Back

Introduction: Opioid use disorder (OUD) has been documented to impose significant financial burden on state Medicaid programs (1). Additionally, it has been found that non-OUD treatment has been a major driver of healthcare costs for Medicaid enrollees with OUD (1). The OUD care continuum has identified linkage to ongoing treatment as an important step in patient engagement (2). Although medication for OUD (MOUD) has been associated with favorable health outcomes for individuals experiencing OUD (3), we do not know how linkage to ongoing MOUD treatment impacts the overall healthcare cost of these individuals. In this analysis, we investigate the impact of linkage to continual MOUD treatment on overall healthcare costs of Medicaid Fee-for-Service enrollees who have started MOUD treatment.
Methods: This was a retrospective study using Medicaid claims data of individuals experiencing OUD and receiving treatment at Denver Health, a safety net urban healthcare system, during the year 2020. We examined the association between their healthcare costs and linkage to care after receiving first dose of MOUD. Our outcome variable was per-member per-month (PMPM) healthcare cost of the Medicaid Fee-For-Service attributed enrollees in our cohort. Primary independent variable was whether the individuals was linked to MOUD treatment after starting MOUD at Denver Health. We also gather information about their age, sex and race/ethnicity. Multivariable generalized linear model (GLM) with log link and gamma distribution was used to empirically test this association.
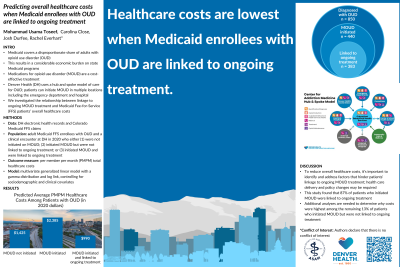
Results: A total of 458 Medicaid FFS enrollees were identified who received MOUD at Denver Health in 2020. Linkage to care was achieved for 398 individuals while 60 were not linked to care. No significant differences were observed between these two groups based on age, race/ethnicity and sex. Results from our GLM showed that PMPM cost of those linked to care is 55.5% lower as compared to those who are not linked to care. The predicted mean cost from our model for those linked to care is $1118.47 (p < 0.01) lower than for those who are not linked to care.
Conclusion: Linkage to ongoing care after initiating MOUD treatment has a significant impact on reducing the healthcare costs for Medicaid FFS enrollees experiencing OUD.
References:
References:
1) Leslie, D. L., Ba, D. M., Agbese, E., Xing, X., & Liu, G. (2019). The economic burden of the opioid epidemic on states: the case of Medicaid. Am J Manag Care, 25(13 Suppl), S243-S249.
2) Prieto J. T., McEwen D., Davidson A. J., et al. (2019). Monitoring opioid addiction and treatment: Do you know if your population is engaged?. Drug Alcohol Depend, 202:56‐60. doi:10.1016/j.drugalcdep.2019.07.002.
3) Williams, A. R., Nunes, E. V., Bisaga, A., Levin, F. R., & Olfson, M. (2019). Development of a cascade of care for responding to the opioid epidemic. The American journal of drug and alcohol abuse, 45(1), 1-10.
Diversity, Equity, and Inclusion: The cohort of our analysis received its medication for opioid use disorder (MOUD) at an urban safety-net institution that caters to a diverse population. In our presentation, we will present and discuss how linkage to MOUD treatment differs across age groups, sex, and race/ethnicity within our cohort at the healthcare system.
(42) Association Between Healthcare Costs and MOUD Treatment Linkage for Medicaid FFS Enrollees
Friday, April 1, 2022
11:30 AM – 1:00 PM ET
Location: Great Hall Foyer, Third Floor
Has Audio

Mohammad Usama Toseef, PhD
Prevention Effectiveness Fellow
Public Health Institute at Denver Health, Colorado- JD
Josh Durfee, MSPH
Biostatistics Manager
Denver Health, Colorado - RE
Rachel Everhart, PhD, MS
Director of Research
Denver Health, Colorado
Presenter(s)
Non-presenting author(s)
Introduction: Opioid use disorder (OUD) has been documented to impose significant financial burden on state Medicaid programs (1). Additionally, it has been found that non-OUD treatment has been a major driver of healthcare costs for Medicaid enrollees with OUD (1). The OUD care continuum has identified linkage to ongoing treatment as an important step in patient engagement (2). Although medication for OUD (MOUD) has been associated with favorable health outcomes for individuals experiencing OUD (3), we do not know how linkage to ongoing MOUD treatment impacts the overall healthcare cost of these individuals. In this analysis, we investigate the impact of linkage to continual MOUD treatment on overall healthcare costs of Medicaid Fee-for-Service enrollees who have started MOUD treatment.
Methods: This was a retrospective study using Medicaid claims data of individuals experiencing OUD and receiving treatment at Denver Health, a safety net urban healthcare system, during the year 2020. We examined the association between their healthcare costs and linkage to care after receiving first dose of MOUD. Our outcome variable was per-member per-month (PMPM) healthcare cost of the Medicaid Fee-For-Service attributed enrollees in our cohort. Primary independent variable was whether the individuals was linked to MOUD treatment after starting MOUD at Denver Health. We also gather information about their age, sex and race/ethnicity. Multivariable generalized linear model (GLM) with log link and gamma distribution was used to empirically test this association.
Results: A total of 458 Medicaid FFS enrollees were identified who received MOUD at Denver Health in 2020. Linkage to care was achieved for 398 individuals while 60 were not linked to care. No significant differences were observed between these two groups based on age, race/ethnicity and sex. Results from our GLM showed that PMPM cost of those linked to care is 55.5% lower as compared to those who are not linked to care. The predicted mean cost from our model for those linked to care is $1118.47 (p < 0.01) lower than for those who are not linked to care.
Conclusion: Linkage to ongoing care after initiating MOUD treatment has a significant impact on reducing the healthcare costs for Medicaid FFS enrollees experiencing OUD.
References:
References:
1) Leslie, D. L., Ba, D. M., Agbese, E., Xing, X., & Liu, G. (2019). The economic burden of the opioid epidemic on states: the case of Medicaid. Am J Manag Care, 25(13 Suppl), S243-S249.
2) Prieto J. T., McEwen D., Davidson A. J., et al. (2019). Monitoring opioid addiction and treatment: Do you know if your population is engaged?. Drug Alcohol Depend, 202:56‐60. doi:10.1016/j.drugalcdep.2019.07.002.
3) Williams, A. R., Nunes, E. V., Bisaga, A., Levin, F. R., & Olfson, M. (2019). Development of a cascade of care for responding to the opioid epidemic. The American journal of drug and alcohol abuse, 45(1), 1-10.
Diversity, Equity, and Inclusion: The cohort of our analysis received its medication for opioid use disorder (MOUD) at an urban safety-net institution that caters to a diverse population. In our presentation, we will present and discuss how linkage to MOUD treatment differs across age groups, sex, and race/ethnicity within our cohort at the healthcare system.
