Back

(80) Syringe Exchange Services in Primary Care
Saturday, April 2, 2022
10:00 AM – 11:30 AM ET
Location: Great Hall Foyer, Third Floor
Has Audio

Paula J. Cook, MD, DFASAM
Faculty physician
Utah Healthcare Institute, Utah- CO
Corey Orndorff, BSc
Community Healthcare worker, Harm Reduction Navigator
AmeriCorp, Utah
Presenter(s)
Introduction / Background
Syringe exchange programs (SEPs) have the ability to reduce transmission of blood borne infections like HIV and HCV by 50% in people who inject drugs (PWIDs)1. Free access to syringe exchange services also has the potential to reduce skin and soft tissue infections, costs of hospitalizations for serious infections like bacterial endocarditis, and emergency room visits in this population2,3. Furthermore, PWIDs who engage in syringe exchange are five times more likely to engage in treatment for substance use disorder4,5. SEPs typically exist as outreach programs, with some programs offering wound care and rapid HCV and HIV testing, and most offering linkage to substance use disorder treatment. Primary care clinics who treat PWIDs are well suited to offer syringe exchange services, with the advantage of onsite availability of medical services including HCV treatment, PrEP/PEP, STI testing and treatment, and medications for opioid use disorder (MOUD).
Methods
In one primary care clinic with a large population of PWIDs, an expanded syringe exchange harm reduction model was initiated and combined with rapid access to MOUD. Syringe exchange services became available for walk-in community participants and existing patients during regular clinic hours. Novel services at the clinic during the project period included distribution of sterile syringes and injection materials, disposal of used syringes, naloxone kits for overdose reversal, fentanyl test strips, personal sharps containers, wound care supplies, and safer sex supplies, as well as education and referrals.
Results
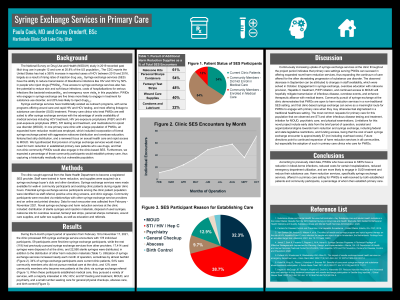
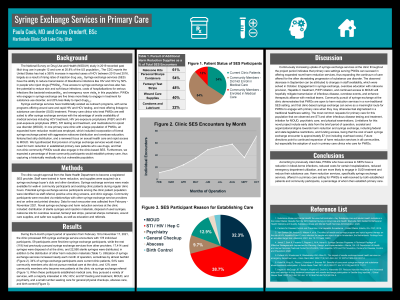
Data for each encounter was collected from February - November 2021. During the period of operation, the clinic processed 355 syringe exchange service encounters with 178 individual participants. 59 participants were first-time syringe exchange participants, while the rest (119) had previously pursued syringe exchange services from other providers. 17,414 used syringes were disposed of at the clinic, and 22,590 sterile syringes were distributed, in addition to the distribution of other harm reduction materials. Utilization of syringe exchange services increased nearly each month of operation, sometimes by almost twofold. 34% of syringe exchange participants were current clinic patients, 54% were community members who did not pursue medical care, and 12% were community members who became new patients at the clinic via syringe exchange referral. When these participants established medical care, they pursued a variety of services, with a majority interested in HIV, HCV, and STI testing and treatment, MOUD, and psychiatry, and a small number seeking care for general physical checkups, abscess care, and birth control.
Conclusions / Discussion
Continuously increasing uptake of syringe exchange services at the clinic indicates that primary care settings serving PWIDs can succeed in offering expanded novel harm reduction services, thus expanding the continuum of care offered for the often devastating progression of substance use disorder. Engagement in syringe exchange, overdose education with naloxone provision, Hepatitis C treatment, PrEP initiation, and continued access to MOUD will hopefully mitigate transmission of infectious disease, overdose events, and enhance therapeutic alliance with medical teams. Community pursuit of syringe exchange at the clinic demonstrates that PWIDs are open to harm reduction services in a non-traditional SEP setting, and that clinic-based syringe exchange can serve as a meaningful route for PWIDs to engage with primary care when they may otherwise feel stigmatized in a traditional healthcare setting.
References
1. van Santen DK, Anders B, Matser A, et al. The effect of needle and syringe program and opioid agonist therapy on the risk of HIV, hepatitis B and C virus infection for people who inject drugs in Amsterdam, the Netherlands: Findings from an emulated target trial. Addiction. 2021. doi: 10.1111/add.15503.
2. Javed Z, Burk K, Facente S, Pegram L, Ali A, Asher A. Syringe Services Programs: A Technical Package of Effective Strategies and Approaches for Planning, Design, and Implementation. Atlanta, GA: US Department of Health and Human Services, National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention, Centers for Disease, Control and Prevention; 2020.
3. Pollack HA, Khoshnood K, Blankenship KM, Altice FL. The impact of needle exchange-based health services on emergency department use. J Gen Intern Med. 2002;17(5):341–348. doi: 10.1007/s11606-002-0037-2.
4. Kidorf M, King VL, Pierce J, Kolodner K, Brooner RK. Benefits of concurrent syringe exchange and substance abuse treatment participation. J Subst Abuse Treat. 2011;40(3):265-271. doi:10.1016/j.jsat.2010.11.011
5. Hagan H, McGough JP, Thiede H, Hopkins S, Duchin J, Alexander ER. Reduced injection frequency and increased entry and retention in drug treatment associated with needle-exchange participation in Seattle drug injectors. J Subst Abuse Treat. 2000;19(3):247-52. doi: 10.1016/s0740-5472(00)00104-5.
