Pradeep Suri, MD
Investigator
VA Puget Sound Health Care System
I do not have any relevant financial / non-financial relationships with any proprietary interests.
OMB No. 0925-0001 and 0925-0002 (Rev. 10/2021 Approved Through 09/30/2024)
BIOGRAPHICAL SKETCH
Provide the following information for the Senior/key personnel and other significant contributors.
Follow this format for each person. DO NOT EXCEED FIVE PAGES.
NAME: Pradeep Suri, MD, MS
eRA COMMONS USER NAME (credential, e.g., agency login): SURIPR
POSITION TITLE: Staff Physician, VA Puget Sound Healthcare System
EDUCATION/TRAINING (Begin with baccalaureate or other initial professional education, such as nursing,
include postdoctoral training and residency training if applicable. Add/delete rows as necessary.)
INSTITUTION AND LOCATION
DEGREE
(if
applicable)
Completion
Date
MM/YYYY
FIELD OF STUDY
University of Michigan, Ann Arbor, MI BA 05/1997 Biomedical Science
University of Michigan Medical School,
Ann Arbor, MI MD 05/2002 Medicine
New York Hospital Queens, New York, NY Internship 06/2003 Medicine/Surgery
University of Washington, Seattle, WA Residency 06/2006 Physical Medicine and
Rehabilitation
New England Baptist Hospital, Boston, MA Fellowship 06/2008 Spine Medicine
Harvard University School of Public Health,
Boston, MA MSc 05/2011 Clinical Epidemiology
A. Personal Statement
I am a spine physiatrist and epidemiologist with clinical and research expertise in the management of low back
pain (LBP) and lumbar spinal disorders. I am board certified in Physical Medicine and Rehabilitation, a
practicing clinical spine specialist at the Veterans Affairs (VA) Puget Sound Healthcare System (VAPSHCS),
and a Professor of Rehabilitation Medicine at the University of Washington. I am Deputy Editor of the journal
PM&R. I am also a core Investigator and Epidemiologist at the VAPSHCS Seattle Epidemiologic Research and
Information Center (ERIC), one of 5 VA epidemiology centers. I have experience leading research teams in
multicenter, international collaborative studies in pain genomics, which resulted in my completion of the first
genome-wide association studies (GWAS), meta-GWAS, and Mendelian randomization studies of chronic low
back pain (CLBP) and lumbar spinal stenosis. I led the first classical twin studies of back pain in Veterans,
funded by a Career Development Award (IK2RX001515) from RR&D. I have been the PI of 6 longitudinal
cohort studies or randomized controlled trials (RCTs) of patients with low back pain and/or lumbar disc
herniations. My expertise in lumbar spinal disorders is exemplified by a first-authored review article on the
diagnosis of lumbar spinal stenosis (LSS) that I wrote for the Journal of the American Medical Association
(JAMA) and a podcast I produced for JAMAEvidence. I am the Director of the Resource Core of the University
of Washington (UW) Clinical Learning, Evidence, and Research (CLEAR) Center for Musculoskeletal
Conditions, which has the overarching goal of facilitating methods to use clinical data (mainly electronic health
record [EHR] data) for research purposes. I have also served as a Co-Investigator for 4 other RCTs involving
lumbar spinal disorders or chronic pain. I have a proven record of collaboration with all study team members,
including GWAS and polygenic risk score development with Dr. Stanaway; the development of new outcome
measures and methods with Dr. Chan; and the use of the VA EHR for pain phenotyping and outcome
measurement in VA quality improvement (QI) projects with Dr. Zeliadt; a decade of collaborations with Dr.
Heagerty across numerous projects related to CLBP; and current work with Mr. Morelli who is the data
manager for an ongoing Merit Review grant (PI: Suri) funded by RR&D. In summary, my background as a VA
physician-scientist gives me a unique and deep understanding of lumbar spinal disorders and LBP, spanning
from contemporary research developments to the practical details of providing clinical care. I have the skills to
lead this investigative team and we have the methodologic expertise and resources needed to make the
proposed work a success.
Ongoing research projects I wish to highlight include:
Dept. of Veterans Affairs, Rehabilitation R&D Service Suri (PI) 4/1/2020-9/30/2024
Effects of Physical Activities on Pain and Functional Recovery in Low Back Pain
This is a longitudinal case-crossover study nested with a cohort study. This research uses frequent, serial
survey assessments, actigraphy, and EHR data to examine the short-term and long-term effects of different
types of physical activities on low back pain outcomes among Veterans in VA primary care.
