Back
Poster, Podium & Video Sessions
Moderated Poster
MP16: Health Services Research: Quality Improvement & Patient Safety I
MP16-07: Frailty As a Predictor of Sacral Neuromodulation Outcomes
Friday, May 13, 2022
4:30 PM – 5:45 PM
Location: Room 228
Colby Souders*, Dallas, TX, Mary Enoh Adakama, Riverside, CA, Allison Sih, Seth Cohen, San Francisco, CA, Maude Carmel, Dallas, TX, Jennifer Anger, La Jolla, CA, Karyn Eilber, Los Angeles, CA, Kai Dallas, San Francisco, CA
- CS
Poster Presenter(s)
Introduction: Geriatric patients with overactive bladder or urge incontinence (UUI) are often medically under-treated. Concerns regarding anticholinergic side effects, polypharmacy, and cost of beta-3 agonists result in limited treatment options. Sacral neuromodulation (SNM) is a minimally invasive and non-pharmacological option. Geriatric patients considered frail may not be offered SMN due to concerns of surgery complications, treatment efficacy, and complexity of device operations. Thus, the purpose of this study is to investigate SNM outcomes in geriatric patients who meet frailty criteria.
Methods: We reviewed California Office of Statewide Health Planning and Development (OSHPD) from 1/1/2012-12/31/2018. Using Current Procedural Terminology (CPT) codes, we identified patients who underwent Stage 1 (CPT:64581) and Stage 2 (CPT:64590) SNM surgery. Treatment was considered successful if a patient proceeded to Stage 2 from Stage 1. Patient age, gender, ethnicity, academic status surgery facility, and payor status were obtained. The SNM patient population was then analyzed using a validated claims-based frailty index (Kim, 2018). Univariate (chi-square/ T-test) and multivariate analysis were performed to assess for associations between variables of interest and completion of Stage 2.
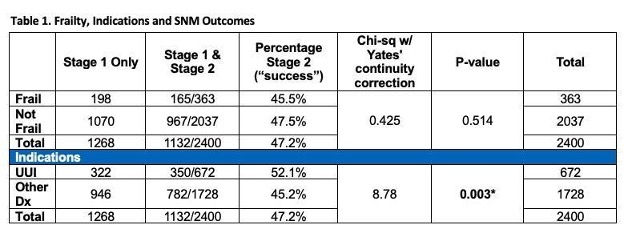
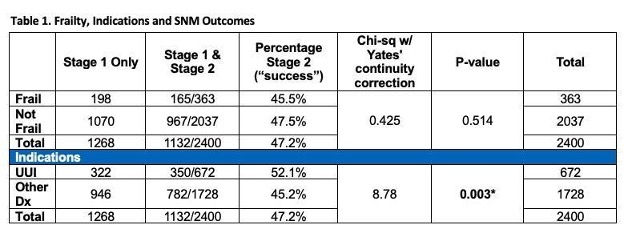
Results: We identified 2,400 patients who underwent Stage 1, and 1,132 patients successfully proceeded to Stage 2. Rates of Stage 2 were higher in females compared to males (36.6% vs. 50.5%, p<0.001), those who had surgery at academic medical centers (58.6% vs. 20.8%, p<0.001), and those with a diagnosis of urgency (52.1% vs. 45.3%, p=0.003). These findings remained significant with multivariate analysis. Of the 2,400 patients identified 363 (15.1%) met frailty criteria and 165 (45.5%) underwent Stage 2. For non-frail patients, SNM success rate was 47.5% (p=0.514) (Table 1). There were no significant associations between patient age, ethnicity, payor status, and completion of Stage 2.
Conclusions: Our work demonstrates that frailty had no significant adverse impact on success of SNM treatment. However, female gender, surgery at an academic center, and a diagnosis of UUI were more likely to have treatment success than patients with other indications. This data supports recommendation of SNM to older, frail patients, especially those with UUI.
Source of Funding: The Medical Student Training in Aging Research Program and the National Institute on Aging (T35AG026736)
Methods: We reviewed California Office of Statewide Health Planning and Development (OSHPD) from 1/1/2012-12/31/2018. Using Current Procedural Terminology (CPT) codes, we identified patients who underwent Stage 1 (CPT:64581) and Stage 2 (CPT:64590) SNM surgery. Treatment was considered successful if a patient proceeded to Stage 2 from Stage 1. Patient age, gender, ethnicity, academic status surgery facility, and payor status were obtained. The SNM patient population was then analyzed using a validated claims-based frailty index (Kim, 2018). Univariate (chi-square/ T-test) and multivariate analysis were performed to assess for associations between variables of interest and completion of Stage 2.
Results: We identified 2,400 patients who underwent Stage 1, and 1,132 patients successfully proceeded to Stage 2. Rates of Stage 2 were higher in females compared to males (36.6% vs. 50.5%, p<0.001), those who had surgery at academic medical centers (58.6% vs. 20.8%, p<0.001), and those with a diagnosis of urgency (52.1% vs. 45.3%, p=0.003). These findings remained significant with multivariate analysis. Of the 2,400 patients identified 363 (15.1%) met frailty criteria and 165 (45.5%) underwent Stage 2. For non-frail patients, SNM success rate was 47.5% (p=0.514) (Table 1). There were no significant associations between patient age, ethnicity, payor status, and completion of Stage 2.
Conclusions: Our work demonstrates that frailty had no significant adverse impact on success of SNM treatment. However, female gender, surgery at an academic center, and a diagnosis of UUI were more likely to have treatment success than patients with other indications. This data supports recommendation of SNM to older, frail patients, especially those with UUI.
Source of Funding: The Medical Student Training in Aging Research Program and the National Institute on Aging (T35AG026736)

.jpg)
.jpg)