Kathleen M. Friel, PhD
Associate Professor
Burke Neurological Institute
White Plains, New York, United States
BIOGRAPHICAL SKETCH
Provide the following information for the Senior/key personnel and other significant contributors.
Follow this format for each person. DO NOT EXCEED FIVE PAGES.
NAME: Kathleen M. Friel, PhD
POSITION TITLE: Director, Clinical Laboratory for Early Brain Injury Recovery, Burke Medical Research Institute, Associate Professor, Brain Mind Research Institute, Weill Cornell Medicine
eRA COMMONS USER NAME (credential, e.g., agency login): KATHYFRIEL
EDUCATION/TRAINING (Begin with baccalaureate or other initial professional education, such as nursing, include postdoctoral training and residency training if applicable. Add/delete rows as necessary.)
INSTITUTION AND LOCATION DEGREE
(if applicable) YEAR(s) FIELD OF STUDY
Rice University, Houston, TX B.A. 1995 Biology
Univ. Texas Health Science Center, Houston, TX M.S. 1997 Neuroscience
Univ. Kansas Medical Center, Kansas City, KS Ph.D. 2002 Physiology/neuroscience
Columbia Univ. Medical Center, New York, NY Postdoctoral 2002-2007 Neuroscience
Columbia Univ. Medical Center, New York, NY M.S. 2010 Biostatistics
A. Personal Statement
Together with others on this R01 supplement study team, I am extremely well-qualified to lead this new kinematics effort. I completed my Ph.D. in the laboratory of Dr. Randolph Nudo at the University of Kansas Medical Center, studying the importance and neurophysiological underpinnings of sensory-motor integration in a primate model of adult stroke. In those studies, I conducted kinematic video analysis of upper limb movements in the primates. I completed my postdoctoral training with Dr. John Martin at Columbia University Medical Center, studying the anatomical, physiological, and motor behavioral consequences of developmental brain injury. The series of five papers that we published form the core of what is known about the circuit changes in hemiplegic cerebral palsy (CP). We identified how these altered circuits can be strengthened with motor training and brain stimulation to promote functional recovery. In my work with Dr. Martin, I also conducted movement analysis from videos of animals performing reaching tasks. As Director of the Clinical Laboratory for Early Brain Injury Recovery at the Burke Medical Research Institute, I use non-invasive brain stimulation (transcranial magnetic stimulation and transcranial direct current stimulation) and magnetic resonance imaging to better understand the neurophysiological mechanisms by which sensory and motor deficits can be restored in children and adults with CP. I currently hold an R01 to study the effects of intensive hand therapy on sensory and motor function, as well as brain plasticity, in children with CP, as well as a second R01 to study sensory impairments in children with CP. Throughout my research career, I have obtained continuous NIH funding for my work (F31, T32, F32, KL2, K01, R03, and R01), demonstrating my strong grant writing skills. In 2010, I obtained an MS in biostatistics, with specialization in Patient Oriented Research, at Columbia’s Mailman School of Public Health.
B. Positions and Honors.
Positions and Employment
1990: Student Research Asst., J. F. Kennedy Space Center, National Aeronautics and Space Admin.
1991-1993: Summer Research Asst., J. F. Kennedy Space Center, National Aeronautics and Space Admin.
1994-1995: Undergraduate research assistant, Department of Biochemistry and Cell Biology, Rice Univ.
1995-1997: Graduate Research Asst., Dept. Neurobiology & Anatomy, Univ. Texas Health Sci. Ctr, Houston.
1997-2002: Graduate Research Asst., Dept. Molecular Integrative Physiology, Univ. Kansas Med. Ctr.
2002: Postdoctoral fellow, Dept. Molecular and Integrative Physiology, University of Kansas Medical Center.
2002-2007: Postdoctoral fellow, Center for Neurobiology and Behavior, Columbia Univ., New York, NY.
