Back
Poster Session C
Imaging
Session: (1228–1266) Imaging of Rheumatic Diseases Poster
1228: Distinctive Alterations in the Functional Anatomy of the Cerebral Cortex in Pain-sensitized Osteoarthritis and Fibromyalgia Patients
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- FO
Fabiola Ojeda, MD
Hospital del Mar
Barcelona, Spain
Abstract Poster Presenter(s)
Jesús Pujol1, Fabiola Ojeda1, Laura Blanco-Hinojo1, Andrea Doreste1, Gerard Martinez-Vilavella1, Víctor Pérez-Solá1, Joan Deus2 and Jordi Monfort1, 1Hospital del Mar, Barcelona, Spain, 2Autonomous University of Barcelona, Barcelona, Spain
Background/Purpose: Fibromyalgia is a primary pain sensitization disorder showing augmented pain sensitivity with no apparent origin. In contrast, secondary sensitization often occurs in knee osteoarthritis patients in the form of lower pain thresholds an regional spreading of pain originally related to the peripheral damage. We hypothesized that primary and secondary pain sensitization would show a different repercussion on the cerebral cortex functioning with more alteration in the nociceptive system in the case of knee osteoarthritis and in cortical areas integrating general sensory information in fibromyalgia. We aimed at assessing the functional repercussions of pain sensitization in the cerebral cortex in sensitized knee osteoarthritis and fibromyalgia patients using novel local connectivity measures.
Methods: A total of 65 pain-sensitized knee osteoarthritis patients, 101 fibromyalgia patients and 60 healthy control subjects were examined using resting state functional MRI. Iso-distance average connectivity (IDAC) measures were estimated to map local, short-distance functional alterations in the cerebral cortex (1).
Results: In osteoarthritis, weaker local connectivity was identified in the insula, which is a cortical area processing important aspects of the brain response to painful stimulation. In contrast, fibromyalgia patients showed weaker connectivity in the sensorimotor cortex extensively affecting the cortical representation of the body (Figure 1).
Conclusion: In osteoarthritis, weaker insular cortex connectivity is compatible with reduced neural activity during metabolic recovery after repeated activation. In the fibromyalgia neurophysiological context, weaker connectivity may better express both reduced neural activity and increased excitability, particularly affecting the sensorimotor cortex in patients with spontaneous body pain. Such a combination is compatible with a central gain enhancement mechanism, where low sensory tolerance results from the over-amplification of central sensory reception to compensate a presumably weak sensory input. We propose that deficient proprioception could be a factor contributing to weak sensory input.