B. Positions, Scientific Appointments, and Honors
Positions and Scientific Appointments:
2022-present Director (Resource Core), Clinical Learning, Evidence, and Research (CLEAR) Center,
University of Washington
2021-present Professor, Rehabilitation Medicine, University of Washington
2021-present Deputy Editor, PM&R
2019-2022 Associate Director (Resource Core), Clinical Learning, Evidence, and Research (CLEAR)
Center, University of Washington
2018-2021 Senior Editor, PM&R
2015-2021 Associate Professor, Rehabilitation Medicine, University of Washington
2013-present Investigator, Comparative Effectiveness, Cost, and Outcomes Research Center
(CECORC)/Clinical Learning, Evidence, and Research (CLEAR) Center, University of
Washington
2013-present Epidemiologist and Investigator, Seattle Epidemiology and Research Information Center (ERIC)
2012-present Staff Physician, Rehabilitation Care Services (Spine Clinic, Musculoskeletal Clinic,
Electrodiagnostic Laboratory), VA Puget Sound Healthcare System
2012-2015 Assistant Professor, Rehabilitation Medicine, University of Washington
2012-2014 Acting Director, Spine and Musculoskeletal Clinics, Rehabilitation Care Services, VA Puget
Sound Healthcare System
2012 Assistant Professor, Physical Medicine and Rehabilitation, Harvard Medical School
2009-2012 Staff Physician, Polytrauma & Pain Clinics, PM&R Services, VA Boston Healthcare System
2008-2012 Attending Physician, Spaulding Rehabilitation Hospital
2008-2012 Instructor, Physical Medicine and Rehabilitation Medicine, Harvard Medical School
2008-2011 Fellow, Rehabilitation Medicine Scientist Training Program
2007-2008 Fellow, Spine and Musculoskeletal Medicine, New England Baptist Hospital
2006-2007 Attending Physician- Back and Neck Clinic/Electrodiagnostic Laboratory, Rehabilitation
Care Services, VA Puget Sound Health Care System.
Honors:
2019 International Society of the Study of the Lumbar Spine (ISSLS) Prize in Clinical Science
(2020): “Examining Causal Effects of Body Mass Index on Back Pain: A Mendelian
Randomization Study"
2016 PM&R Best Paper Award (2016), “Recurrence of Pain after Usual Non-Operative care for
Symptomatic Lumbar Disc Herniation: Analysis of Data from the Spine Patient Outcomes
Research Trial”
2016 The Spine Journal/North American Spine Society Outstanding Paper Award (2016),
Medical/Interventional Science, “Modifiable Risk Factors for Chronic Back Pain: Insights Using
the Co-Twin Control Design.”
2014 Teresa Massagli Award for Outstanding Resident Teaching
2012 Outstanding Scientific Presentation Award, Association of Academic Physiatrists Annual
Meeting
2011 Best Presentation Award, New England Baptist Hospital Annual Research Symposium
2011 Osteoarthritis Research Society International Young Investigator Article of the Month, January
2010 Best Presentation Award, New England Baptist Hospital Annual Research Symposium
2010 Best Poster Award, Association of Academic Physiatrists Annual Meeting
C. Contributions to Science
1. Conducting genome-wide association studies of low back pain, lumbar spinal disorders, and
other musculoskeletal pain sites. Beginning in 2016, I led an international collaboration to conduct the
first GWAS of CLBP. This was a meta-analysis of new GWAS conducted in 16 cohorts from the Cohorts
on Heart and Aging Research Genomic Epidemiology (CHARGE) consortium and the PainOmics
consortium. Since this time, I jsbr led an international pain genomics workgroup that includes Dr.
Stanaway. Our workgroup has used multiple genomic biobanks, self-report, and EHR-based
phenotyping to conduct the first GWAS of “any LBP” (irrespective of chronicity) and symptomatic lumbar
spinal stenosis (SLSS), and a GWAS of lumbosacral radicular syndrome (LSRS, also called ‘sciatica’).
Under my leadership, this workgroup has been at the forefront of pain genomics research for the past 5
years, with 10 pain genomics publications since 2016, two of which have received best paper awards.
