Back
Poster, Podium & Video Sessions
Moderated Poster
MP16: Health Services Research: Quality Improvement & Patient Safety I
MP16-03: Stone Management in the Solitary Kidney, Are We Doing Things Differently? Results from a Statewide Clinical Registry
Friday, May 13, 2022
4:30 PM – 5:45 PM
Location: Room 228
Mohit Butaney*, Detroit, MI, Stephanie Daignault-Newton, Ann Arbor, MI, Isaac Palma-Zamora, Grace Yaguchi, David Leavitt, Detroit, MI, Casey Dauw, Khurshid Ghani, Ann Arbor, MI, Naveen Kachroo, Detroit, MI, for the Michigan Urological Surgery Improvement Collaborative, Ann Arbor, MI
Poster Presenter(s)
Introduction: Stone management in patients with solitary kidneys (SK) is challenging due to the significantly increased morbidity associated with any complication or potential kidney function insult. Given the lack of high quality-evidence to guide optimal management, we sought to assess statewide stone management patterns in SK patients.
Methods: The Michigan Urological Surgery Improvement Collaborative Reducing Operative Complications from Kidney Stones (MUSIC ROCKS) prospective clinical registry was utilized to identify patients with SK from any etiology undergoing either ureteroscopy (URS) or shockwave lithotripsy (SWL) between 2016 and 2021 and compared their management to patients with non-anomalous urinary anatomy (non-SK). Outcomes evaluated included peri-operative management patterns, complication and stone free rates.
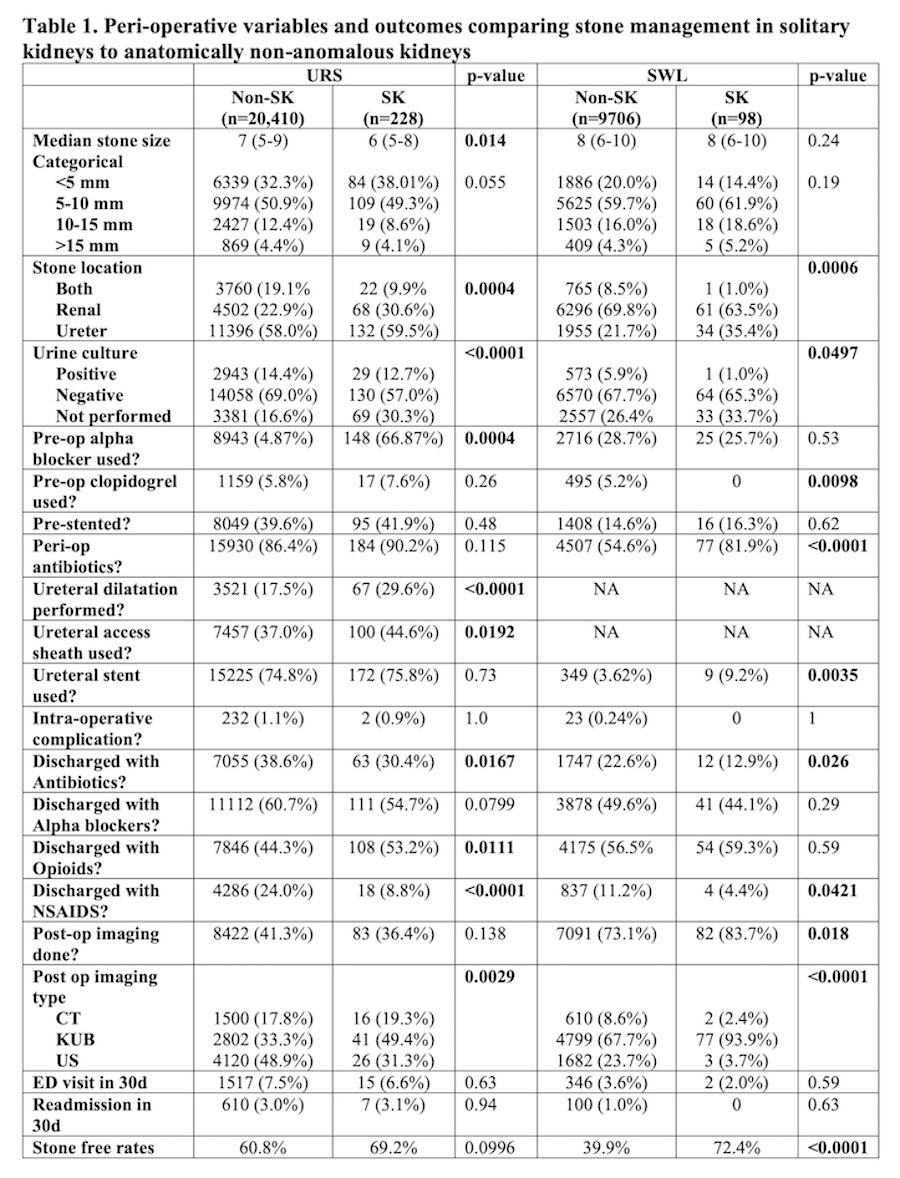
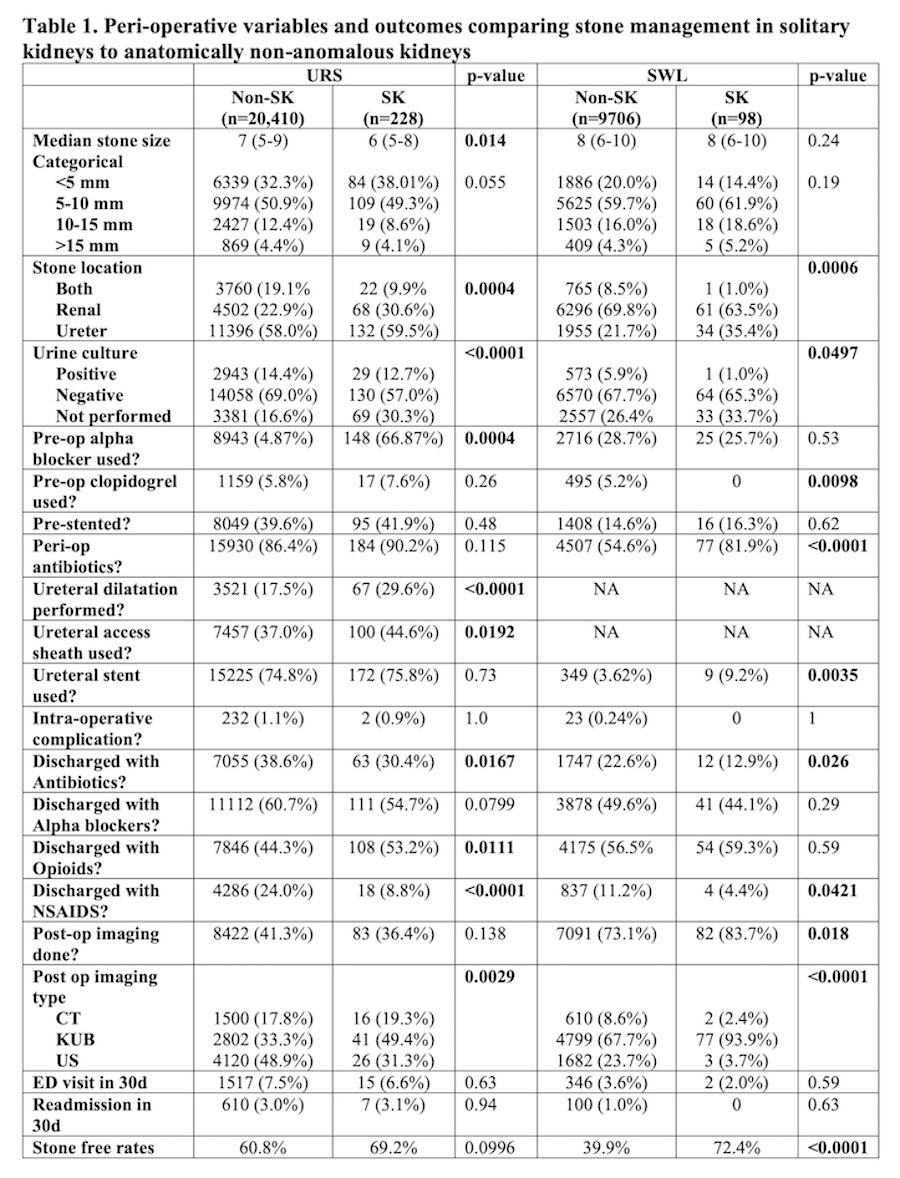