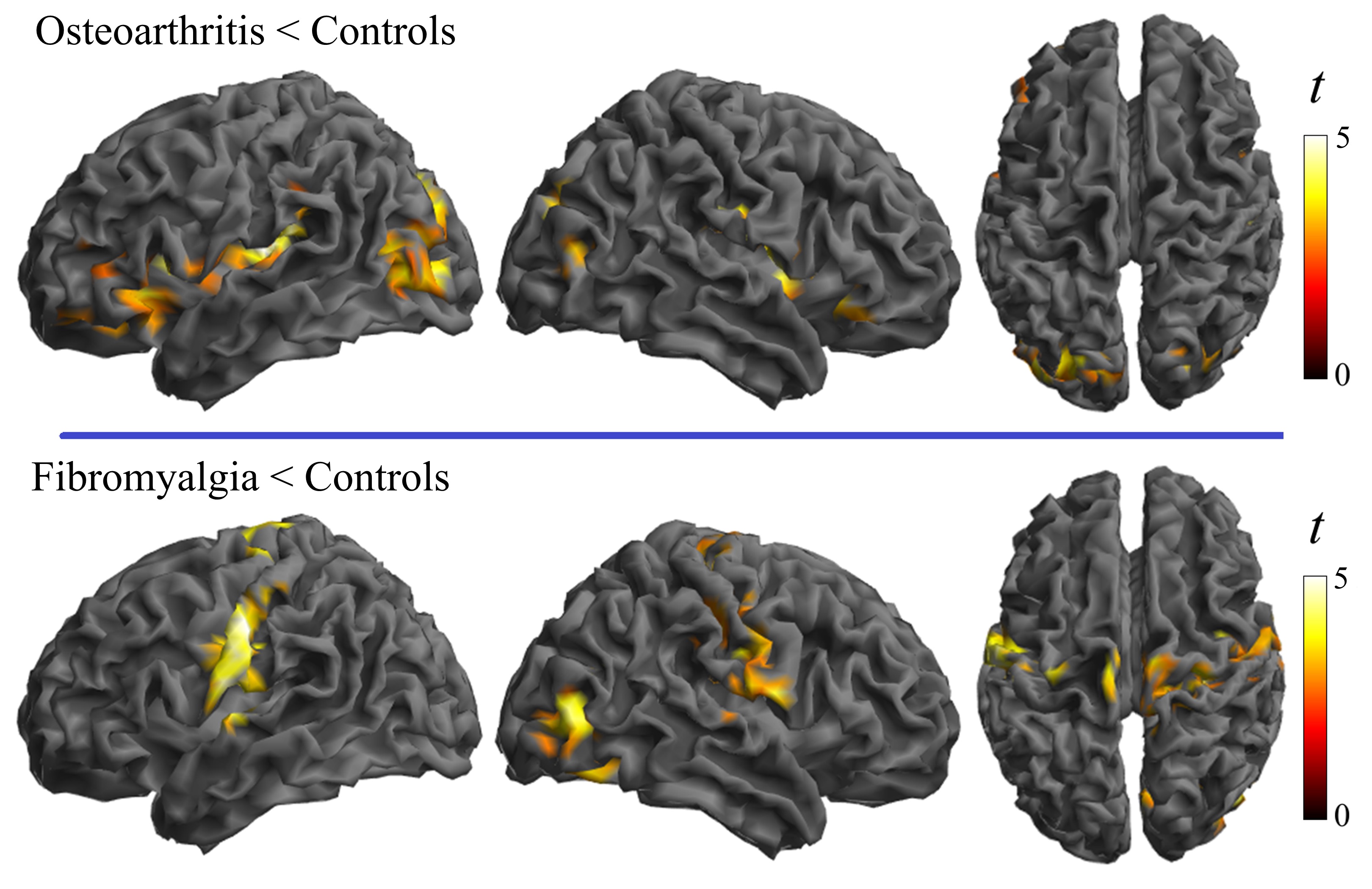 Figure 1. Main between-group differences in local functional connectivity IDAC measures in osteoarthritis and fibromyalgia patients versus their respective control groups. All the identified alterations were in the direction of weaker connectivity in the patient condition.
Figure 1. Main between-group differences in local functional connectivity IDAC measures in osteoarthritis and fibromyalgia patients versus their respective control groups. All the identified alterations were in the direction of weaker connectivity in the patient condition.
Disclosures: J. Pujol, None; F. Ojeda, None; L. Blanco-Hinojo, None; A. Doreste, None; G. Martinez-Vilavella, None; V. Pérez-Solá, None; J. Deus, None; J. Monfort, GlaxoSmithKlein(GSK).
Background/Purpose: Fibromyalgia is a primary pain sensitization disorder showing augmented pain sensitivity with no apparent origin. In contrast, secondary sensitization often occurs in knee osteoarthritis patients in the form of lower pain thresholds an regional spreading of pain originally related to the peripheral damage. We hypothesized that primary and secondary pain sensitization would show a different repercussion on the cerebral cortex functioning with more alteration in the nociceptive system in the case of knee osteoarthritis and in cortical areas integrating general sensory information in fibromyalgia. We aimed at assessing the functional repercussions of pain sensitization in the cerebral cortex in sensitized knee osteoarthritis and fibromyalgia patients using novel local connectivity measures.
Methods: A total of 65 pain-sensitized knee osteoarthritis patients, 101 fibromyalgia patients and 60 healthy control subjects were examined using resting state functional MRI. Iso-distance average connectivity (IDAC) measures were estimated to map local, short-distance functional alterations in the cerebral cortex (1).
Results: In osteoarthritis, weaker local connectivity was identified in the insula, which is a cortical area processing important aspects of the brain response to painful stimulation. In contrast, fibromyalgia patients showed weaker connectivity in the sensorimotor cortex extensively affecting the cortical representation of the body (Figure 1).
Conclusion: In osteoarthritis, weaker insular cortex connectivity is compatible with reduced neural activity during metabolic recovery after repeated activation. In the fibromyalgia neurophysiological context, weaker connectivity may better express both reduced neural activity and increased excitability, particularly affecting the sensorimotor cortex in patients with spontaneous body pain. Such a combination is compatible with a central gain enhancement mechanism, where low sensory tolerance results from the over-amplification of central sensory reception to compensate a presumably weak sensory input. We propose that deficient proprioception could be a factor contributing to weak sensory input.