Other manuscripts under review include studies of rare variants implicating the gene PANX3 in CLBP;
gene-environment interactions; and initial polygenic risk score development for self-reported back pain.
a. Suri P, Palmer MR, Tsepilov YA, et al. Genome-wide Meta-analysis of 158,000 Individuals of
European Ancestry Identifies Three Loci Associated with Chronic Back Pain. PLoS Genet. 2018
Sep 27;14(9). PMID: 30261039
b. Suri P, Stanaway IB, Zhang Y, et al. Genome-wide association studies of low back pain and
lumbar spinal disorders using electronic health record data identify a locus associated with lumbar
spinal stenosis. Pain. 2021 Feb 4.
c. Freidin MB, Tsepilov YA, Palmer M, Karssen LC, Suri P, Aulchenko YS, Williams FM; CHARGE
Musculoskeletal Working Group. Insight into the genetic architecture of back pain and its risk
factors from a study of 509,000 individuals. Pain. 2019 Feb 6. PMID: 30747904
d. Freidin MB, Tsepilov YA, Stanaway IB, Meng W, Hayward C, Smith BH, Khoury S, Parisien M,
Bortsov A, Diatchenko L, Børte S, Winsvold BS, Brumpton BM, Zwart JA, Aulchenko YS, Suri P,
Williams FMK; HUNT All-In Pain. Sex- and age-specific genetic analysis of chronic back pain. Pain.
2020 Sep 30. PMID: 33021770
2. Identifying risk factors for low back pain that can inform prevention and prognostic factors
that can inform treatment. My work to date has examined non-specific predictors that can identify
patients who should be targeted for more intensive treatment, and causal mechanisms which may
elucidate the underlying biology. I led a cohort study which established the predictive validity of the
STarT Back Tool among Veterans with LBP, but also showed the limitations of this approach, which
is informed by a limited number of traditional risk factors for chronic pain. As part of RR&D-funded
research into the genetics of CLBP (IK2RX001515), I used the co-twin control design to demonstrate
that the association of many traditional risk factors with CLBP is partially explained by shared genetic
factors (pleiotropy). In more recent work, I leveraged large-scale genomic data to conduct Mendelian
randomization studies showing that greater height and body mass index (BMI) are causally
associated with LBP. I also led a series of Mendelian randomization (MR) studies examining
bidirectional relationships between putative risk factors (educational attainment, smoking, alcohol
consumption, physical activity, sleep, and depression) and CLBP (see Appendix). Our team has also
completed studies using MR to examine bidirectional relationships between CLBP, cardiovascular
risk factors, and less commonly studied psychological conditions, and drug repurposing of common
cardiovascular medications, which are not yet reflected as publications.
a. Kneeman J, Battalio S, Korpak A, Luo G, Rundell S, Suri P. Predicting Persistent Disabling Low
Back Pain in Veterans Affairs Primary Care Using the STarT Back Tool. PM R. 2020 Sep 9.
PMID: 32902134
b. Suri P, Boyko E, Smith NL, et al. Modifiable Risk Factors for Chronic Back Pain: Insights Using
the Co-Twin Control Design. Spine J. 2017 Jan;17(1):4-14. PMID: 27794503
c. Elgaeva EE, Tsepilov Y, Freidin MB, Williams FMK, Aulchenko Y, Suri P. ISSLS Prize in Clinical
Science 2020. Examining causal effects of body mass index on back pain: a Mendelian
randomization study. Eur Spine J. 2020 Apr;29(4):686-691. PMID: 31797139
d. Suri P, Palmer MR, Tsepilov YA, et al. Genome-wide Meta-analysis of 158,000 Individuals of
European Ancestry Identifies Three Loci Associated with Chronic Back Pain. PLoS Genet. 2018
Sep 27;14(9). PMID: 30261039
3. Diagnostic accuracy studies for pain-related spinal disorders and spinal imaging findings.
Few of the commonly treated spine-related conditions have ‘gold-standard’ diagnostic methods,
which complicates diagnosis for the non-specialist clinician. I led a diagnostic accuracy study of
lumbosacral radiculopathy in the setting of lumbar disc herniation. I conducted two systematic reviews
of diagnostic methods for symptomatic lumbar spinal stenosis, including a first-author article I
published in the Journal of the American Medical Association (JAMA). Problems of diagnostic
accuracy also apply when developing machine learning methods to identify common and rare spinal
imaging findings among lumbar spine radiograph and magnetic resonance imaging (MRI) reports. My
work as part of the LIRE RCT involved the use of machine learning to detect specific imaging findings
in EHR data (lumbar radiology reports), which we will use in the currently proposed work.
a. Suri P, Rainville J, Kalichman L, Katz JN. Does this older adult with lower extremity pain have the
clinical syndrome of lumbar spinal stenosis? JAMA 2010;304:2628-36. PMID: 21156951
b. Suri P, Rainville J, Katz JN, Jouve C, Hartigan C, Limke J, Pena E, Li L, Swaim B, Hunter DJ.
