Janna Friedly, MD
Professor
University of Washington
I do not have any relevant financial / non-financial relationships with any proprietary interests.
OMB No. 0925-0001 and 0925-0002 (Rev. 12/2020 Approved Through 02/28/2023)
BIOGRAPHICAL SKETCH
Provide the following information for the Senior/key personnel and other significant contributors.
Follow this format for each person. DO NOT EXCEED FIVE PAGES.
NAME: Janna Friedly, MD, MPH
eRA COMMONS USER NAME (credential, e.g., agency login): JFRIEDLY
POSITION TITLE: Professor
EDUCATION/TRAINING (Begin with baccalaureate or other initial professional education, such as nursing, include postdoctoral training and residency training if applicable. Add/delete rows as necessary.)
INSTITUTION AND LOCATION DEGREE
(if applicable)
Completion Date
MM/YYYY
FIELD OF STUDY
Stanford University, Stanford, California A.B. 06/1994 Human Biology
Oregon Health & Science University, Portland, OR M.D. 06/2001 Medicine
University of Washington, Seattle, WA 06/2005 Physical Medicine and Rehabilitation residency
George Washington University, Washington, D.C. M.P.H. 06/2020 Public Health
A. Personal Statement
I am a physiatrist and Professor of Physical Medicine and Rehabilitation at the University of Washington and have extensive experience conducting patient centered outcomes research primarily related to low back pain (LBP). I was the PI of the largest comparative effectiveness trial of lumbar epidural steroid injections to date (LESS trial) that included 16 clinical sites across the United States. I have been a co-investigator on 4 additional randomized clinical trials including a trial of behavioral interventions for LBP. Currently I serve as the director of the Resource Core for a NIAMS funded P30 clinical research center grant that has a primary goal of facilitating and training researchers to conduct musculoskeletal research (called the Clinical Learning Effectiveness and Research or CLEAR center). I have worked with Dr. Sean Rundell on a variety of successful back pain related projects. Given my experience with research related to spine conditions and my experience conducting clinical trials, I am well equipped to collaborate with Dr. Rundell on this proposed pilot trial to integrate an evidence-based collaborative care intervention within a community-based exercise program. This is an important project that will provide valuable information to improve our ability to better treat pain in combination with chronic conditions.
1 Friedly JL, Comstock BA, Turner JA, Heagerty PJ, Deyo RA, Sullivan SD, Bauer Z, Bresnahan BW, Avins AL, Nedeljkovic SS, Nerenz DR, Standaert C, Kessler L, Akuthota V, Annaswamy T, Chen A, Diehn F, Firtch W, Gerges FJ, Gilligan C, Goldberg H, Kennedy DJ, Mandel S, Tyburski M, Sanders W, Sibell D, Smuck M, Wasan A, Won L, Jarvik JG. A randomized trial of epidural glucocorticoid injections for spinal stenosis. N Engl J Med. 2014 Jul 3;371(1):11-21. doi: 10.1056/NEJMoa1313265. PubMed PMID: 24988555.
2 Jarvik, J, Gold, L, Comstock, B, Heagerty, P, Rundell, S, Turner, J, Avins, A, Bauer, Z, Bresnahan, B, Friedly, J, James, K, Kessler, L, Nedeljkovic, S, Nerenz, D, Shi, X, Sullivan, S, Chan, L, Schwalb, J, Deyo, R. Association of early imaging in older adults with back pain with clinical outcomes. JAMA. 2015 Mar 17;313(11):1143-53. PubMed PMID: 25781443.
3 Jarvik JG, Meier EN, James KT, Gold LS, Tan KW, Kessler LG, Suri P, Kallmes DF, Cherkin DC, Deyo RA, Sherman KJ, Halabi SS, Comstock BA, Luetmer PH, Avins AL, Rundell SD, Griffith B, Friedly JL, Lavallee DC, Stephens KA, Turner JA, Bresnahan BW, Heagerty PJ. The Effect of Including Benchmark Prevalence Data of Common Imaging Findings in Spine Image Reports on Health Care Utilization Among Adults Undergoing Spine Imaging: A Stepped-Wedge Randomized Clinical Trial. JAMA Netw Open. 2020 Sep 1;3(9):e2015713. doi: 10.1001/jamanetworkopen.2020.15713. PubMed PMID: 32886121; PubMed Central PMCID: PMC7489827.