Diversity, Equity, and Inclusion:
Underserved patients who continue to use drugs and who do not access health care due to multiple systemic and individual healthcare disparities are at increased risk of secondary and tertiary disease states. Participants in traditional syringe exchange programs are often from diverse backgrounds with higher levels of socioeconomic stress, incarceration and poverty. Our study addressed the need for increased access to harm reduction services in a traditional medical setting to allow for expanded on-site medical, psychiatric and addiction treatment availability. Our study and program aims to be inclusive regardless of social background, ethnicity, socioeconomic status, drug use status and readiness to change.
Syringe exchange programs (SEPs) have the ability to reduce transmission of blood borne infections like HIV and HCV by 50% in people who inject drugs (PWIDs)1. Free access to syringe exchange services also has the potential to reduce skin and soft tissue infections, costs of hospitalizations for serious infections like bacterial endocarditis, and emergency room visits in this population2,3. Furthermore, PWIDs who engage in syringe exchange are five times more likely to engage in treatment for substance use disorder4,5. SEPs typically exist as outreach programs, with some programs offering wound care and rapid HCV and HIV testing, and most offering linkage to substance use disorder treatment. Primary care clinics who treat PWIDs are well suited to offer syringe exchange services, with the advantage of onsite availability of medical services including HCV treatment, PrEP/PEP, STI testing and treatment, and medications for opioid use disorder (MOUD).
Methods
In one primary care clinic with a large population of PWIDs, an expanded syringe exchange harm reduction model was initiated and combined with rapid access to MOUD. Syringe exchange services became available for walk-in community participants and existing patients during regular clinic hours. Novel services at the clinic during the project period included distribution of sterile syringes and injection materials, disposal of used syringes, naloxone kits for overdose reversal, fentanyl test strips, personal sharps containers, wound care supplies, and safer sex supplies, as well as education and referrals.
Results
Data for each encounter was collected from February - November 2021. During the period of operation, the clinic processed 355 syringe exchange service encounters with 178 individual participants. 59 participants were first-time syringe exchange participants, while the rest (119) had previously pursued syringe exchange services from other providers. 17,414 used syringes were disposed of at the clinic, and 22,590 sterile syringes were distributed, in addition to the distribution of other harm reduction materials. Utilization of syringe exchange services increased nearly each month of operation, sometimes by almost twofold. 34% of syringe exchange participants were current clinic patients, 54% were community members who did not pursue medical care, and 12% were community members who became new patients at the clinic via syringe exchange referral. When these participants established medical care, they pursued a variety of services, with a majority interested in HIV, HCV, and STI testing and treatment, MOUD, and psychiatry, and a small number seeking care for general physical checkups, abscess care, and birth control.
Conclusions / Discussion
Continuously increasing uptake of syringe exchange services at the clinic indicates that primary care settings serving PWIDs can succeed in offering expanded novel harm reduction services, thus expanding the continuum of care offered for the often devastating progression of substance use disorder. Engagement in syringe exchange, overdose education with naloxone provision, Hepatitis C treatment, PrEP initiation, and continued access to MOUD will hopefully mitigate transmission of infectious disease, overdose events, and enhance therapeutic alliance with medical teams. Community pursuit of syringe exchange at the clinic demonstrates that PWIDs are open to harm reduction services in a non-traditional SEP setting, and that clinic-based syringe exchange can serve as a meaningful route for PWIDs to engage with primary care when they may otherwise feel stigmatized in a traditional healthcare setting.
References
1. van Santen DK, Anders B, Matser A, et al. The effect of needle and syringe program and opioid agonist therapy on the risk of HIV, hepatitis B and C virus infection for people who inject drugs in Amsterdam, the Netherlands: Findings from an emulated target trial. Addiction. 2021. doi: 10.1111/add.15503.
2. Javed Z, Burk K, Facente S, Pegram L, Ali A, Asher A. Syringe Services Programs: A Technical Package of Effective Strategies and Approaches for Planning, Design, and Implementation. Atlanta, GA: US Department of Health and Human Services, National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention, Centers for Disease, Control and Prevention; 2020.
3. Pollack HA, Khoshnood K, Blankenship KM, Altice FL. The impact of needle exchange-based health services on emergency department use. J Gen Intern Med. 2002;17(5):341–348. doi: 10.1007/s11606-002-0037-2.
4. Kidorf M, King VL, Pierce J, Kolodner K, Brooner RK. Benefits of concurrent syringe exchange and substance abuse treatment participation. J Subst Abuse Treat. 2011;40(3):265-271. doi:10.1016/j.jsat.2010.11.011
5. Hagan H, McGough JP, Thiede H, Hopkins S, Duchin J, Alexander ER. Reduced injection frequency and increased entry and retention in drug treatment associated with needle-exchange participation in Seattle drug injectors. J Subst Abuse Treat. 2000;19(3):247-52. doi: 10.1016/s0740-5472(00)00104-5.
Diversity, Equity, and Inclusion:
Underserved patients who continue to use drugs and who do not access health care due to multiple systemic and individual healthcare disparities are at increased risk of secondary and tertiary disease states. Participants in traditional syringe exchange programs are often from diverse backgrounds with higher levels of socioeconomic stress, incarceration and poverty. Our study addressed the need for increased access to harm reduction services in a traditional medical setting to allow for expanded on-site medical, psychiatric and addiction treatment availability. Our study and program aims to be inclusive regardless of social background, ethnicity, socioeconomic status, drug use status and readiness to change.
