Back
Poster, Podium & Video Sessions
Late-breaking Abstract II - Benign Disease
LBA02-09: Intracellular SARS-CoV-2 found in the spermatozoa of convalescent men with negative PCR semen samples revealed by Electron Microscopy.
Sunday, May 15, 2022
4:50 PM – 5:00 PM
Location: Room 243
Jorge Hallak, ELIA TAMASO ESPIN GARCIA CALDINI, Maria Cássia Jacintho Mendes Corrêa, Marisa Dolhnikoff, PAULO HILARIO NASCIMENTO SALDIVA, ESPER GEORGES KALLAS, AMARO NUNES DUARTE NETO, RAUL SEGUNDO SANCHEZ GUTIERREZ, Joel R Drevet, Thiago Afonso Carvalho Celestino Teixeira, Felipe Saraiva Bernardes, HELOISA FAQUINETI
- JH
Jorge Hallak, MD, PHD
Full Professor of Urology
Podium Presenter(s)
Introduction: SARS-CoV-2 can invade different testicular cell types, such as spermatogonia, spermatids, Sertoli, and Leydig cells. We investigated the viral presence inside the sperm of negative PCR infected men up to 3 months after discharge from the hospital.
Methods: This cross-sectional study included 13 of a 26 moderate-to-severe SARS-CoV-2 infected men cohort (mean 34.3 ± 6.5 years; range: 21–50 years old). Patients were enrolled 30 to 90 days after the diagnosis. Semen samples were obtained by masturbation and processed within one hour according to WHO guidelines. All patients were PCR negative for the virus in the ejaculate. Samples were liquefied for 30 min at room temperature in 0.1M phosphate buffer before centrifuging at 500 g for 10 min. The supernatant was removed, and pellets were fixed in 2,5% v/v glutaraldehyde in 0.1M phosphate buffer for 2h at 4°C, post-fixed in 1% OsO4 for 1h at 4°C, stained overnight in 1% aqueous uranyl acetate. Then, the pellets were dehydrated sequentially in 30%, 70%, and 100% ethanol and embedded in epoxy resin. Ultrathin sections (70nm) were obtained in an ultramicrotome, collected on nickel grids, and double-stained by uranyl acetate and lead citrate. Micrographs were obtained with a Jeol JEM 1010 electron microscope (Tokyo, Japan, 80 kV).
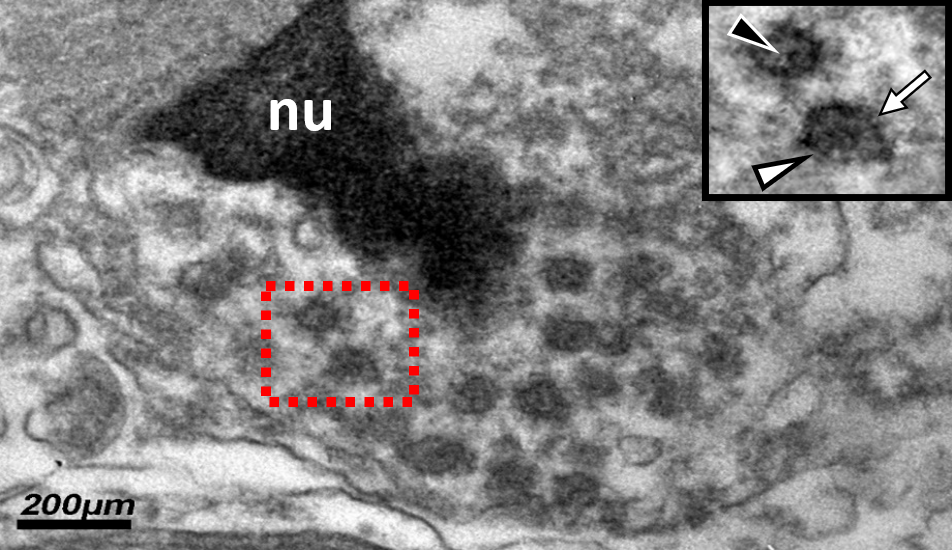
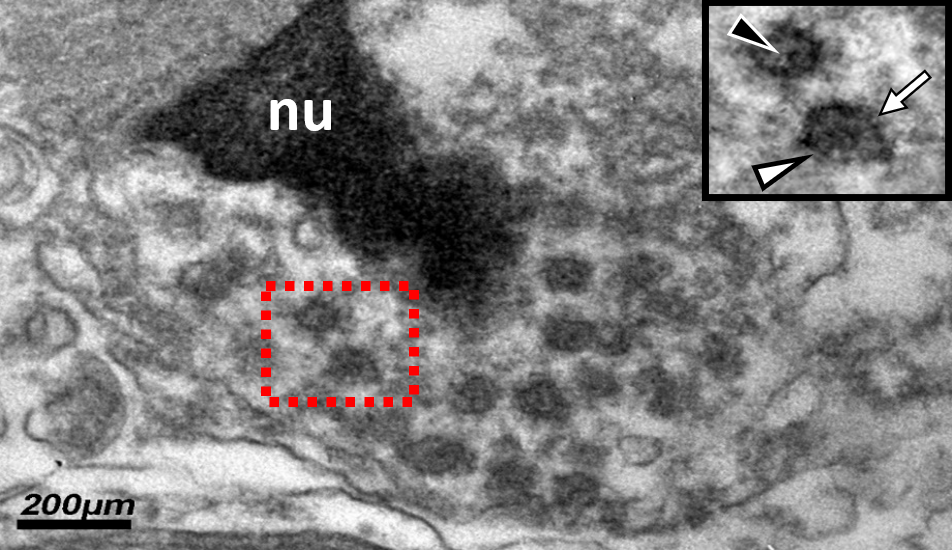
Results: We identified viruses inside spermatozoa in 9/13 patients up to 90 days after discharge from the hospital. Moreover, in all 13 men, a type of DNA-based extracellular traps, probably in a cfDNA-dependent manner, like described in the COVID-19 systemic inflammatory response .