2007-2008: Associate Research Scientist, Center for Neurobiology and Behavior, Columbia Univ., New York, NY.
2008-2013: Assistant Professor of Clinical Psychiatry, Division of Brain Stimulation and Therapeutic Modulation, Department of Psychiatry, Columbia Univ., New York, NY.
2013-2019: Assistant Professor, Brain Mind Research Institute, Weill Cornell Medicine, New York, NY.
2013-present: Director, Clinical Laboratory for Early Brain Injury Recovery, Burke Neurological Institute, White Plains, NY.
2015-2019: Director, Cerebral Palsy Research, Blythedale Children’s Hospital, Valhalla, NY
2020-present: Associate Professor, Brain Mind Research Institute, Weill Cornell Medicine, New York, NY.
Other Experience and Professional Memberships
1996-present Society for Neuroscience
1995-present National Chemical Honor Society
1999: Training Symposium, NeuroRecovery Research, Inc.: Stroke drug development: behavior assessment of research animals to determine drug effect
2011-present American Academy of Cerebral Palsy and Developmental Medicine
2015-2019: Member, National Advisory Board for Medical Rehabilitation Research
2017-present: Member, American Society of Neurorehabilitation
2017-present: Member, Scientific Advisory Council, Cerebral Palsy Foundation
2020-present: Ad hoc reviewer, National Institute on Disability, Independent Living, and Rehabilitation Research
2020-present: Ad hoc reviewer, Center for Scientific Review, National Institutes of Health, study section MFSR
2020-present: Ad hoc reviewer, Metavivor
Honors
1993 Tsanoff Prize for outstanding sophomore, Rice University
1995 James Street Fulton Prize for outstanding senior, Rice University
1991-1995 Rice University Tuition Grant
1998 Graduate Student Travel Fellowship, KU Medical Center
1999 Predoctoral National Research Service Award, National Institutes of Neurological Disease and Stroke, Grant number F31 NS11003
2001 P.E.O. Scholar Award, International Chapter P.E.O. Sisterhood
2002 Received Doctor of Philosophy with honors, University of Kansas Medical Center
2004 Postdoctoral National Research Service Award, National Institutes of Neurological Disease and Stroke, Grant number F32 NS46882
2008 K12 Career Development Award, Irving Institute for Clinical and Translational Research, Funded by an NIH CTSA Award to Columbia University (KL2 RR024157, UL1 RR024156, TL1 RR024158).
2012 Gayle Arnold Award, American Academy of Cerebral Palsy and Developmental Medicine
2012 Max Keith Press Promising Career Award, American Academy of Cerebral Palsy and Developmental Medicine
2013 Finalist, Gayle Arnold Award, American Academy of Cerebral Palsy and Developmental Medicine
2014 Named a “Pioneering Woman in Technology,” Westchester County Association, NY
2017 Corbett Ryan Pathways Pioneer Award, American Academy of Cerebral Palsy and Developmental
Medicine
2021 Cerebral Palsy Awareness Research Award, Cerebral Palsy Foundation
2022 Lifelines profile in Lancet Neurology, Jan 2022
C. Contributions to Science
1) Understanding factors that reshape the sensorimotor brain networks after injury: Throughout my research career, I have investigated changes in structure and function of the brain and spinal cord after brain injury in adult (stroke, cerebral palsy) or pediatric (cerebral palsy) model systems. This work has determined that both sensory and motor systems are critical for the production of skillful movements. I showed that motor cortex lesions in a primate model of stroke produce deficits in sensory function that can limit motor recovery. I also determined that both sensory and motor system connectivity and physiology have strong impacts on movement impairments in children with CP.
a. Friel K.M., Kuo HC, Fuller J, Ferre CL, Brandão M, Carmel JB, Bleyenheuft Y, Gowatsky JL, Stanford AD, Rowny SB, Luber B, Bassi B, Murphy DL, Lisanby SH, Gordon AM. (2016). Skilled bimanual training drives motor cortex plasticity in children with unilateral cerebral palsy. Neurorehabil Neural Repair, 30:834-844. PCMID: PMC4981562.
b. Gupta D., Barachant A., Gordon A.M., Kuo A.C., Ferre C.L., Carmel J.B., Friel K.M. (2017). Effect of sensory and motor connectivity on hand function in pediatric hemiplegia. Annals of Neurology, 82(5):766-780. PMCID: PMC5708868.
