Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1186–1214) Epidemiology and Public Health Poster II
1195: Duloxetine and the Risk for Acute Myocardial Infarction and Stroke in Medicare Recipients with Non-Cancer Pain
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- MC
Meghan Corriere, MPH
Vanderbilt University
Nashville, TN, United States
Abstract Poster Presenter(s)
Meghan Corriere, Alyson Dickson, Laura Daniel, Puran Nepal, Kathi Hall, Dale Plummer, William Dupont, Katherine Murray, Michael Stein, Wayne Ray and Cecilia Chung, Vanderbilt University Medical Center, Nashville, TN
Background/Purpose: Duloxetine is a serotonin-norepinephrine reuptake inhibitor antidepressant also prescribed for musculoskeletal and other forms of chronic pain. Its dual pharmacologic properties have the potential to either raise or lower cardiovascular risk: adrenergic activity may increase the risk for acute myocardial infarction (AMI) and stroke, but antiplatelet activity may decrease risk. With current emphasis on the use of non-opioid medications to treat patients with chronic pain, assessing cardiovascular risks associated with these medications among high-risk patients is important.
Methods: We conducted a retrospective cohort study of new users of duloxetine or gabapentin (the active comparator) among a 20% sample of Medicare recipients who had chronic pain, were 65-89 years old, and filled prescriptions between 2015 and 2018. We excluded individuals with cancer or other life-threatening diagnoses in the year prior to first prescription fill. The primary outcome was a composite of AMI and stroke ascertained by validated algorithms using ICD-9 and ICD-10 codes. We calculated time-dependent propensity scores and used inverse probability weighting analysis to compare the risk of AMI and stroke between the study drugs.
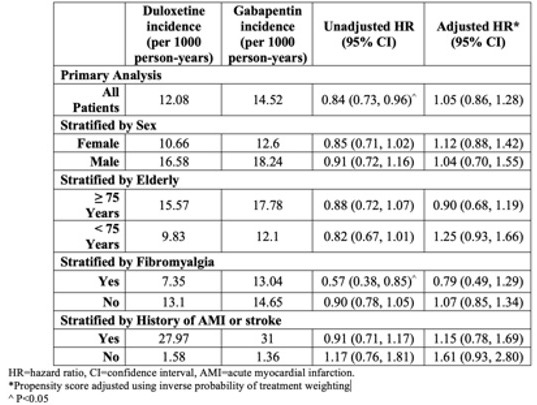
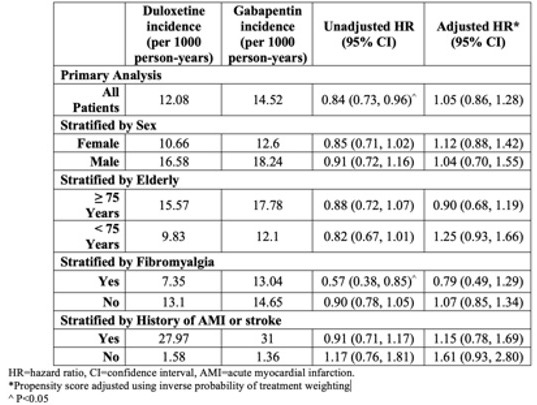
Results: The study included 33,999 new users of duloxetine and 232,824 of gabapentin. The cohort was predominantly female (65.9%) and non-Hispanic White (80.3%), with a median age of 73. The most common chronic pain diagnoses were back pain (67.2%) and other musculoskeletal conditions (71.6%). At baseline, the groups had similar rates of cardiovascular comorbidities and medications, as well as other pain medications. However, before inverse probability weighting, the groups differed in several respects. More duloxetine than gabapentin users (74.6% vs. 64.6%) were female and had neuropathic pain (60.9% vs. 43.3%). Duloxetine users had higher rates of fibromyalgia (22.5%) than gabapentin users (12.3%). After propensity score weighting none of the variables had a standardized difference >0.10. During 115,925 person-years of follow-up, 1,635 patients had either an AMI or stroke. The rate of AMI or stroke among new users of duloxetine was 12.1/1,000 person-years compared to new users of gabapentin (14.5/1,000 person-years), time-dependent, adjusted HR=1.05 (95%CI: 0.86-1.28). Results were similar for the individual components of the composite outcome as well as for analyses stratified by race, sex, age≥75 years old, and when restricted to patients with fibromyalgia indication (Table).
Conclusion: In this large-scale retrospective study of elderly patients treated for non-cancer pain, new users of duloxetine and gabapentin had comparable rates of AMI and stroke.
 Acute Myocardial Infarction/Stroke Risk
Acute Myocardial Infarction/Stroke Risk
Disclosures: M. Corriere, None; A. Dickson, None; L. Daniel, None; P. Nepal, None; K. Hall, None; D. Plummer, None; W. Dupont, None; K. Murray, None; M. Stein, None; W. Ray, None; C. Chung, None.
Background/Purpose: Duloxetine is a serotonin-norepinephrine reuptake inhibitor antidepressant also prescribed for musculoskeletal and other forms of chronic pain. Its dual pharmacologic properties have the potential to either raise or lower cardiovascular risk: adrenergic activity may increase the risk for acute myocardial infarction (AMI) and stroke, but antiplatelet activity may decrease risk. With current emphasis on the use of non-opioid medications to treat patients with chronic pain, assessing cardiovascular risks associated with these medications among high-risk patients is important.
Methods: We conducted a retrospective cohort study of new users of duloxetine or gabapentin (the active comparator) among a 20% sample of Medicare recipients who had chronic pain, were 65-89 years old, and filled prescriptions between 2015 and 2018. We excluded individuals with cancer or other life-threatening diagnoses in the year prior to first prescription fill. The primary outcome was a composite of AMI and stroke ascertained by validated algorithms using ICD-9 and ICD-10 codes. We calculated time-dependent propensity scores and used inverse probability weighting analysis to compare the risk of AMI and stroke between the study drugs.
Results: The study included 33,999 new users of duloxetine and 232,824 of gabapentin. The cohort was predominantly female (65.9%) and non-Hispanic White (80.3%), with a median age of 73. The most common chronic pain diagnoses were back pain (67.2%) and other musculoskeletal conditions (71.6%). At baseline, the groups had similar rates of cardiovascular comorbidities and medications, as well as other pain medications. However, before inverse probability weighting, the groups differed in several respects. More duloxetine than gabapentin users (74.6% vs. 64.6%) were female and had neuropathic pain (60.9% vs. 43.3%). Duloxetine users had higher rates of fibromyalgia (22.5%) than gabapentin users (12.3%). After propensity score weighting none of the variables had a standardized difference >0.10. During 115,925 person-years of follow-up, 1,635 patients had either an AMI or stroke. The rate of AMI or stroke among new users of duloxetine was 12.1/1,000 person-years compared to new users of gabapentin (14.5/1,000 person-years), time-dependent, adjusted HR=1.05 (95%CI: 0.86-1.28). Results were similar for the individual components of the composite outcome as well as for analyses stratified by race, sex, age≥75 years old, and when restricted to patients with fibromyalgia indication (Table).
Conclusion: In this large-scale retrospective study of elderly patients treated for non-cancer pain, new users of duloxetine and gabapentin had comparable rates of AMI and stroke.
 Acute Myocardial Infarction/Stroke Risk
Acute Myocardial Infarction/Stroke RiskDisclosures: M. Corriere, None; A. Dickson, None; L. Daniel, None; P. Nepal, None; K. Hall, None; D. Plummer, None; W. Dupont, None; K. Murray, None; M. Stein, None; W. Ray, None; C. Chung, None.