4 Skelly AC, Chou R, Dettori JR, Turner JA, Friedly JL, Rundell SD, Fu R, Brodt ED, Wasson N, Kantner S, Ferguson AJR. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review Update. 2020 Apr;. Review. PubMed PMID: 32338846.
B. Positions, Scientific Appointments, and Honors
Positions and Scientific Appointments
2021- Member, Scientific Advisory Board, Rehabilitation Medicine Scientist Training Program
2020- Chair, DSMB, NIH/DOD/VA Pain Management Collaboratory program
2019- Vice Chair for Clinical Affairs, Department of Rehabilitation Medicine, University of Washington
2019- Editor-in-Chief, Physical Medicine and Rehabilitation
2019-2020 Chair, Protocol Review Council, NIH/DOD/VA Pain Management Collaboratory program
2019- Member, Washington State Health Technology Clinical Committee (HTCC)
2018- Ex-officio member, American Academy of Physical Medicine and Rehabilitation (AAPMR), Board of Governors
2015-2020 Associate Professor, Department of Rehabilitation Medicine, University of Washington
2014-2018 At large member, UW Physicians Board of Trustees Executive Committee
2013-2014 Patient Experience Champion, Harborview Medical Center
2012-2013 President, Medical Staff at Harborview Medical Center
2010-2015 Assistant Professor, Department of Rehabilitation Medicine, University of Washington
2010-2013 Medical Executive Board, At-Large Member, Harborview Medical Center
2010-2014 Medical Director, Limb Viability Service, Harborview Medical Center
2008-2019 Medical Director, Outpatient Rehabilitation Medicine Clinics, Harborview Medical Center
2007-2010 Acting Assistant Professor, Harborview Medical Center, University of Washington
2005-2007 Acting Instructor, Harborview Medical Center, University of Washington
2005-2008 Rehabilitation Medicine Scientist Training Program (RMSTP) K12 Fellowship
Honors and Awards
2012-2022 Seattle Met’s Top Doctors Award, Seattle, WA
2014 Best Clinical Abstract, Spine Intervention Society 22nd Annual Scientific Meeting, Orlando, FL
2013 UW Medicine PRAISE Award Winner, recognizing physician excellence in patient communication and leadership, Seattle, WA
2013 Seattle Met’s Top Doctors Award, Seattle, WA
2013-2014 Best Doctors in America, Best Doctors, Inc.
2008 AAP Outstanding Platform Paper Presentation and Poster, Association of Academic Physiatrists 2008 Annual Meeting, Anaheim, CA
2006 PASSOR Award for Outstanding Musculoskeletal Research, Honolulu, HI
2005 Outstanding Resident Award, Department of Rehabilitation Medicine, UW
1999 Medical Faculty Auxiliary Award for Academic Excellence, OHSU
1999 Alpha Omega Alpha officer, elected junior year, OHSU
1999 Humanities in Science stipend recipient, OHSU, Portland, OR
1994 Dean’s Award for Public Service, Stanford University, Stanford, CA
1993 Cap and Gown, Women’s Honorary Society, Stanford University, Stanford, CA
C. Contributions to Science
1. Comparative effectiveness of epidural steroid injections: My early research raised significant questions about the effectiveness of epidural steroid injections, particularly for spinal stenosis. My early research demonstrated that about a quarter of injections nationally were being done for this diagnosis, but there were no randomized clinical trials to demonstrate the effectiveness and safety of this treatment in older adults with spinal stenosis. This led me to pursue the conduct of a large pragmatic clinical trial of epidural steroid injections for spinal stenosis, a logical extension of my early research. Through a large AHRQ funded CHOICE award, I served as the PI for the largest multicenter trial of epidural steroid injections to date (the LESS trial) and have answered key questions related to the effectiveness of these treatments. The results of the LESS trial have sparked national discussions with large payers and policymakers about the rationale for continued coverage for epidural injections for this diagnosis. My research team has developed a strong infrastructure for serving as a data coordinating center for large clinical trials and through the LESS trial, I have developed a national infrastructure for conducting further interventional trials in low back pain.
