Back
Poster, Podium & Video Sessions
Moderated Poster
MP15: Prostate Cancer: Localized: Surgical Therapy I
MP15-03: Prognostic Value of Lymphovascular Invasion in Patients Treated with Salvage Radical Prostatectomy for Radiation-Recurrent Prostate Cancer
Friday, May 13, 2022
2:45 PM – 4:00 PM
Location: Room 222
Stephan Brönimann*, Fahad Quhal, Ekaterina Laukhtina, Benjamin Pradere, Vienna, Austria, Alberto Briganti, Milan, Italy, Pawel Rajwa, Vienna, Austria, Axel Heidenreich, Cologne, Germany, Shahrokh F. Shariat, Vienna, Austria

Stephan Broenimann, MD (he/him/his)
Attending Urologist
Johns Hopkins University
Poster Presenter(s)
Introduction: It is estimated that 20-50% of patients treated with radiation therapy for localized prostate cancer (PCa) will eventually develop recurrence. Radical prostatectomy(RP) is considered a salvage therapeutic option for these patients with potential cure. However, large portion of patients continue to develop recurrence despite this approach.
Lymphovascular invasion (LVI) have been shown to be associated with adverse outcomes after primary RP. However, its prognostic value has not been evaluated in patients with radiation-recurrent (PCa) undergoing salvage radical prostatectomy (SRP).
Methods: A retrospective analysis was conducted on 214 patients treated with SRP in five tertiary referral centers from January 2007 to December 2015. Univariable and multivariable Cox regression analyses were performed to test the association between LVI and BCR and survival outcomes. Logistic regression analyses were used to test the association between LVI and pathologic features.
Results: Patients with LVI were more likely to have higher Gleason score, advanced pathologic tumor stage, and lymph node metastasis. The median follow-up duration was 25.1 months (IQR 4.8-27.9).
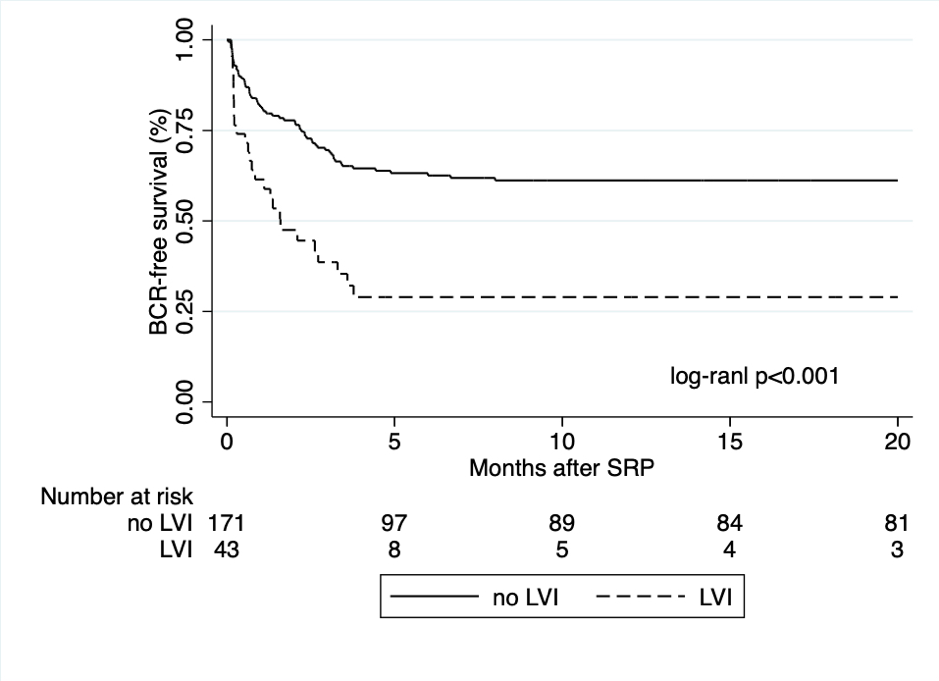
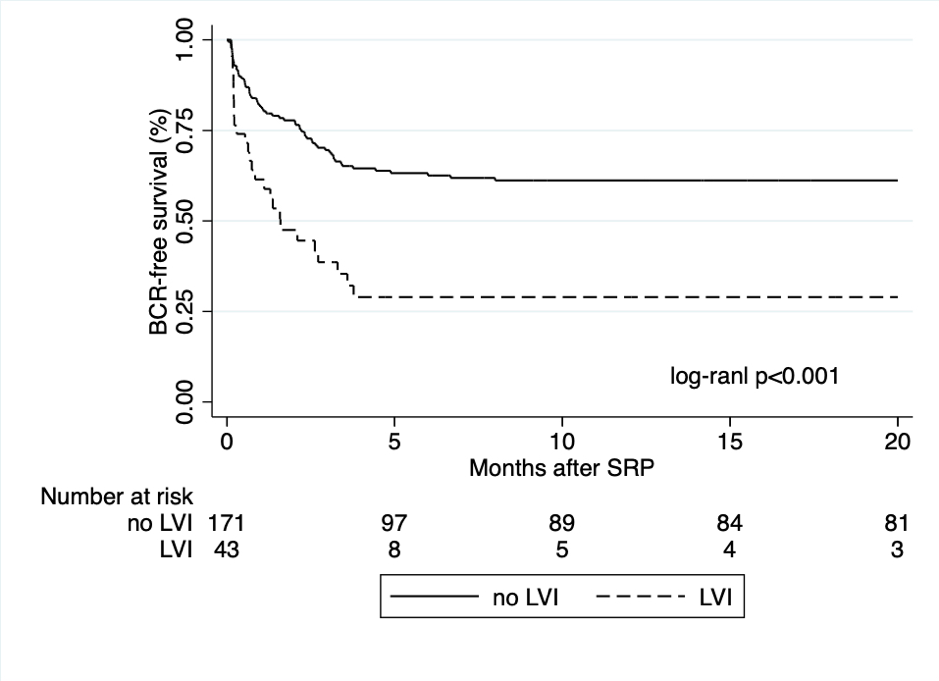
On univariable Cox regression analyses, LVI was significantly associated with biochemical recurrence (BCR) free survival [hazard ratio (HR 2.55, 95% CI 1.62–20.02; P<0.001) (Figure.1), metastasis free survival (MFS) (HR 2.91, 95% CI 1.23–6.89; P=0.015) and overall survival (OS) (HR 3.96, 95% CI 1.22–12.88; P=0.022). However, LVI did not retain its statistically significant association on multivariable Cox regression analyses after adjusting for the established clinicopathological features (BCR P= 0.12, MFS P= 0.89, and OS P= 0.73).
