Back
Poster, Podium & Video Sessions
Moderated Poster
MP15: Prostate Cancer: Localized: Surgical Therapy I
MP15-08: Pathological, functional and oncological best-case scenarios after robot-assisted radical prostatectomy, can we improve quality of life?
Friday, May 13, 2022
2:45 PM – 4:00 PM
Location: Room 222
Theodoros Karagiotis*, Jorn H. Witt, Mikolaj Mendrek, Christian Wagner, Andreas Schuette, Nikolaos Liakos, Pawel Rachubinski, Katarina Urbanova, Matthias Oelke, Sami-Ramzi Leyh-Bannurah, Gronau, Germany
- TK
Poster Presenter(s)
Introduction: The perceived quality-of-life (QoL) of patient-centric robot-assisted radical prostatectomy (RARP) “best-case scenarios” is largely unexplored, since such best-case scenarios often rely on specific combinations of pathological, perioperative, functional and oncological outcome. The aim of this study was to assess meaningful changes of QoL before and after RARP based on patient reported outcomes (PROM) measured with the EORTC QLQ-C30 questionnaire.
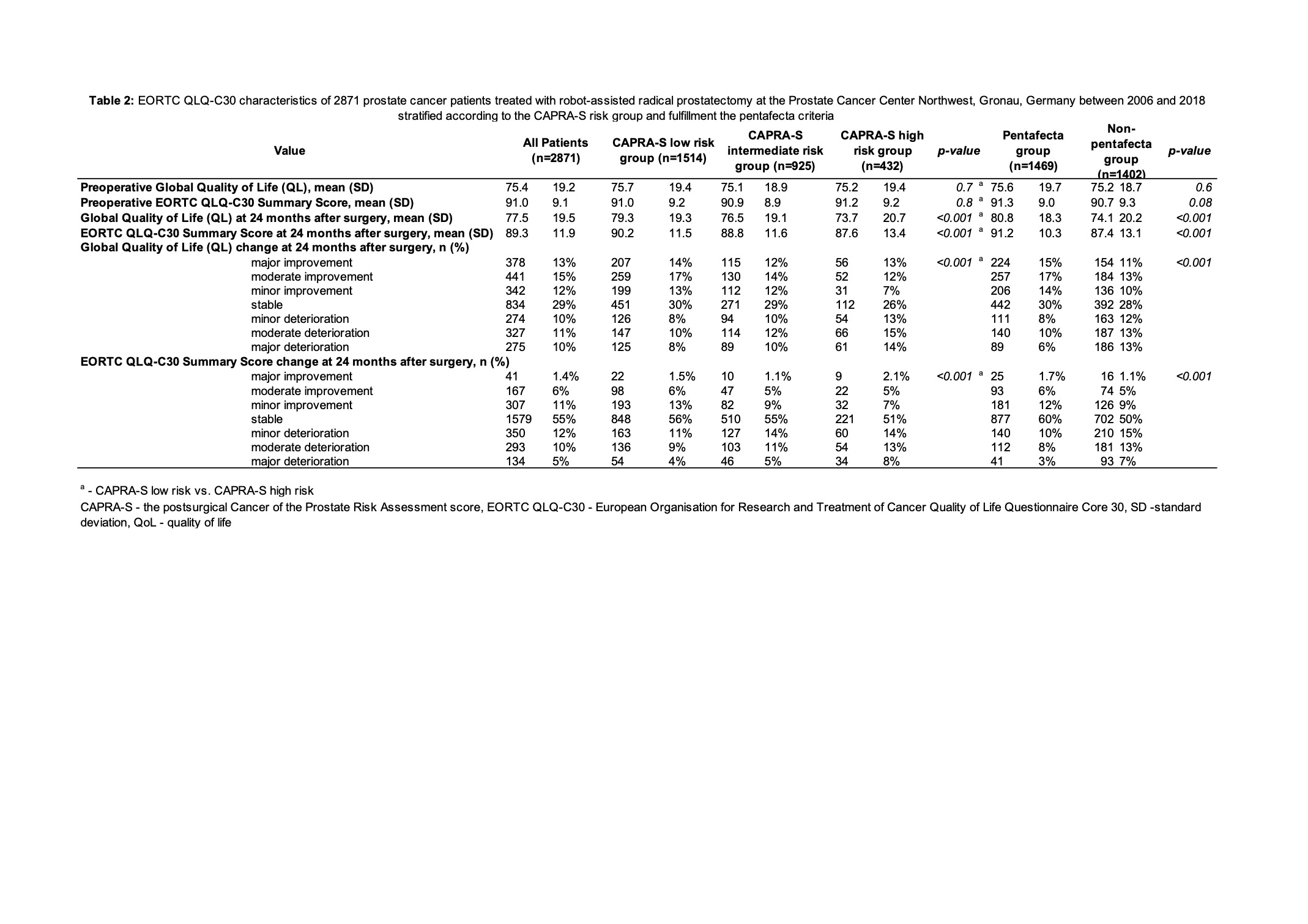
Methods: Overall, 2871 prostate cancer (PCa) patients with completed EORTC QLQ-C30 at baseline and 24 months after surgery were stratified based on postsurgical Cancer of the Prostate Risk Assessment score (CAPRA-S) and 24-months pentafecta criteria. These consist of potency, urinary continence, no biochemical recurrence, negative surgical margins and Clavien-Dindo classified complications =3a. Multivariable logistic regression analyses (LRM) aimed to predict improvement and absence of deterioration for all core EORTC constructs.