2) Understanding the importance of skilled sensorimotor training in neurorehabilitation: Throughout my research career, I have investigated the importance of skilled motor training in rehabilitation after brain injury in adult (stroke, cerebral palsy) or pediatric (cerebral palsy) model systems. My work has tested the hypothesis, in many different approaches, that skilled motor rehabilitation is key to recovery. In a non-human primate stroke model, I compared the efficacy of skilled hand training plus constraint therapy with constraint therapy alone. Skill was necessary to optimize recovery. I tested this same hypothesis in a cat model of cerebral palsy and in children with cerebral palsy. Again, I found that skilled training was a key ingredient in maximally improving motor function.
a. Kuo H.-C., Gordon A.M., Henrionnet A., Hautfenne S., Friel K.M., Bleyenheuft Y. (2016). The effects of intensive bimanual training with and without tactile training on tactile function in children with unilateral spastic cerebral palsy: A pilot study. Res Dev Disabil. 2016 Feb-Mar;49-50:129-39. PCMID: PMC4871715.
b. Smorenburg A.R.P., Gordon A.M., Kuo H.C., Ferre C.L., Brandao M., Bleyenheuft Y., Carmel J.B., Friel K.M. (2017). Does corticospinal tract connectivity influence the response to intensive bimanual therapy in children with unilateral cerebral palsy? Neurorehabil Neural Repair, 31(3), 250-260. PCMID: PMC5567681.
c. Friel K.M., Lee P., Soles L.V., Smorenburg A.R.P., Kuo H.-C., Gupta D., Edwards D.J. (2017). Combined transcranial direct current stimulation and robotic upper limb therapy improves upper limb function in an adult with cerebral palsy. NeuroRehabilitation 41:41-50. PMCID: PMC5546204.
3) Understanding neural correlates of sensory and motor impairments in cerebral palsy using neuromodulation and neuroanatomy: My laboratory and collaborators have identified key neurophysiological and neuroanatomical factors that are associated with sensory and motor impairments in people with CP. I have also identified neuroplastic changes associated with recovery of motor and sensory function in children with CP, using diffusion tensor imaging, functional magnetic resonance imaging, and transcranial magnetic stimulation.
a. Bleyenheuft Y., Dricot L., Gilis N. Kuo H.-C., Grandin C. Bleyenheuft C., Gordon A.M. Friel K.M. (2015). Capturing neuroplastic changes after bimanual intensive rehabilitation in children with unilateral spastic cerebral palsy: a combined DTI, TMS, and fMRI pilot study. Res Dev Disabil, 43-44:136-149. PCMID: PMC4871716.
b. Kuo H.-C, Ferre C.L., Carmel J.B., Gowatsky J.L., Stanford A.D., Rowny S.B., Lisanby S.H., Gordon A.M., Friel K.M. (2017). Using diffusion tensor imaging to identify corticospinal tract projection patterns in children with unilateral spastic cerebral palsy. Dev Med Child Neurol 59:65-71. PMCID: PMC5215687.
c. Marneweck M., Hsing-Ching Kuo H.-C., Smorenburg A.R.P, Ferre C.L., Flamand V.H., Gupta D., Carmel J.B., Bleyenheuft Y., Gordon A.M., Friel K.M. (2018). The relationship between hand function and overlapping motor representations of the hands in the contralesional hemisphere in unilateral spastic cerebral palsy. Neurorehabil Neural Repair 32(1):62-72. PMCID: PMC5943063
d. Friel KM, Ferre CL, Brandao M, Kuo H-C, Chin K, Hung YC, Robert MT, Flamand VH, Smorenburg ARP, Bleyenheuft Y, Carmel JB, Campos T, Gordon AM. (2021). Improvements in Upper Extremity Function Following Intensive Training Are Independent of Corticospinal Tract Organization in Children With Unilateral Spastic Cerebral Palsy: A Clinical Randomized Trial. Front Neurol 12:660780.
