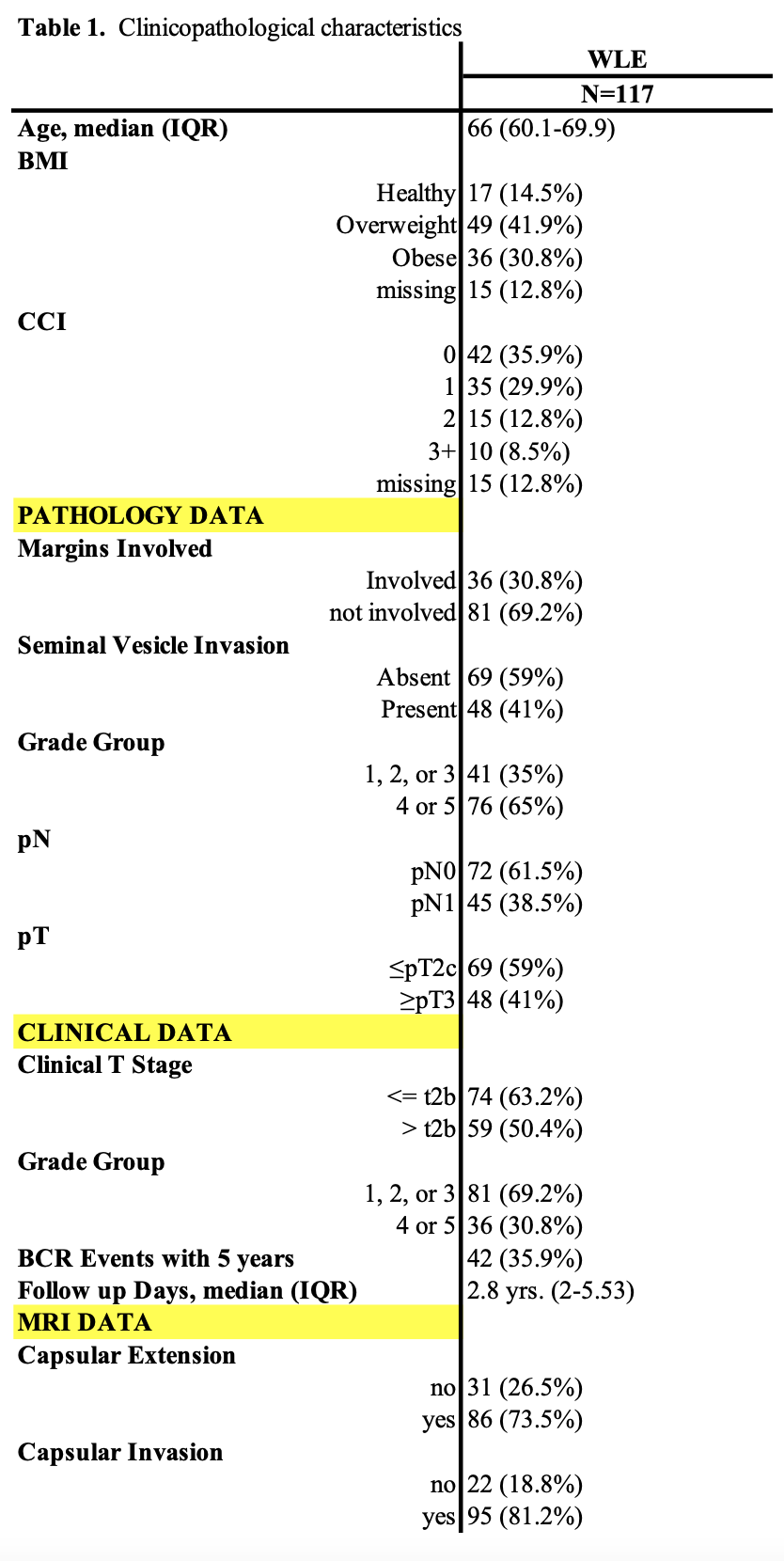
Methods: Our cohort was derived from a prospectively maintained institutional prostate cancer database. We identified 117 men with high-risk or locally advanced PCa treated with RARP (wide excision) and pelvic lymph node dissection between 2008-2018 by a single expert robotic surgeon at the Huntsman Cancer Institute. Only patients with a minimum of 2 years follow-up were included. Post-operative outcomes were analyzed in patients with complete follow-up data. Post-operative outcomes were measured using univariate cox-proportional hazard models, modeling for BCR survival in wide local excision patients.
Results: The median age of men was 66 (IQR: 60.1-69.9) with a median follow-up of 2.8 years (IQR: 2-5.53). Overall, 41% of men had a pathological T-stage of =pT3 and 38.5% of men had a N-stage of pN1. 81.2% and 73.5% of patients had capsular extension and capsular invasion, respectively, on preoperative MRI. 69.2% of patients had negative surgical margins. At 5-year follow-up, 64.1% of men achieved BCR-free survival. From our univariate analysis, grade group, pathologic T- and N-stage, and margin status were all independent predictors of BCR.
Conclusions: In this study we presented a revised RARP approach for patients with locally advanced or high-risk prostate cancer. This technique is associated with good post-operative oncological outcomes and may assure biochemical control of the disease in complex PCa patients.
Source of Funding: This research was funded by the Huntsman Cancer Institute at the University of Utah.

.jpg)
.jpg)