Results: Mean preoperative QoL values did not statistically significantly differ between
CAPRA-S low- (LR) vs. high-risk (HR) (75.7, SD 19.4 vs. 75.2, SD 19.4; p=0.7) and pentafecta vs. non-pentafecta groups (75.6, SD 19.7 vs. 75.2, SD 18.7; p=0.6). For CAPRA-S LR vs. HR at 24 months post-RARP, global QoL remained stable in 30 vs. 26% and further improved in 44 vs. 32%. For pentafecta vs. non-pentafecta group, observations were similar with 30 vs. 28% and 47 vs. 34 % (p < 0.001). In LRM, higher preoperative score (OR 0.94, 95% CI 0.93-0.94; p<0.001), higher risk group of CAPRA-S (HR vs. LR [REF] OR 0.60, 95% CI 0.46-0.78; p<0.001) as well as 90d surgical complications (CDC =3b vs. 0-3a [REF] OR 0.49, 95% CI 0.24-0.99; p=0.048) were associated with lower chance of improved QoL. Conversely, fulfilment of trifecta criteria was associated with a double increased chance of improved QoL (OR 1.91, 95% CI 1.59-2.29; p<0.001).
Conclusions: Pathological, perioperative and postoperative measurements are key-elements of health-related quality of life. Our results strongly indicate great potential to improve post-treatment rehabilitation by implementation of PROM tools in cancer survivorship monitoring systems, which in turn may lead to better outcomes.
Source of Funding: Open Access funding enabled and organized by Projekt DEAL. We acknowledge support from the University of Muenster.
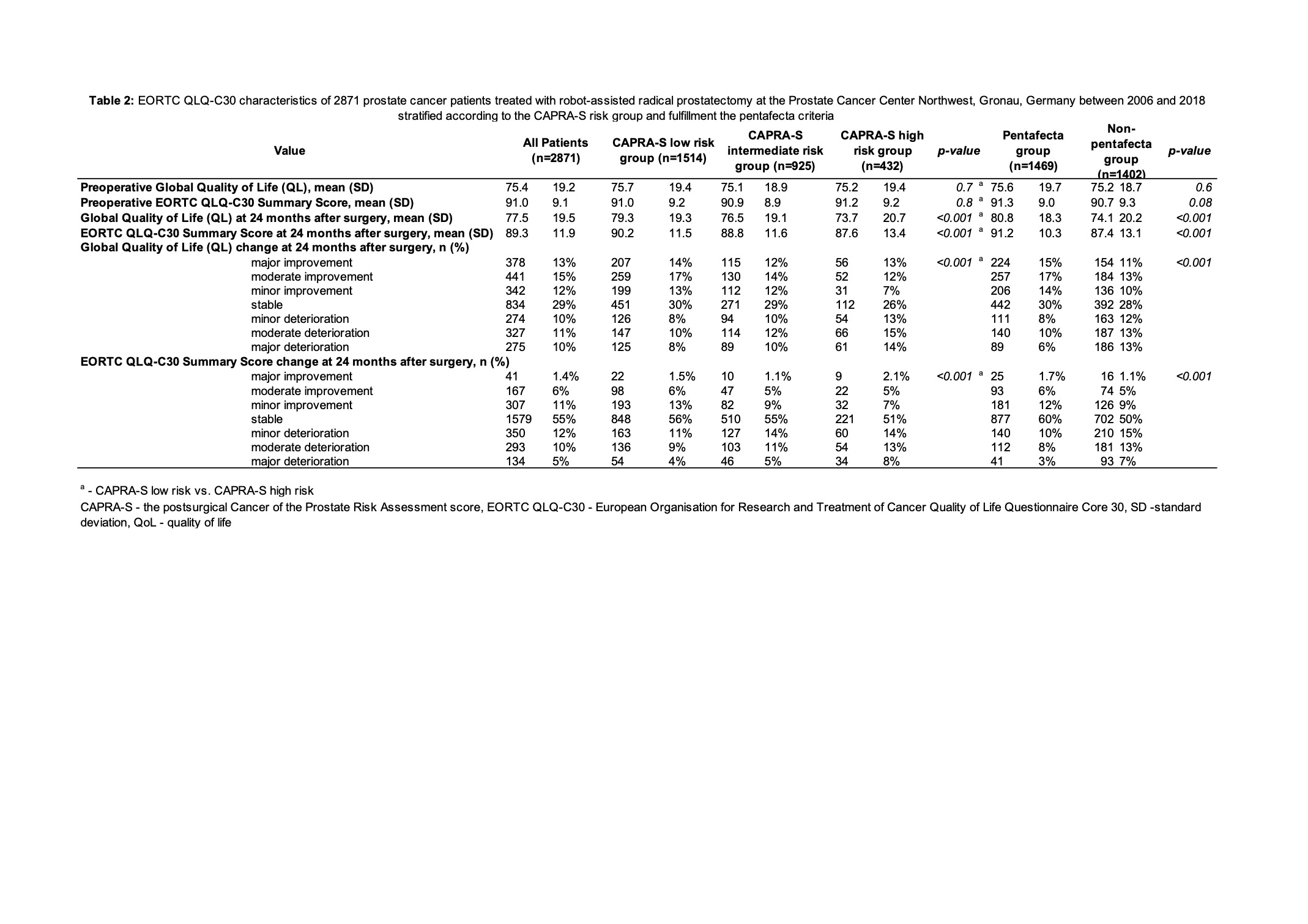
Methods: Overall, 2871 prostate cancer (PCa) patients with completed EORTC QLQ-C30 at baseline and 24 months after surgery were stratified based on postsurgical Cancer of the Prostate Risk Assessment score (CAPRA-S) and 24-months pentafecta criteria. These