Jonathan Barlow, MD
Assistant Professor of Orthopedics
Mayo Clinic College of Medicine and Science
I do not have any relevant financial / non-financial relationships with any proprietary interests.
OMB No. 0925-0001 and 0925-0002 (Rev. 03/2020 Approved Through 02/28/2023)
BIOGRAPHICAL SKETCH
Provide the following information for the Senior/key personnel and other significant contributors.
Follow this format for each person. DO NOT EXCEED FIVE PAGES.
NAME: Barlow, Jonathan
eRA COMMONS USER NAME (credential, e.g., agency login): BARLOW142
POSITION TITLE: Orthopedic Surgeon, Division Chair of Community Orthopedic Surgery
EDUCATION/TRAINING (Begin with baccalaureate or other initial professional education, such as nursing, include postdoctoral training and residency training if applicable. Add/delete rows as necessary.)
INSTITUTION AND LOCATION DEGREE
(if applicable) Completion Date
MM/YYYY FIELD OF STUDY
University of Wisconsin, Madison BS 2001-2004 Biology
University of Wisconsin, Madison MD 2004-2008 Medicine
Mayo Orthopedic Surgery Residency MS 2008-2013 Orthopedic Surgery
Rothman Institute/Jefferson University 2013-2014 Shoulder/Elbow Fellowship
Ohio State University 2016-2017 Sports Medicine Fellowship
A. Personal Statement
I am a fellowship-trained shoulder/elbow surgeon with a primary, high volume shoulder orthopedic practice. In my 5 years since fellowship, I have specialized in the treatment and management of rotator cuff pathology. I have published with the MOON Shoulder group which is a Multi-Center Orthopaedic Outcome Network working together to do research with the hopes of giving patients with shoulder problems the best possible care.
B. Positions and Honors
Positions and Employment
2014-2017 Assistant Professor, The Ohio State University-Wexner Medical Center, Columbus, OH
2017-Present Senior Associate Consultant, Orthopedic Surgery, Mayo Clinic, Rochester, MN
2018-Present Division Chair of Community Practice Orthopedics, Department of Orthopedics, Mayo Clinic, Rochester, MN
2018-Present Assistant Professor of Orthopedics, Mayo Clinic College of Medicine and Science, Rochester, MN
Other Experience and Professional Membership
2016-Present Abstract Reviewer, Ohio Shoulder and Elbow Society; Brandon Bell Scholarship
2017-Present Candidate Member, Mid-America Orthopedic Association
2017-Present Member, Mayo Fellows' Association
2017-Present Representative, Web Education Committee, International Congress for Joint Reconstruction
2017-Present Member. American Medical Association
2017-Present Member, American Academy of Orthopedic surgeons
2017-Present Candidate Member, American Society of Shoulder and Elbow Surgeons (ASES)
2018-Present Member, Orthopedic Trauma Association (OTA)
Honors
2008 Alpha Omega Alpha, University of Wisconsin Madison Medical School, Madison, Wisconsin
2008 Honors in Research, University of Wisconsin Madison Medical School, Madison, Wisconsin
2008 Lewis E. and Edith Phillips Academic Scholarship - University of Wisconsin Madison Medical School, Madison, Wisconsin
2010 Coventry Research Award Finalist 2010, Department of Orthopedic Surgery
2012 Kelly Research Award Finalist 2012, Department of Orthopedic Surgery, Mayo Clinic
2012 Representative to ACGME Site Review 2012 - Department of Orthopedic Surgery, Mayo Clinic
2013 Clinical Competency Award, Department of Orthopedic Surgery, Mayo Clinic
Awarded for chief resident with most outstanding faculty evaluations
2013 Coventry Research Award Finalist 2013, Department of Orthopedic Surgery, Mayo Clinic
2013 Joe Janes Award, Department of Orthopedic Surgery, Mayo Clinic
Elected by fellow residents for chief resident most outstanding in clinical responsibilities, research, and teaching
2013 Trauma Chief Resident Award 2013, Department of Orthopedic Surgery, Mayo Clinic
C. Contributions to Science
1. Clinical management of the rotator cuff and glenohumeral joint. My primary clinical practice is focused on the shoulder. I treat patients with rotator cuff pathology, arthritis, and candidates for arthroplasty. My clinical research into these conditions has focused on improving clinical outcomes, surgical techniques, and personalized care for patients with shoulder disorders. Our work has demonstrated that education level, employment status, pain levels, and patient perception of percentage of shoulder normalcy were most predictive of emotional health in patients with full-thickness rotator cuff tears. My research is focused on optimizing patient outcomes with nonoperative and operative treatment of rotator cuff tears.
a. Barlow JD, Bishop JY, Dunn WR, Kuhn JE, Baumgarten KM, Brophy RH, Carey JL, Holloway BG, Jones GL, Ma BC, Marx RG, McCarty EC, Poddar SK, Smith MV, Spencer EE, Vidal AF, Wolf BR, Wright RW, MOON Shoulder Group. What factors are predictors of emotional health in patients with full-thickness rotator cuff tears? J Shoulder Elbow Surg. 2016 Nov; 25 (11):1769-1773 Epub 2016 June 06 PMID: 27282735 DOI: 10.1016/j.jse.2016.04.007
b. Barlow JD, Ravindra A, Jain S, Crasto JA, Bishop JY. Risk Factors for Neurological Injury After Reverse Total Shoulder Arthroplasty. Techniques in Shoulder & Elbow Surgery. 2018 Mar 1;19(1):13-7.