Results: Patients with a SK (n=326) and with non-SK (n=30116) treated for stones were compared. SK patients were older (median age 63 vs 58, p<0.0001) and more likely to have public or no insurance (p < 0.01). SK patients were significantly more likely to not have a pre-op urine culture prior to both URS (30.3% vs 16.6%, p<0.0001) and SWL (33.7% vs 26.4%, p<0.05) but had increased peri-op SWL antibiotic rates (81.9% vs 54.6%, p<0.001). Clopidogrel usage in SK patients completely excluded SWL as a treatment modality. SK patients undergoing URS were more likely to undergo ureteral dilation (p < 0.0001) and ureteral access usage (p=0.02) but had no difference in post-op stent placement (p-0.73). Only 9% of SK patients had a stent placed at time of SWL. SK patients were less likely to be prescribed antibiotics or NSAIDs post URS and SWL but had higher rates of opioids post-URS (Table 1). Significant differences in postoperative imaging rates and modality were noted (Table 1). Stone free rates in SK were significantly higher among SWL (72% vs 40%, p<0.0001) but not among URS patients (69% vs 61%, p=0.10).
Conclusions: We observed significant variation in urolithiasis management for SK patients compared to non-SK patients likely due to lack of specific guidelines. Certain findings in SK patients, the lower pre-op urine culture performance and higher opioid rates in particular, represent opportunities for quality improvement.
Source of Funding: Blue Cross Blue Shield of Michigan
Methods: The Michigan Urological Surgery Improvement Collaborative Reducing Operative Complications from Kidney Stones (MUSIC ROCKS) prospective clinical registry was utilized to identify patients with SK from any etiology undergoing either ureteroscopy (URS) or shockwave lithotripsy (SWL) between 2016 and 2021 and compared their management to patients with non-anomalous urinary anatomy (non-SK). Outcomes evaluated included peri-operative management patterns, complication and stone free rates.
