Elyse Walsh, PT, DPT, NCS, CCRC
Clinical Research Coordinator
CARES-Hines VA
I do not have any relevant financial / non-financial relationships with any proprietary interests.
Biographical Sketch
Provide the following information for each individual included in the Research & Related Senior/Key Person Profile (Expanded) Form.
NAME
ELYSE R. WALSH PT,DPT,NCS,CCRC POSITION TITLE
RESEARCH PHYSICAL THERAPIST
EDUCATION/TRAINING (Begin with baccalaureate or other initial professional education, such as nursing, and include postdoctoral training).
INSTITUTION AND LOCATION DEGREE
(IF APPLICABLE) YEAR(S) FIELD OF STUDY
Central Michigan University – Mount Pleasant, MI
University of Southern California – Los Angeles, CA B.S.
DPT 2003-2007
2007-2010 Health Fitness in Preventative and Rehabilitative Programs
Physical Therapy
POSITIONS AND HONORS
2007-2010 California Physical Therapy Association
2007-2018 American Physical Therapy Association
2010 – 2016 Physical Therapist, Rehabilitation Institute of Chicago; Brain Injury, & Day Rehabilitation Programs, Chicago, IL.
2011-2018 Illinois Physical Therapy Association
2012-2018 Neurology Section, American Physical Therapy Association
2014 – 2017 Evening Lab Clinician, Northwestern University Department of Physical Therapy and Human Movement Sciences, Chicago, IL.
2014-Present Clinical Research Therapist, WOC appointment, CARES, Hines VA Medical Center
Hines, IL
2014 Received Neurologic Specialty Certification through the American Board of
Physical Therapy Specialists
2017 Illinois Physical Therapy Association Eastern District Assembly Representative
2020 Received Certified Clinical Research Coordinator Certificate
CONTRIBUTION TO SCIENCE
Publications
Papadimitriou C, Weaver JA, Guernon A, Walsh E, Mallinson T, Pape TLB. "Fluctuation is the norm": Rehabilitation practitioner perspectives on ambiguity and uncertainty in their work with persons in disordered states of consciousness after traumatic brain injury. PLoS One. 2022 Apr 21;17(4):e0267194. doi: 10.1371/journal.pone.0267194. PMID: 35446897; PMCID: PMC9022828.
Kletzel SL, Aaronson AL, Guernon A, Carbone C, Chaudhry N, Walsh E, Conneely M, Patil V, Roth E, Steiner M, Pacheco M, Rosenow J, Bender Pape TL. Safety Considerations for the Use of Transcranial Magnetic Stimulation as Treatment for Coma Recovery in People With Severe Traumatic Brain Injury. J Head Trauma Rehabil. 2020 Nov/Dec;35(6):430-438. doi: 10.1097/HTR.0000000000000636. PMID: 33165155.
Bender Pape TL, Herrold AA, Livengood SL, Guernon A, Weaver JA, Higgins JP, Rosenow JM, Walsh E, Bhaumik R, Pacheco M, Patil VK, Kletzel S, Conneely M, Bhaumik DK, Mallinson T, Parrish T. A Pilot Trial Examining the Merits of Combining Amantadine and Repetitive Transcranial Magnetic Stimulation as an Intervention for Persons With Disordered Consciousness After TBI. J Head Trauma Rehabil. 2020 Nov/Dec;35(6):371-387. doi: 10.1097/HTR.0000000000000634. PMID: 33165151.
Poster Presentations
Chaudhry N, Livengood S, Alsakaji R, Higgins J, Walsh E, Guernon A, Kletzel S, Parrish T, Bender Pape T, (2022, March). (C4) Music vs. Language Processing in Disorders of Consciousness from Severe Traumatic Brain Injury. Poster Presented at: Chicago Chapter of the Society for Neuroscience: 2022 Scientific Meeting; 2022 Mar 4.