On logistic regression analyses, LVI was significantly associated with the rate of extracapsular tumor extension) (Odds ratio (OR) 4.66, 95% CI 2.23–9.73; P<0.001) and lymph node involvement (OR 10.42, 95% CI 4.77–22.75; P<0.001), but not with the rates of positive surgical margins (p=0.32).
Conclusions: LVI might serve as an indicator of adverse pathologic features. However, no direct association was noted on BCR and survival outcomes. Further studies with longer follow-up periods are needed to further evaluate the predictive value of LVI on this group of patients.
Source of Funding: no funding
Lymphovascular invasion (LVI) have been shown to be associated with adverse outcomes after primary RP. However, its prognostic value has not been evaluated in patients with radiation-recurrent (PCa) undergoing salvage radical prostatectomy (SRP).
Methods: A retrospective analysis was conducted on 214 patients treated with SRP in five tertiary referral centers from January 2007 to December 2015. Univariable and multivariable Cox regression analyses were performed to test the association between LVI and BCR and survival outcomes. Logistic regression analyses were used to test the association between LVI and pathologic features.
Results: Patients with LVI were more likely to have higher Gleason score, advanced pathologic tumor stage, and lymph node metastasis. The median follow-up duration was 25.1 months (IQR 4.8-27.9).
On univariable Cox regression analyses, LVI was significantly associated with biochemical recurrence (BCR) free survival [hazard ratio (HR 2.55, 95% CI 1.62–20.02; P<0.001) (Figure.1), metastasis free survival (MFS) (HR 2.91, 95% CI 1.23–6.89; P=0.015) and overall survival (OS) (HR 3.96, 95% CI 1.22–12.88; P=0.022). However, LVI did not retain its statistically significant association on multivariable Cox regression analyses after adjusting for the established clinicopathological features (BCR P= 0.12, MFS P= 0.89, and OS P= 0.73).
On logistic regression analyses, LVI was significantly associated with the rate of extracapsular tumor extension) (Odds ratio (OR) 4.66, 95% CI 2.23–9.73; P<0.001) and lymph node involvement (OR 10.42, 95% CI 4.77–22.75; P<0.001), but not with the rates of positive surgical margins (p=0.32).
Conclusions: LVI might serve as an indicator of adverse pathologic features. However, no direct association was noted on BCR and survival outcomes. Further studies with longer follow-up periods are needed to further evaluate the predictive value of LVI on this group of patients.
Source of Funding: no funding

.jpg)
.jpg)