a. Bresnahan BW, Rundell SD, Dagadakis MC, Sullivan SD, Jarvik JG, Nguyen H, Friedly JL. A systematic review to assess comparative effectiveness studies in epidural steroid injections for lumbar spinal stenosis and to estimate reimbursement amounts. PMR. 2013 Aug;5(8):705-14. PMID: 23953016.
b. Friedly J, Bresnahan, B, Comstock B, Turner J, Deyo R, Sullivan S, Heagerty P, Bauer Z, Nedeljkovic S, Avins A, Nerenz D, Jarvik J. Study Protocol- Lumbar Epidural Steroid Injections for Spinal Stenosis (LESS): a double-blind randomized controlled trial of epidural steroid injections for lumbar spinal stenosis among older adults. BMC Musculoskeletal Disorders BMC Musculoskelet Disord. 2012 Mar 29;13:48. PMID: 22458343.
c. Friedly J, Comstock, B, Turner J, Heagerty P, Deyo R, Sullivan S, Bauer Z, et. Al. A Randomized Trial of Epidural Steroid Injections for Spinal Stenosis. N Engl J Med. 2014 Jul 3;371(1):11-21. PMID: 24988555
d. Turner JA, Comstock BA, Standaert C, Heagerty PJ, Jarvik JG, Deyo RA, Wasan AD, Nedeljkovic SS, Friedly JL Can Patient Characteristics Predict Benefit from Epidural Corticosteroid Injections for Lumbar Spinal Stenosis Symptoms?. Spine J. 2015 Jun 18. PMID: 26096484
2. Understanding epidemiology of back pain treatments: The use of and costs associated with a variety of back pain treatments has increased dramatically over time without concurrent improvements in outcomes. Starting with a K12 fellowship under the mentorship of Rick Deyo, MD, MPH, my early career focused on health services research approach to understanding national trends in the use of a variety of treatments for low back pain, including epidural steroid injections. I developed skills in examining key research questions through large datasets, including Medicare and national VA data. My research is highly cited and has drawn national attention to the issue of potential overuse of treatments without demonstrated effectiveness. This early research has guided my ongoing research efforts to determine the effectiveness of back pain treatments through large pragmatic clinical trials.
a. Friedly J, Chan L, Deyo R. Increases in Lumbosacral Injections in the Medicare Population:1994 to 2001. Spine. 2007; 32(16): 1754-60. PMID: 17632396.
b. Friedly J, Nishio I, Maynar C, Bishop M. The Relationship Between Repeated Epidural Steroid Injections on Subsequent Opioid Use and Lumbar Surgery. Arch Phys Med Rehabil. 2008 Jun;89(6):1011-5. PMID: 18503793.
c. Friedly J, Chan L, Deyo, R. Geographic Variations in Epidural Steroid Injection Use in Medicare Patients. J Bone Joint Surg. 2008: 90-A (8): 1730-1737. PMID: 18676905.
d. Friedly J., Standaert, C, Chan, L. Epidemiology of Spine Care: The Back Pain Dilemma. Phys Med Rehabil Clin N Am. 2010 Nov;21(4):659-77. PMID: 20977955.
3. Back pain in older adults: My research that demonstrated increasing use of a variety of back pain treatments in the Medicare population stimulated my interest in further understanding how back pain is treated, particularly in older adults. To this end, I have been a co-investigator with Dr. Jerry Jarvik (Director of the Comparative Effectiveness, Cost and Outcomes Research Center at the University of Washington) on several large projects ranging from the development of a large cohort of older adults with back pain (the BOLD registry) to participating in the conduct of a large multicenter trial, a demonstration project of the NIH Collaboratory, to examine if inserting epidemiologic data in spine imaging reports reduces subsequent diagnostic and treatment procedures for low back pain. Our research has advanced our expertise in conducting large multicenter pragmatic trials, serving as a data coordinating center, collecting and using large EMR datasets as well as using advanced clinical trial design methodology to answer complex research questions.
a. Jarvik JG, Comstock BA, Bresnahan BW, Nedeljkovic SS, Nerenz DR, Bauer Z, Avins AL, James K, Turner JA, Heagerty P, Kessler L, Friedly JL, Sullivan SD, Deyo RA. Study protocol: The back pain outcomes using longitudinal data (BOLD) registry. BMC Musculoskelet Disord. 2012 May 3;13:64. PMID: 22554166.
