Back
Poster, Podium & Video Sessions
Moderated Poster
MP16: Health Services Research: Quality Improvement & Patient Safety I
MP16-01: Effect of surgery-specific financial incentive on opioid prescribing practices: Outcomes of a statewide surgical collaborative
Friday, May 13, 2022
4:30 PM – 5:45 PM
Location: Room 228
John Michael DiBianco*, Stephanie Daignault-Newton, Bronson Conrado, Ann Arbor, MI, David Wenzler, Royal Oak, MI, Hector Pimentel, Grand Rapids, MI, S. Mohammad Jafri, Royal Oak, MI, Rebn Frontera, Rochester Hills, MI, Jessica Phelps, John Hollingsworth, Khurshid R. Ghani, Casey A. Dauw, for the Michigan Urological Surgery Improvement Collaborative, Ann Arbor, MI
.jpg)
John M. Dibianco, MD
University of Michigan
Poster Presenter(s)
Introduction: Reducing unnecessary opioid prescriptions after ureteroscopy (URS) has been advocated. The Michigan Pain Optimization Pathway (MPOP) was a payor initiative begun in 7/2019 funded by Blue Cross Blue Shield of Michigan that provided a 35% increased reimbursement to urologists if no opioids were prescribed after URS. It is unknown how financial incentives effect opioid prescribing practices after ambulatory URS. We therefore aimed to understand the effect of this statewide financial incentive on opioid prescribing after URS as compared to shockwave lithotripsy (SWL) where no such incentive was in place.
Methods: Using the Michigan Urological Surgery Improvement Collaborative (MUSIC) registry we identified all SWL and URS cases from 2018-2020. We separated cases by date with January 2018 - June 2019 as pre-MPOP and July 2019 - December 2020 as post-MPOP. We assessed surgeon rates of postoperative opioid prescription by treatment modality. Urologists (N=80) who had performed at least 5 SWL and URS during the study period were included. We compared opioid prescription rates pre- and post-MPOP by modality. Changes were classified as increase, small decrease and large decrease, defined as any rate increase, =20% and >20%, respectively. Change in pre- and post-MPOP opioid rates between SWL and URS paired by surgeon were compared using the signed rank test.
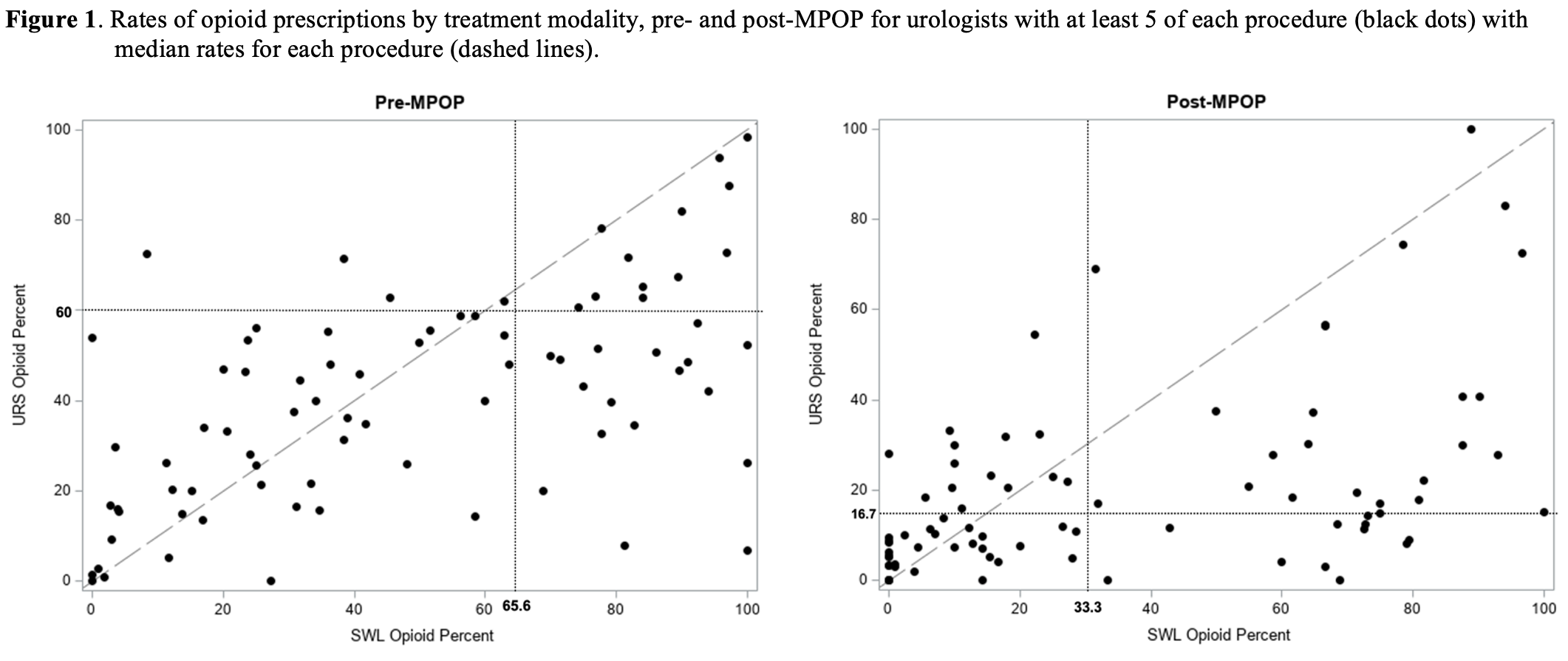