Bender Pape, T Foecking, E Zilliox, M Saban, K Herrold, A Kletzel, S Walsh, E Guernon, A Pape, A Bhaumik, D Conneely, M. (2020) A Primary study examining utility of miRNA for diagnosing TBI, developing phenotypes of TBI recovery and developing phenotypes of treatment responsiveness. Military Health System Research Symposium (MHSRS) (Poster Abstract # MHSRS-20-00883 for TBI Biomarkers: Diagnostic & Prognostic Indicators - Peripheral Blood miRNA Biomarkers for TBI) (Accepted Poster) *Conference cancelled due to COVID-19
Bender Pape, T Mallinson, T Papadimitriou, C Guernon, A Walsh, E O’Brien, K Weaver, J. (2020) Co-calibrating Five Assessments of Neurobehavioral Sensory-Motor Function in Persons in Disordered States of Consciousness. Military Health System Research Symposium (MHSRS) (Poster Abstract # MHSRS-20-01966 for Improving Neurosensory Function after TBI) (Accepted Poster) *Conference cancelled due to COVID-19
Mallinson T, Pape T, Guernon A, Weaver J, Walsh E. Steering a Clinician- Reported TBI Outcome Assessment Through the FDA Drug Development Tool Qualification Program: A collaboration between industry, academic, and clinical partners. Military Health System Research Symposium. August 27-30 2017.
Papadimitriou C, Mallinson T, Pape T, Guernon A, Weaver J, Walsh E. Exemplars of Meaningful Change in Patients with Disorders of Consciousness: Clinician Perspectives on Recovery of Neurobehavioral Function. International Brain Injury Association 12th World Congress on Brain Injury. March 29-April 1 2017.
Lyons L, Mallinson T, Pape T, Guernon A, Cotton L, Weaver J, Walsh E. SMARTraining: A Novel Approach for Teaching Clinicians, Family Members, and Caregivers to Conduct Neurobehavioral Assessments. International Brain Injury Association 12th World Congress on Brain Injury. March 29- April 1 2017.
Walsh E, Blabas B, Gurnon A, Pape T. Reliability of Motor Threshold Testing. Poster Presentation. American Congress of Rehabilitation Medicine Annual Conference. November 2-4 2016.
RESEARCH SUPPORT
1. rTMS: A Treatment to Restore Function after Severe TBI. CDMRP and Department of Army Grant #PT120274. Goals of the project are to address the need for targeted treatments to improve neurobehavioral functioning in minimally conscious and vegetative patients. My role includes subject recruitment, subject/surrogate consenting, IRB management including amendments and addendums to the current protocol, adverse event reporting as necessary, subject scheduling, administration of TMS protocol, administration of outcome assessments, and data entry/management.
2. Neurmodulation and Neurorehabilitation for Treatment of Functional Deficits after mTBI plus PTSD. Goals of this project include determining the immediate effects of active APT-III + Active iTBS on neurophychological measures of attention, measures of fucnitonal status, and symptoms. My role includes subject recruitment, subject consenting, administration of intervention protocol, administration of outcomes assessments, and data entry.
3. Understanding Clinician Language Regarding Neurobehavioral Change of Persons in Disordered States of consciousness. Goals of this project include understanding how clinicians describe change for patients in states of disordered consciousness and what clinicians consider meaningful change. My role includes IRB submission for three recruitment sites, conducting clinician interviews, assisting with interview transcription, and data management.
Poster(s):
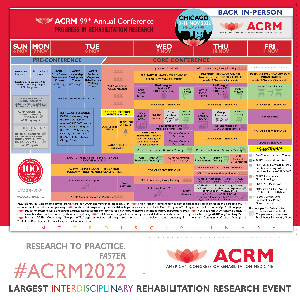
- "My Person" or "A Person": CarePartner and Practitioner Perceptions Caring for Persons in Disordered ConsciousnessWednesday, November 9, 20229:45 AM – 9:50 AM

.jpg)