Back

Poster Session
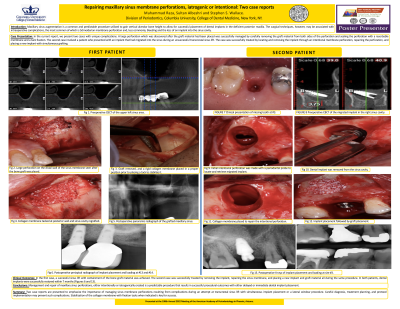
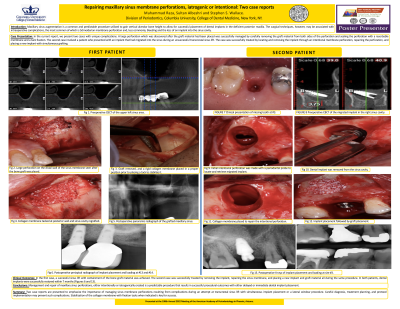
(32) Repairing maxillary sinus membrane perforations, iatrogenic or intentional: Two case reports
Has Audio

Muhammad Raza, BDS, DDS, MS.
Section Chief Periodontology
Jamaica Hospital Medical Center
Hicksville, New York, United States
Lead Author(s)
Introduction: Over the last 50 years, implant-supported restorations have become a proven treatment modality. Sinus membrane elevation has become a predictable pre-prosthetic surgical procedure for implant site preparation in the posterior maxilla. Lifting the Schneiderian membrane can
be achieved internally (indirectly) by many transcrestal techniques or externally (directly) by a lateral window approach. As with any other surgical procedures, several intraoperative complications may occur with this technique. The most common complication is Schneiderian membrane perforation. The average perforation rate with rotary instrumentation is 20%–25%. The perforation rate is reduced from the average reported rate of 30% to 7% with Piezoelectric instrumentation. In a study by Wallace et al found perforations with the piezoelectric technique occurred during the hand instrumentation phase and not with the piezoelectric inserts. The most common clinical risk factors are the presence of septa and secondly, the presence of a thin membrane. Management of perforations is dependent upon the size, location, and extent of the perforation.
Methods: Patient 1
The first patient is a 56-year-old Caucasian male referred from the undergraduate clinic to the Postdoctoral Clinic at Columbia University, with the chief complaint of missing teeth on the upper left side. He is otherwise medically healthy and is a non-smoker. Clinical and radiographic
(CBCT) examinations highlighted a vertical and horizontal ridge deficiency, missing teeth #’s 13–15, pneumatization of the maxillary sinus and the presence of an anterior and a posterior septum (Figure 1). After anesthesia, a paracrestal incision with anterior and posterior verticals was made sparing the distal papilla of #12.A full thickness mucoperiosteal flap was elevated and an antrostomy of 15 × 20 mm oval shape was made about 3 mm above the sinus floor utilizing a piezoelectric device. Despite the precautions taken, a 9×7 mm perforation occurred on the distal aspect while the graft material was being placed (Figure 2). In order to avoid a second surgical procedure, the complication was addressed by removing the graft material from both sides of the perforation, followed by repair of the perforation with a large, rigid, cross-linked, and slowly resorbing collagen membrane with the dimensions of 20 × 30 mm. The membrane was made long enough to reach the medial wall to prevent the displacement
of bone graft into the posterior cavity (Figure 3). One sinus. A second resorbable membrane was placed over the antrostomy. Closure was achieved with a combination of horizontal mattress and interrupted synthetic resorbable sutures. A postoperative panoramic radiograph showed a well contained graft (Figure 5).
Results: In the first case, a successful sinus lift with containment of the bone graft material was achieved. The second case was successfully treated by removing the implant, repairing the sinus membrane, and placing a new implant and graft material all during the same procedure. In both patients, dental implants were successfully restored within 7 months (Figures 6 and 14).
Conclusions: Management and repair of maxillary sinus perforations, either intentionally or iatrogenically created is a predictable procedure that results in successful procedural outcomes with either delayed or immediate dental implant placement.
Lead Author’s Contributions to the Research Project: I performed the surgeries at Columbia University during my residency.
be achieved internally (indirectly) by many transcrestal techniques or externally (directly) by a lateral window approach. As with any other surgical procedures, several intraoperative complications may occur with this technique. The most common complication is Schneiderian membrane perforation. The average perforation rate with rotary instrumentation is 20%–25%. The perforation rate is reduced from the average reported rate of 30% to 7% with Piezoelectric instrumentation. In a study by Wallace et al found perforations with the piezoelectric technique occurred during the hand instrumentation phase and not with the piezoelectric inserts. The most common clinical risk factors are the presence of septa and secondly, the presence of a thin membrane. Management of perforations is dependent upon the size, location, and extent of the perforation.
Methods: Patient 1
The first patient is a 56-year-old Caucasian male referred from the undergraduate clinic to the Postdoctoral Clinic at Columbia University, with the chief complaint of missing teeth on the upper left side. He is otherwise medically healthy and is a non-smoker. Clinical and radiographic
(CBCT) examinations highlighted a vertical and horizontal ridge deficiency, missing teeth #’s 13–15, pneumatization of the maxillary sinus and the presence of an anterior and a posterior septum (Figure 1). After anesthesia, a paracrestal incision with anterior and posterior verticals was made sparing the distal papilla of #12.A full thickness mucoperiosteal flap was elevated and an antrostomy of 15 × 20 mm oval shape was made about 3 mm above the sinus floor utilizing a piezoelectric device. Despite the precautions taken, a 9×7 mm perforation occurred on the distal aspect while the graft material was being placed (Figure 2). In order to avoid a second surgical procedure, the complication was addressed by removing the graft material from both sides of the perforation, followed by repair of the perforation with a large, rigid, cross-linked, and slowly resorbing collagen membrane with the dimensions of 20 × 30 mm. The membrane was made long enough to reach the medial wall to prevent the displacement
of bone graft into the posterior cavity (Figure 3). One sinus. A second resorbable membrane was placed over the antrostomy. Closure was achieved with a combination of horizontal mattress and interrupted synthetic resorbable sutures. A postoperative panoramic radiograph showed a well contained graft (Figure 5).
Results: In the first case, a successful sinus lift with containment of the bone graft material was achieved. The second case was successfully treated by removing the implant, repairing the sinus membrane, and placing a new implant and graft material all during the same procedure. In both patients, dental implants were successfully restored within 7 months (Figures 6 and 14).
Conclusions: Management and repair of maxillary sinus perforations, either intentionally or iatrogenically created is a predictable procedure that results in successful procedural outcomes with either delayed or immediate dental implant placement.
Lead Author’s Contributions to the Research Project: I performed the surgeries at Columbia University during my residency.
