Back
Poster, Podium & Video Sessions
Moderated Poster
MP16: Health Services Research: Quality Improvement & Patient Safety I
MP16-08: Major Shift In Antibiotic Prophylaxis Patterns Following Implementation of Guidelines Based Cystoscopy Survey
Friday, May 13, 2022
4:30 PM – 5:45 PM
Location: Room 228
Kelly R. Pekala*, Danielle Sharbaugh, Jonathan G. Yabes, Adam J. Sharbaugh, Michelle Yu, Valentina Grajales, Oluwaseun Orikogbo, Hermoon Worku, Jordan M. Hay, Toby S. Zhu, Kody M. Armann, Chandler N. Hudson, Benjamin J. Davies, Bruce L. Jacobs, Pittsburgh, PA
- KP
Poster Presenter(s)
Introduction: Inappropriate antibiotic administration has a host of well-defined deleterious downstream effects. The American Urological
Association (AUA) released antibiotic guidelines for cystoscopy in June 2019 that recommended oral antibiotics only if there is a break in the mucosal barrier and fluoroquinolones were no longer the antibiotic of choice. As a result, we created a novel clinic-based rapid survey to increase AUA antibiotic guideline adherence.
Methods: To obtain baseline data, we retrospectively reviewed the urology clinic schedule for three-months and identified all patients who underwent cystoscopy. We then completed a literature review and designed a cystoscopy survey based on previous protocols and AUA guidelines to identify patients at high risk of infection. We then implemented a multi-pronged intervention for a twelve-month period where we provided a ‘formal’ grand rounds presentation, ad hoc emails with individual updates, monthly progress reports, edited the electronic health record cystoscopy order set, educated clinic staff, and started using the cystoscopy survey. We then recorded antibiotics given for prophylaxis at time of procedure, individual patient risk factors for infection, 30-day infection outcomes, and urine culture data both pre-intervention and post-intervention.
