Peggy Kim, MD
Chief, Pain Management Section, Anesthesia & Pain Medicine Service Line
VA Puget Sound Health Care System
I do not have any relevant financial / non-financial relationships with any proprietary interests.
OMB No. 0925-0001 and 0925-0002 (Rev. 12/2020 Approved Through 02/28/2023)
BIOGRAPHICAL SKETCH
Provide the following information for the Senior/key personnel and other significant contributors.
Follow this format for each person. DO NOT EXCEED FIVE PAGES.
NAME: Kim, Peggy
eRA COMMONS USER NAME (credential, e.g., agency login): PEGGY.KIM
POSITION TITLE: Clinical Associate Professor, University of Washington
EDUCATION/TRAINING (Begin with baccalaureate or other initial professional education, such as nursing, include postdoctoral training and residency training if applicable. Add/delete rows as necessary.)
INSTITUTION AND LOCATION DEGREE
(if applicable)
Completion Date
MM/YYYY
FIELD OF STUDY
Princeton University, Princeton, NJ AB 1994 Psychology
Northwestern University, Evanston, IL MS 2000 Clinical Psychology
DePaul University, Chicago, IL MBA 2006 Health Sector Management
Case Western Reserve University, Cleveland, OH MD 2011 Medicine
Cleveland Clinic Akron General, Akron, OH Resident 2012 Internship
Massachusetts General Hospital Resident 2015 Anesthesiology
University of Texas MD Anderson Cancer Center, Houston, TX Fellowship 2016 Pain Management
A. Personal Statement
I am the Chief of the Pain Management Section at the VA Puget Sound Health Care System, Director of the Pain Clinic and Clinical Associate Professor at the University of Washington School of Medicine. I have the training, expertise and enthusiasm to assist in the successful implementation and support of this project. I have a master’s degree in psychology, during which I completed all of the PhD-level coursework, including statistics, data analysis, and study design. My graduate work in gender and other sexual preferences resulted two peer-reviewed publications. I worked as a senior research associate at the Western Psychiatric Institute and Clinic, conducting standardized psychological diagnostic interviews. Next, I worked as the lead project manager at The University of Chicago Hospitals’ Department of Psychiatry, supervising and coordinating an 11-site NIH/CDC-funded study, completing IRB submissions and ensuring that the study was being carried out appropriately at each satellite site, as well as assisting with grant writing. I have worked as a research associate in industry, as well, serving as a medical monitor, writing clinical study protocols, FDA white papers, and clinical study reports. I then entered medical school, where I spearheaded multiple medical education projects, resulting in 4 peer-reviewed publications. During anesthesia residency, I took the initiative on another medical education study, which resulted in 1 peer-reviewed publication. Since starting as a faculty member at the University of Wisconsin-Madison after completing an interventional pain fellowship, I became a mentor for medical students, residents, and fellows. In total, I have been a coauthor on 40 poster presentations, 16 peer-reviewed articles, and 7 book chapters.
In my role on this project, I will contribute the following: (1) facilitating the proposed research within the VA Puget Sound Pain Clinic’s clinical processes and promoting staff engagement; (2) being available for clinical questions related to recruitment and adverse events; (3) attending regular meetings of the study team; (4) serving on any advisory review teams as requested; and (5) contributing to interpreting the findings and writing manuscripts as requested.
B. Positions, Scientific Appointments, and Honors
Positions and Employment
2020-Present Chief, Pain Management Section, Anesthesia and Pain Medicine Service Line, VA Puget Sound Health Care System, Seattle, WA
2020- Present Clinical Associate Professor, Department of Anesthesiology and Pain Medicine, University of Washington School of Medicine, Seattle, WA
2016-2019 Attending Physician, University of Wisconsin Medical Foundation, Madison, WI
2016-2019 Assistant Professor, Department of Anesthesiology, University of Wisconsin-Madison School of Medicine, Madison, WI
Selected Other Experience and Professional Memberships
2017- Cancer Pain Research Consortium
2017- Wisconsin Society of Anesthesiologists
2017- Wisconsin State Medical Society
2008- American Society of Anesthesiologists (Medical School Delegate 2009 -2001)
2006- Beta Gamma Sigma
1994- Sigma Xi
Selected Honors
2019 Patient and Family Experience Provider Champion Award
2019 John Peterson Award for Humanism in Medicine
2014 Donald P. Todd “Golden Needle” Massachusetts General Hospital Pain Center Resident Award, 2014
2011 Noether Memorial Fund Award for Excellence in Therapeutics, Case Western Reserve University School of Medicine
2011 Scholars in Teaching Award, Case Western Reserve University School of Medicine
2009 Student Scholarship Award for International Association of Medical Science Educators 13th Annual Meeting
2008 Scholars Collaboration in Teaching & Learning Summer Scholarship, Case Western Reserve University School of Medicine
2006 Elected to Beta Gamma Sigma
1994 Elected to Sigma Xi
C. Contributions to Science
1. Anesthesia Residents and Self-Directed Learning. Self-directed learning is an important component of medical education, as it is not possible to provide lectures for every aspect of clinical practice. During residency, I undertook a project to determine whether a decision support system (in the form of an online interface) could assist anesthesia residents in improving their self-directed learning by allowing them to request particular operating room (OR) cases, according to their personal learning needs. My involvement included determining the study design, data collection, assisting with data analysis, and manuscript writing. We found that for the most part, anesthesia residents appeared to request more complex cases as they advanced in training, and the more advanced residents exhibited a stronger preference for highly educational cases than more junior residents. This suggests that residents are capable of and willing to use decision support systems to help them further their learning according to their individualized learning goals.