Results: A total of 17,355 cases (5,027 SWL and 12,328 URS) were performed. Rates of opioid prescriptions pre- and post-MPOP after SWL were 64.2% and 45.6% (p < 0.001) and URS were 54.4% and 24.4% (p < 0.001). For SWL, 31% of urologists demonstrated an increase, 39% demonstrated a small decrease, and 30% demonstrated a large decrease. For URS, 16% of urologists demonstrated an increase, 35% demonstrated a small decrease, and 49% demonstrated a large decrease (Figure). Both SWL and URS had a reduction in opioid prescriptions, with urologists reducing their prescribing more for URS than for SWL (p=0.001).
Conclusions: Opioid prescriptions after ambulatory stone surgery decreased over the last 3 years in the state of Michigan. Urologists reduced opioid prescriptions significantly more for URS than SWL, suggesting the benefit of payor incentives to change practice to align with quality improvement.
Source of Funding: Blue Cross Blue Shield of Michigan
Methods: Using the Michigan Urological Surgery Improvement Collaborative (MUSIC) registry we identified all SWL and URS cases from 2018-2020. We separated cases by date with January 2018 - June 2019 as pre-MPOP and July 2019 - December 2020 as post-MPOP. We assessed surgeon rates of postoperative opioid prescription by treatment modality. Urologists (N=80) who had performed at least 5 SWL and URS during the study period were included. We compared opioid prescription rates pre- and post-MPOP by modality. Changes were classified as increase, small decrease and large decrease, defined as any rate increase, =20% and >20%, respectively. Change in pre- and post-MPOP opioid rates between SWL and URS paired by surgeon were compared using the signed rank test.
Results: A total of 17,355 cases (5,027 SWL and 12,328 URS) were performed. Rates of opioid prescriptions pre- and post-MPOP after SWL were 64.2% and 45.6% (p < 0.001) and URS were 54.4% and 24.4% (p < 0.001). For SWL, 31% of urologists demonstrated an increase, 39% demonstrated a small decrease, and 30% demonstrated a large decrease. For URS, 16% of urologists demonstrated an increase, 35% demonstrated a small decrease, and 49% demonstrated a large decrease (Figure). Both SWL and URS had a reduction in opioid prescriptions, with urologists reducing their prescribing more for URS than for SWL (p=0.001).
Conclusions: Opioid prescriptions after ambulatory stone surgery decreased over the last 3 years in the state of Michigan. Urologists reduced opioid prescriptions significantly more for URS than SWL, suggesting the benefit of payor incentives to change practice to align with quality improvement.
Source of Funding: Blue Cross Blue Shield of Michigan

.jpg)
.jpg)