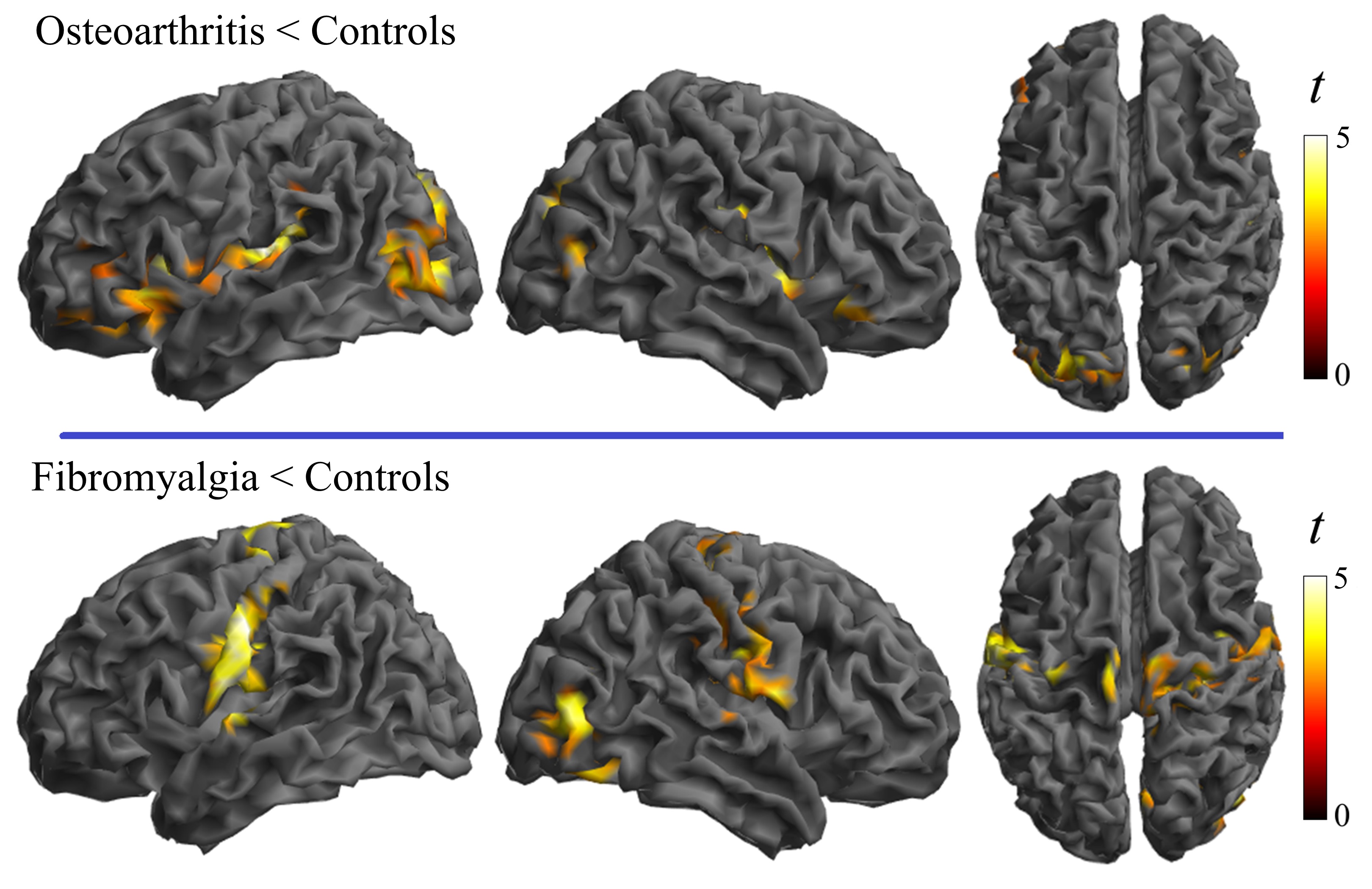 Figure 1. Main between-group differences in local functional connectivity IDAC measures in osteoarthritis and fibromyalgia patients versus their respective control groups. All the identified alterations were in the direction of weaker connectivity in the patient condition.
Figure 1. Main between-group differences in local functional connectivity IDAC measures in osteoarthritis and fibromyalgia patients versus their respective control groups. All the identified alterations were in the direction of weaker connectivity in the patient condition.Disclosures: J. Pujol, None; F. Ojeda, None; L. Blanco-Hinojo, None; A. Doreste, None; G. Martinez-Vilavella, None; V. Pérez-Solá, None; J. Deus, None; J. Monfort, GlaxoSmithKlein(GSK).