Results: Patients with a SK (n=326) and with non-SK (n=30116) treated for stones were compared. SK patients were older (median age 63 vs 58, p<0.0001) and more likely to have public or no insurance (p < 0.01). SK patients were significantly more likely to not have a pre-op urine culture prior to both URS (30.3% vs 16.6%, p<0.0001) and SWL (33.7% vs 26.4%, p<0.05) but had increased peri-op SWL antibiotic rates (81.9% vs 54.6%, p<0.001). Clopidogrel usage in SK patients completely excluded SWL as a treatment modality. SK patients undergoing URS were more likely to undergo ureteral dilation (p < 0.0001) and ureteral access usage (p=0.02) but had no difference in post-op stent placement (p-0.73). Only 9% of SK patients had a stent placed at time of SWL. SK patients were less likely to be prescribed antibiotics or NSAIDs post URS and SWL but had higher rates of opioids post-URS (Table 1). Significant differences in postoperative imaging rates and modality were noted (Table 1). Stone free rates in SK were significantly higher among SWL (72% vs 40%, p<0.0001) but not among URS patients (69% vs 61%, p=0.10).
Conclusions: We observed significant variation in urolithiasis management for SK patients compared to non-SK patients likely due to lack of specific guidelines. Certain findings in SK patients, the lower pre-op urine culture performance and higher opioid rates in particular, represent opportunities for quality improvement.
Source of Funding: Blue Cross Blue Shield of Michigan

.jpg)
.jpg)