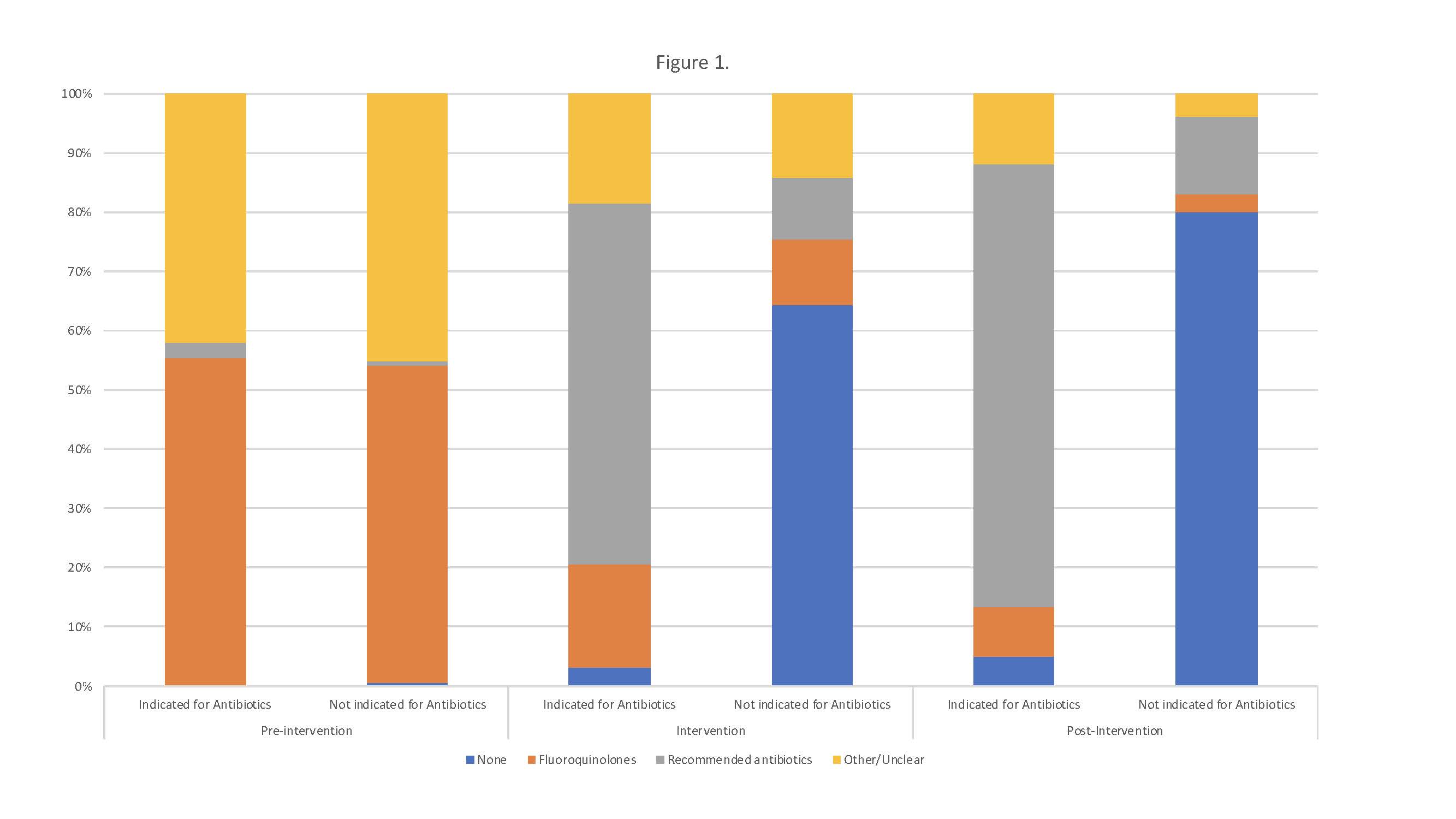
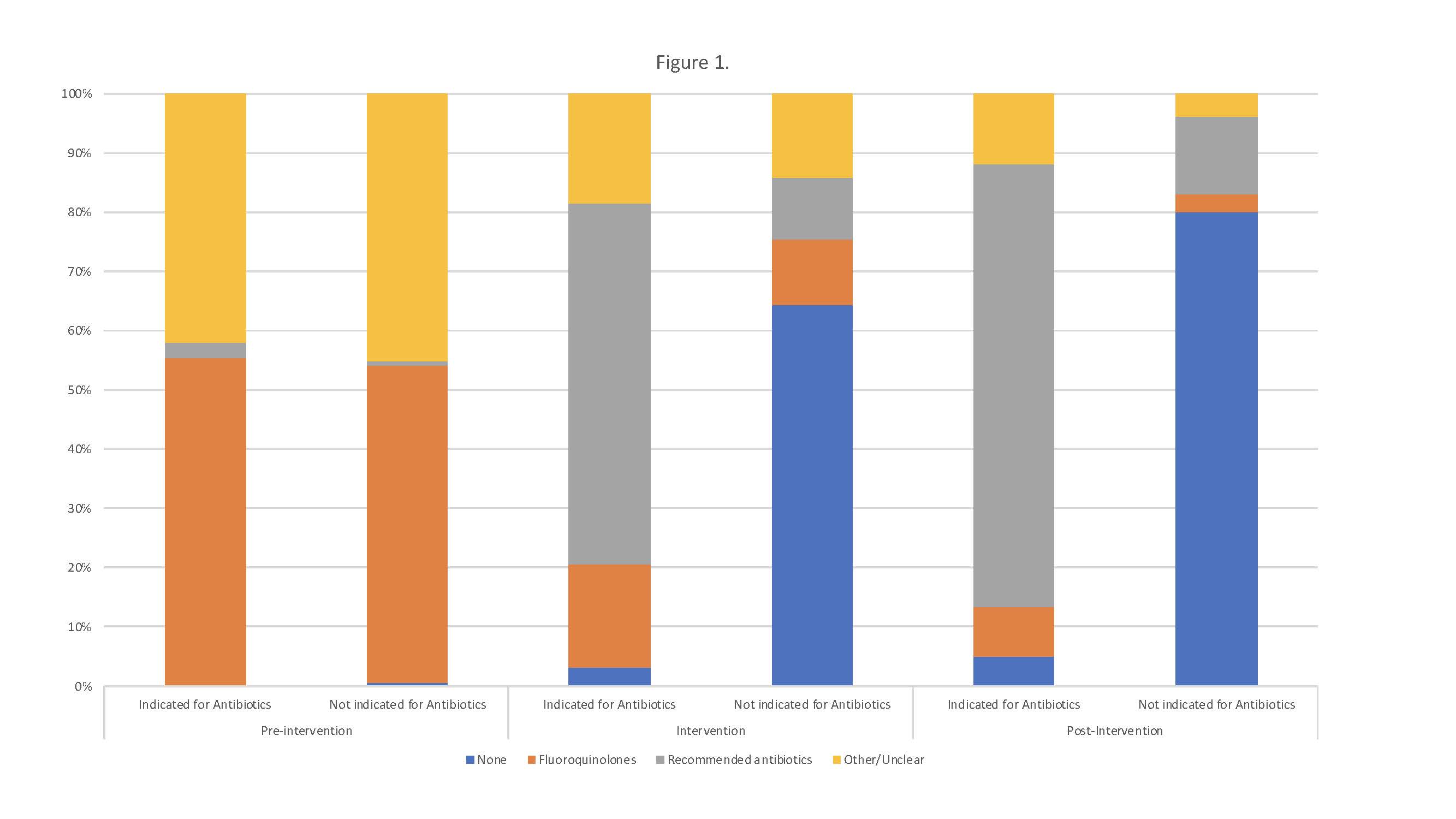
Results: We identified 473 cystoscopies pre-intervention, 2,137 cystoscopies in the intervention, and 417 cystoscopies post-intervention. There was a 30% decrease in the total amount of antibiotics administered and infection rates did not increase. We found that 99% of patients were administered antibiotics pre-intervention, the majority of which were fluoroquinolones. During and after the intervention phase, fluoroquinolone use decreased significantly to 15% and 6.5% respectively. (Figure 1) The utilization rates of recommended antibiotics increased to 91% and persisted post-intervention.
Conclusions: We found that implementation of a cystoscopy survey enabled rapid adoption of new AUA guidelines on antibiotic prophylaxis for cystoscopy, which resulted in a drastic reduction in the amount of antibiotics administered without a spike in infection rates. The use of recommended antibiotics improved dramatically during the intervention period and persisted post-intervention.
Source of Funding: Bruce L. Jacobs, MD, MPH is supported in part by the Shadyside Hospital Foundation.
Association (AUA) released antibiotic guidelines for cystoscopy in June 2019 that recommended oral antibiotics only if there is a break in the mucosal barrier and fluoroquinolones were no longer the antibiotic of choice. As a result, we created a novel clinic-based rapid survey to increase AUA antibiotic guideline adherence.