consist of potency, urinary continence, no biochemical recurrence, negative surgical margins and Clavien-Dindo classified complications =3a. Multivariable logistic regression analyses (LRM) aimed to predict improvement and absence of deterioration for all core EORTC constructs.
Results: Mean preoperative QoL values did not statistically significantly differ between
CAPRA-S low- (LR) vs. high-risk (HR) (75.7, SD 19.4 vs. 75.2, SD 19.4; p=0.7) and pentafecta vs. non-pentafecta groups (75.6, SD 19.7 vs. 75.2, SD 18.7; p=0.6). For CAPRA-S LR vs. HR at 24 months post-RARP, global QoL remained stable in 30 vs. 26% and further improved in 44 vs. 32%. For pentafecta vs. non-pentafecta group, observations were similar with 30 vs. 28% and 47 vs. 34 % (p < 0.001). In LRM, higher preoperative score (OR 0.94, 95% CI 0.93-0.94; p<0.001), higher risk group of CAPRA-S (HR vs. LR [REF] OR 0.60, 95% CI 0.46-0.78; p<0.001) as well as 90d surgical complications (CDC =3b vs. 0-3a [REF] OR 0.49, 95% CI 0.24-0.99; p=0.048) were associated with lower chance of improved QoL. Conversely, fulfilment of trifecta criteria was associated with a double increased chance of improved QoL (OR 1.91, 95% CI 1.59-2.29; p<0.001).
Conclusions: Pathological, perioperative and postoperative measurements are key-elements of health-related quality of life. Our results strongly indicate great potential to improve post-treatment rehabilitation by implementation of PROM tools in cancer survivorship monitoring systems, which in turn may lead to better outcomes.
Source of Funding: Open Access funding enabled and organized by Projekt DEAL. We acknowledge support from the University of Muenster.

.jpg)
.jpg)