a) Kim PY, Wanderer JP, Allbritton DW, Eikermann M, Baker, K. Anesthesia residents preferentially request operating room case assignments with complex cases. Journal of Medical Systems, 2017;41(4):64.
2. Supplemental Online Modules Increase Recognition and Production Memory in Medical Students. During medical school, I was concerned that the change in curriculum to a hybrid problem-based learning model was not supporting pharmacology learning in an optimal manner. Thus, I spearheaded a study which created online pharmacology modules to supplement the curriculum and enhance learning in a distributed manner. My contributions included study design, creation of the online modules (with a faculty mentors as advisors for clinical content), data collection, assisting in data analysis, and manuscript writing. This work resulted in multiple peer-reviewed publications, cited below. We found that students who participated in these voluntary supplemental modules not only performed better on recognition memory assessments but also on production memory assessments. Thus, this suggests that distributed online supplemental modules can support deeper learning in a longitudinal manner within a problem-based learning curriculum.
a) Kim PY, Allbritton DW, Keri RA, Mieyal JJ, Wilson-Delfosse AL. Creation of an online curriculum to introduce and supplement the learning of pharmacology in a problem-based learning/lecture hybrid curriculum. Journal of the International Association of Medical Science Educators, 2010;20-2:98-106.
b) Kim PY, Allbritton DW, Keri RA, Mieyal JJ, Wilson-Delfosse AL. Supplemental online pharmacology modules increase recognition and production memory in a hybrid problem-based learning (PBL) curriculum. Medical Science Educator, 2015;25:261-269.
c) Butler R, Kim P, Nieman M, Wilson-Delfosse AL. Implementing web design and usability principles in online medical curricula is associated with improved student utilization and satisfaction. Medical Science Educator, 2015;25:255-259.
3. Predictors of Success on a Written Board Certification Examination. Another project with which I had primary responsibility during medical school was an educational project which focused on potential predictors of success of anesthesia residents on the written anesthesiology board certification examination. I was responsible for creating the study design, data collection, assisting in data analysis, and manuscript writing. We found that factors such as gender, under-represented minority status, and type of medical degree (MD vs. DO) were not significantly correlated with passing the anesthesia written board certification examination. We found that the most important predictors were USMLE Step 2 score and the most recent specialty-specific In-Training Exam (ITE) score, which accounted for 50% of the variance. Therefore, our findings suggest that USMLE Step 2 score could potentially be used early during training to identify residents who may need additional educational support. ITE scores can also be used as an ongoing tool to provide support to those who may not be on track to pass the anesthesia written board examination.
a) Kim PY, Wallace DA, Allbritton DW, Altose MD. Predictors of success on the written anesthesiology board certification examination. International Journal of Medical Education, 2012;3:225-235.
4. Gender and Its Influence on Partner Preferences. During graduate school, I was the lead researcher for a project attempting to elucidate factors which are involved with partner selection for gay men and lesbian women. My contributions included formulating study design; creating study materials, including obtaining inter-rater agreement on materials presented to study participants; coordinating undergraduate students and personally performing data collection; assisted with data analysis, and assisted with manuscript preparation. Our findings were combined with another study and published (citation below). We discovered that gay men had strong preferences for potential hypothetical dating partners who were gender typical, comparable with physical attractiveness level, while lesbian women did not have as strong preferences for gender typical potential dating partners. This work suggests the implications of the role of gender on sexual selection in humans.
a) Bailey JM, Kim PY, Hills A, Linsenmeier JAW. Butch, femme, or straight-acting? Partner preferences of gay men and lesbians. Journal of Personality and Social Psychology, 1997;73:960-973.
Poster(s):
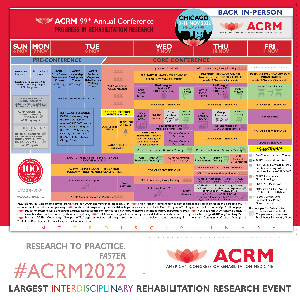
- Combining Procedural and Behavioral Treatments for Chronic Low Back Pain: A Pilot Randomized Controlled TrialWednesday, November 9, 20224:12 PM – 4:17 PM

.jpg)