Methods: To obtain baseline data, we retrospectively reviewed the urology clinic schedule for three-months and identified all patients who underwent cystoscopy. We then completed a literature review and designed a cystoscopy survey based on previous protocols and AUA guidelines to identify patients at high risk of infection. We then implemented a multi-pronged intervention for a twelve-month period where we provided a ‘formal’ grand rounds presentation, ad hoc emails with individual updates, monthly progress reports, edited the electronic health record cystoscopy order set, educated clinic staff, and started using the cystoscopy survey. We then recorded antibiotics given for prophylaxis at time of procedure, individual patient risk factors for infection, 30-day infection outcomes, and urine culture data both pre-intervention and post-intervention.
Results: We identified 473 cystoscopies pre-intervention, 2,137 cystoscopies in the intervention, and 417 cystoscopies post-intervention. There was a 30% decrease in the total amount of antibiotics administered and infection rates did not increase. We found that 99% of patients were administered antibiotics pre-intervention, the majority of which were fluoroquinolones. During and after the intervention phase, fluoroquinolone use decreased significantly to 15% and 6.5% respectively. (Figure 1) The utilization rates of recommended antibiotics increased to 91% and persisted post-intervention.
Conclusions: We found that implementation of a cystoscopy survey enabled rapid adoption of new AUA guidelines on antibiotic prophylaxis for cystoscopy, which resulted in a drastic reduction in the amount of antibiotics administered without a spike in infection rates. The use of recommended antibiotics improved dramatically during the intervention period and persisted post-intervention.
Source of Funding: Bruce L. Jacobs, MD, MPH is supported in part by the Shadyside Hospital Foundation.

.jpg)
.jpg)