b. Jarvik, J, Comstock, B, Heagerty, P, Turner, J, Sullivan, S, Shi, X, Nerenz, D, Nedeljkovic, S, Kessler, L, James, K, Friedly, J, Bresnahan, B, Bauer, Z, Avins, A, Deyo, R. Back Pain in Seniors: The Back pain Outcomes using Longitudinal Data (BOLD) Cohort Baseline Data. BMC Musculoskelet Disord. 2014 Apr 23;15:134. PMID: 24755158
c. Jarvik, J, Gold, L, Comstock, B, Heagerty, P, Rundell, S, Turner, J, Avins, A, Bauer, Z, Bresnahan, B, Friedly, J, James, K, Kessler, L, Nedeljkovic, S, Nerenz, D, Shi, X, Sullivan, S, Chan, L, Schwalb, J, Deyo, R. Association of early imaging in older adults with back pain with clinical outcomes. JAMA. 2015 Mar 17;313(11):1143-53. PubMed PMID: 25781443.
d. Edwards TC, Lavallee DC, Bauer Z, Comstock BA, Jarvik JG, Patrick DL, Makris UE, Friedly JL. Problem areas identified as important to older adults with lumbar spinal stenosis. Spine J. 2015 Mar 17. PubMed PMID: 25791366.
4. Amputation Rehabilitation and Pain: Since joining the faculty at UW, I have run the multidisciplinary Amputee Clinic and have provided clinical care for people facing limb loss and those rehabilitating from limb loss. The Amputee program at Harborview Medical Center is nationally known for the exceptional multidisciplinary comprehensive care for patients facing or with limb loss. Given my leadership and expertise working with this population, I was appointed the Medical Director for hospital’s Limb Preservation Service and as part of a quality improvement process, reorganized the service to encompass wound care across the hospital system. One of my main interests clinically has been the treatment of pain in patients with amputation. Given my research expertise, I have started to develop collaborations with researchers in amputation-related research, particularly as it related to neuropathic pain in amputees. I have collaborated with several researchers within the UW system to better understand the impact of TMR surgery on neuroma-related pain. I have participated in a Life Sciences Discovery Fund project and a DOD funded project with Pierre Mourad, PhD in Neurosciences to study a novel high intensity focused ultrasound device that care detect pain thresholds in amputees with neuroma-related pain. Each of these projects will contribute to our understanding of the impact of TMR on the treatment and prevention of neuroma-related pain in amputees. Ultimately, my hope is that this will improve the care of patients with this challenging and debilitating clinical problem.
a. Pet MA, Ko JH, Friedly JL, Mourad PD, Smith DG. Does targeted nerve implantation reduce neuroma pain in amputees? Clin Orthop Relat Res. 2014 Oct;472(10):2991-3001. PubMed Central PMCID: PMC4160473.
b. Morgan SJ, Friedly JL, Amtmann D, Salem R, Hafner BJ. Cross-Sectional Assessment of Factors Related to Pain Intensity and Pain Interference in Lower Limb Prosthesis Users. Arch Phys Med Rehabil. 2017 Jan;98(1):105-113. 2016 Oct 11. PMID: 27742450
c. Pet MA, Ko JH, Friedly JL, Smith DG. Traction Neurectomy for Treatment of Painful Residual Limb Neuroma in Lower Extremity Amputees. J Orthop Trauma. 2015 Mar 28. PubMed PMID: 25875175.
d. Mourad, P, Friedly, J, McClintic, A, Olmstead, T, Loeser, J. Intense Focused Ultrasound Preferentially Stimulates Transected Nerves Within Residual Limbs: Pilot Study Pain Medicine. 07 September 2017 PMID: 29025106
My Bibliography
http://www.ncbi.nlm.nih.gov/sites/myncbi/1z_h6r7aTz4/bibliography/47604950/public/?sort=date&direction=ascending
Poster(s):
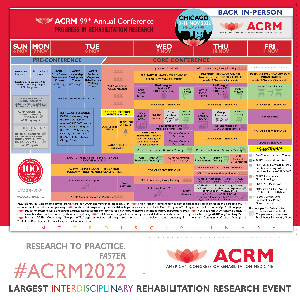
- Combining Procedural and Behavioral Treatments for Chronic Low Back Pain: A Pilot Randomized Controlled TrialWednesday, November 9, 20224:12 PM – 4:17 PM

.jpg)