The accuracy of the physical examination for the diagnosis of midlumbar and low lumbar nerve
root impingement. Spine 2011;36:63-73. PMID: 20543768
c. de Schepper EI, Overdevest GM, Suri P, Peul WC, Oei EH, Koes BW, Bierma-Zeinstra SM,
Luijsterburg PA. Diagnosis of lumbar spinal stenosis: an updated systematic review of the
accuracy of diagnostic tests. Spine (Phila Pa 1976). 2013 Apr 15;38(8):E469-81. PMID:23385136
d. Tan WLK, Hassanpour S, Rundell SD, Suri P, Huhdanpaa H, James KT, Carrell D, Organ N,
Meier E, Sherman K, Kallmes D, Luetmer P, Nerenz D, Heagerty P, Jarvik J. Comparison of
Natural Language Processing Rules-Based and Machine-Learning Systems to Identify Lumbar
Spine Imaging Findings Related to Low Back Pain. Acad Rad 2018 Mar 28. PMID: 29605561
4. Clinical trials of lumbar spinal disorders and pain conditions. I have been PI or Co-I for four
randomized trials of treatments for LBP, lumbar spinal disorders, and chronic pain. I was the PI of the
Selecting Effective Combinations of Treatment (SELECT) pilot RCT comparing LRFA to a simulated
control procedure (NCT03520387). I was a Co-I with the recently completed LIRE trial, the largest
randomized trial of patients with LBP ever conducted; the “SKILLS” RCT comparing three behavioral
treatments for chronic pain; the LESS pragmatic RCT comparing lumbar epidural steroid injections
with and without corticosteroid for the treatment of lumbar spinal stenosis; and the “MATCH”
randomized trial . The LIRE trial defined LBP outcomes entirely using EHR-based phenotyping, as is
proposed for the current work.
a. Suri P, Meier EN, Gold LS, et al. Providing Epidemiologic Data in Lumbar Spine Imaging Reports
Did Not Affect Subsequent Utilization of Spine Procedures: Secondary Outcomes from a Stepped-
Wedge Randomized Controlled Trial. Pain Med. 2021 Feb 17. Online ahead of print. PMID:
33595635
b. Williams RM, Ehde DM, Day M, Turner AP, Hakimian S, Gertz K, Ciol M, McCall A, Kincaid C,
Pettet MW, Patterson D, Suri P, Jensen MP. The chronic pain skills study: Protocol for a
randomized controlled trial comparing hypnosis, mindfulness meditation and pain education in
Veterans. Contemp Clin Trials. 2020 Jan 9;90:105935. [Epub ahead of print] PMID: 31926321
c. Suri P, Pashova H, Heagerty PJ, et al. Short-term Improvements in Disability Mediate Patient
Satisfaction After Epidural Corticosteroid Injections for Symptomatic Lumbar Spinal Stenosis.
Spine (Phila Pa 1976). Spine (Phila Pa 1976). 2015 Sep 1;40(17):1363-70. PMID: 26010037
d. Jarvik JG, Meier EN, James KT, Gold LS, Tan KW, Kessler LG, Suri P, Kallmes DF, Cherkin DC,
Deyo RA, Sherman KJ, Halabi SS, Comstock BA, Luetmer PH, Avins AL, Rundell SD, Griffith B,
Friedly JL, Lavallee DC, Stephens KA, Turner JA, Bresnahan BW, Heagerty PJ. The Effect of
Including Benchmark Prevalence Data of Common Imaging Findings in Spine Image Reports on
Health Care Utilization Among Adults Undergoing Spine Imaging: A Stepped-Wedge Randomized
Clinical Trial. JAMA Netw Open. 2020 Sep 1;3(9):e2015713. PMID: 32886121
Complete List of Published Work in MyBibliography:
My Bibliography complete citation list:
https://www.ncbi.nlm.nih.gov/sites/myncbi/1b34i6aFqGZAq/bibliography/41918355/public/?sort=date&direction
=ascending
Poster(s):
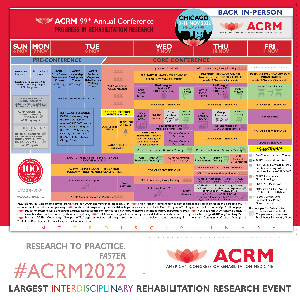
- Combining Procedural and Behavioral Treatments for Chronic Low Back Pain: A Pilot Randomized Controlled TrialWednesday, November 9, 20224:12 PM – 4:17 PM

.jpg)