c. Barlow JD, Abboud J. Surgical options for the young patient with glenohumeral arthritis. Int J Shoulder Surg. 2016 Jan-Mar; 10 (1):28-36 PMID: 26980987 PMCID: 4772413 DOI: 10.4103/0973-6042.174516
d. Jahanian O, Van Straaten MG, Goodwin BM, Lennon, RJ, Barlow, JD, Murthy NS, Morrow MM. Shoulder Magnetic Resonance Imaging Findings in Manual Wheelchair Users with Spinal Cord Injury. J Spinal Cord Med. 2020 Nov 9 Epub PMID: 33166207. DOI: 10.1080/10790268.2020.1834774.
2. Effect of Rosiglitazone on a novel rabbit model. In parallel with my residency program at Mayo Clinic, I completed a Master’s Degree training program – obtaining an MS in orthopedic surgery. This program consisted of a 6 month period of dedicated research, with research and classroom expectations throughout the remaining 4.5 years of residency. During this research period, I used a funded program to complete my Master’s Thesis: Effect of Rosiglitazone in reducing flexion contracture in a rabbit model of arthrofibrosis with surgical capsular release: A biomechanical, histological, and genetic analysis (PMID: 26813567). This process involved ideation and creation of the research model of posterior capsular release, as well as the use of rosiglitazone for this model. I personally completed the project, seeing it through from conception through publication.
a. Barlow JD, Morrey ME, Hartzler RU, Riester S, van Wijnen AJ, Morrey BF, Sanchez-Sotelo J, Abdel MP. Effectiveness of rosiglitazone in reducing flexion contracture in a rabbit model of arthrofibrosis with surgical capsular release: A biomechanical, histological, and genetic analysis. Bone Joint Res 2016;5:11-17.
b. Barlow JD, Hartzler RU, Abdel MP, Morrey ME, An KN, Steinmann SP, Morrey BF, Sanchez-Sotelo J. Surgical capsular release reduces flexion contracture in a rabbit model of arthorlfibrosis. J Orthop Res 2013;10:1529-32
3. Implementation of a rabbit model at Rothman Institute. While doing my fellowship at the Rothman Institute in Philadelphia, I was instrumental in developing and expanding their arthrofibrosis project. As a part of Andrzej Fertala’s lab, I designed and implemented a modified rabbit model of arthrofibrosis. This was similar in design to previous studies, but intraarticular drug delivery was designed and created in the rabbit model. I was the lead surgical consultant on the surgical and model design parameters. This lab has used this model for the successful treatment of several studies.
a. Staplewski A, Fertala J, Beredjiklian PK, Abboud JA, Wang MLY, Namdari S, Barlow JD, Rivlin M, Arnold WV, Kostas J, Hou C, Fertala A. Blocking collagen fibril formation in injured knees reduces flexion contracture in a rabbit model. J Orthop Res;35(5):1038-1046.
b. Staplewski A, Fertala J, Beredjiklian PK, Abboud JA, Wang MLY, Namdari S, Barlow JD, Rivlin M, Arnold WV, Kostas J, Hou C, Fertala A. Auxiliary proteins that facilitate formation of collagen-rich deposits in the posterior knee capsule in a rabbit-based joint contracture model. J Orthop Res;35(5):1038-1046.
4. Description of Proximal Humerus Fracture Fixation Technique. As a resident, I designed, researched, and published an article on a series of patients with proximal humerus fractures. This article focused on a technique driven approach to open reduction and internal fixation of proximal humerus fractures in the very elderly. Results were substantially better than several articles were indicating at the time. This technique has become a widespread practice in surgeons across the country.
a. Barlow JD, Sanchez-Sotelo J, Torchia M. Proximal humerus fractures in the eldely can be reliably fixed with a “hybrid” locked plating technique. Clin Orthop Relat Res. 2011;469(12)3281-91.
Complete List of Published Work in MyBibliography:
https://www.ncbi.nlm.nih.gov/sites/myncbi/1JuUavo08kiAn/bibliography/43511013/public/?sort=date&direction=ascending.
D. Additional Information: Research Support and/or Scholastic Performance
No funded research projects in last 3 years.
Poster(s):
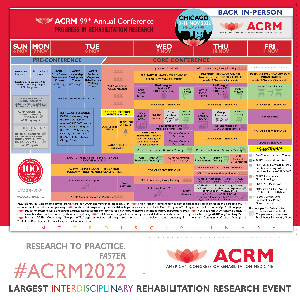
- Rotator Cuff Tear Progression at 2-year Follow-up in Manual Wheelchair Users with Spinal Cord InjuryWednesday, November 9, 20223:08 PM – 3:13 PM

.jpg)