Complete List of Published Work in MyBibliography: https://www.ncbi.nlm.nih.gov/sites/myncbi/kathleen.friel.1/bibliography/40329011/public/?sort=date&direction=descending
D. Research Support
Ongoing Research Support
National Institute of Child Health and Development, National Institutes of Health
R01 06 HD 076436-01A1 Friel, Kathleen M. (PI) 09/01/20-08/31/24
tDCS plus bimanual training for children with cerebral palsy
Role: PI
National Institute of Child Health and Development, National Institutes of Health
R01 HD 095663-01 Friel, Kathleen M. (PI) 09/13/18-05/31/23
Impact of sensory impairments on movement in children with cerebral palsy
Role: PI
New York State Spinal Cord Injury Board
Assess the effects of rehabilitation on the recovery from nerve transfer 05/01/19-04/30/22
C34463GG Hollis, Edmund and Brown, Justin (PIs)
Role: Co-PI
The Burke Foundation 02/01/13-Ongoing
Institutional support for research administrative duties
Role: Faculty
Completed Research Support
Blythedale Children’s Hospital 01/01/16-06/30/20
Institutional support for hemiplegia research Friel, Kathleen M (Co-PI)
Role: Co-I
National Institute of Child Health and Development, National Institutes of Health
R01 HD 076436-01A1 Friel, Kathleen M. (PI) 09/26/14-08/30/19
Neural predictors of hand therapy efficacy in children with cerebral palsy
Role: PI
National Institute of Child Health and Development, National Institutes of Health 08/01/15-07/31/17
R03 HD 084971-01 Friel, Kathleen M. (PI)
Transcranial direct current stimulation and robotic training in adults with cerebral palsy
Role: PI
Tom and Agnes Carvel Foundation
Friel, Kathleen M. (Co-PI) 09/01/13-12/31/17
Using transcranial direct current stimulation to treat hemiplegic cerebral palsy
Role: Co-PI
National Institute of Child Health and Development, National Institutes of Health
R03 HD 073515 Friel, Kathleen M. (PI) 08/07/2012-07/31/2014
Impact of motor connectivity on efficacy of hand therapy in congenital hemiplegia
Studying associations between motor system connectivity and recovery of function in children with hemiplegic cerebral palsy.
Role: PI
National Institute of Neurological Disorders and Stroke, National Institutes of Health
K01 NS 062116 Friel, Kathleen M. (PI) 09/01/2009-08/31/2013
Mechanisms of Cerebral Palsy Recovery Induced by Balancing Motor Cortex Activity
Studying mechanisms of hemiplegic cerebral palsy recovery in a cat model and in children with hemiplegia. Increasing neural activity to promote recovery. Using electrophysiological, anatomical, and behavioral techniques to assess recovery. Role: PI
I do not have any relevant financial / non-financial relationships with any proprietary interests.
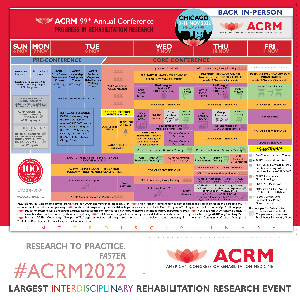
Presentation(s):
-
Tele-Exercise During COVID-19: Effectiveness of an Adaptive Seated Intervention for Adults With Chronic Neurological Impairments
Wednesday, November 9, 2022
3:15 PM – 3:31 PM

.jpg)