FIGURE: High magnification electron micrograph of a spermatozoon with the nucleus (nu) displaying the typical condensed chromatin. The remained cytoplasm contains several viral particles (ranging in diameter from 90 to 110 nm). The inset corresponds to a higher magnification of the boxed area containing two virions, showing the SARS-CoV-2 characteristics: viral envelope (white arrowhead), nucleocapsids (black arrowhead), and spike-like projections (white arrow).
Conclusions: Although SARS-CoV-2 is not found in the infected men’s semen, it was intracellularly present in the spermatozoa. The potential implications for assisted conception should be addressed.
Source of Funding: none
Methods: This cross-sectional study included 13 of a 26 moderate-to-severe SARS-CoV-2 infected men cohort (mean 34.3 ± 6.5 years; range: 21–50 years old). Patients were enrolled 30 to 90 days after the diagnosis. Semen samples were obtained by masturbation and processed within one hour according to WHO guidelines. All patients were PCR negative for the virus in the ejaculate. Samples were liquefied for 30 min at room temperature in 0.1M phosphate buffer before centrifuging at 500 g for 10 min. The supernatant was removed, and pellets were fixed in 2,5% v/v glutaraldehyde in 0.1M phosphate buffer for 2h at 4°C, post-fixed in 1% OsO4 for 1h at 4°C, stained overnight in 1% aqueous uranyl acetate. Then, the pellets were dehydrated sequentially in 30%, 70%, and 100% ethanol and embedded in epoxy resin. Ultrathin sections (70nm) were obtained in an ultramicrotome, collected on nickel grids, and double-stained by uranyl acetate and lead citrate. Micrographs were obtained with a Jeol JEM 1010 electron microscope (Tokyo, Japan, 80 kV).
Results: We identified viruses inside spermatozoa in 9/13 patients up to 90 days after discharge from the hospital. Moreover, in all 13 men, a type of DNA-based extracellular traps, probably in a cfDNA-dependent manner, like described in the COVID-19 systemic inflammatory response .
FIGURE: High magnification electron micrograph of a spermatozoon with the nucleus (nu) displaying the typical condensed chromatin. The remained cytoplasm contains several viral particles (ranging in diameter from 90 to 110 nm). The inset corresponds to a higher magnification of the boxed area containing two virions, showing the SARS-CoV-2 characteristics: viral envelope (white arrowhead), nucleocapsids (black arrowhead), and spike-like projections (white arrow).
Conclusions: Although SARS-CoV-2 is not found in the infected men’s semen, it was intracellularly present in the spermatozoa. The potential implications for assisted conception should be addressed.
Source of Funding: none

.jpg)
.jpg)