Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1475: Epidemiology of Acute Ischemic Stroke in Patients with Systemic Lupus Erythematosus
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- UK
Uzair Khan, DO
NYITCOM
Odessa, FL, United States
Abstract Poster Presenter(s)
Uzair Khan1, Izza Bazigh2, Achint Patel3, Aaparna Singh3, Neha Ghalib3, Ghazi Farman4, Salman Muddassir3, Farrukh Zaidi5, Sami Mughni3 and Adam Grunbaum6, 1HCA Healthcare Florida / USF Morsani College of Medicine GME Consortium / Oak Hill Hospital, Odessa, FL, 2HCA Florida Oak Hill Hospital, Spring Hill, FL, 3HCA Healthcare Florida / USF Morsani College of Medicine GME Consortium / Oak Hill Hospital, Spring Hill, FL, 4Rehman Medical College, Spring Hill, FL, 5HCA Healthcare Florida / USF Morsani College of Medicine GME Consortium / Oak Hill Hospital, Port Richey, FL, 6Gulf Coast Rheumatology, Trinity, FL
Background/Purpose: Vascular events, including cerebrovascular accidents (CVA) occur earlier and more frequently in patients with Systemic Lupus Erythematosus (SLE) compared with healthy individuals. Several studies aiming to evaluate the risk of Acute Ischemic Stroke (AIS) and other vascular events in adult patients with SLE concluded that there is a two to three-fold higher risk of stroke in patients with SLE. Apart from the traditional role of accelerated atherosclerosis, anti-phospholipid antibodies (in particular lupus anticoagulant) has been well studied in increasing the risk of future thrombosis. There is paucity of data that describes epidemiological trends and risk factors associated with AIS among SLE patients. Our study aims to utilize the largest national database from the United States to estimate temporal trends, predictors and in-hospital outcomes of hospitalizations due to AIS among SLE patients.
Methods: We extracted hospitalizations among adult SLE patients due to AIS using Nationwide Inpatient Sample (NIS) and Healthcare Cost and Utilization Project (HCUP) data for years 2010-2018. Previously validated ICD-9/10-CM codes were used to identify diagnoses of interest. We then utilized the Cochrane Armitage trend test and multivariate survey logistic regression models to analyze trends and predictors of AIS among SLE patients. We used SAS 9.4 software for analyzing the data.
Results: We identified 19,648 hospitalizations due to primary diagnosis of AIS out of a total of 1,636,848 hospitalizations among SLE patients. We observed an increasing trend of AIS from 1754 (1.0%) in 2010 to 2385 (1.3%) in 2018 (p:< 0.001). Even after adjusting with demographics and patient characteristics, AIS hospitalizations increased by 4% annually (OR 1.04; 95%CI 1.03-1.05; p< 0.0001). SLE patients with AIS were more likely to be older, male and African American. In multivariable survey regression analysis, male gender (OR 1.2; 95%CI 1.1-1.4; p< 0.0001), increasing age (OR 1.3; 95%CI 1.2-1.3; p< 0.0001), African American ethnicity (OR 1.3; 95%CI 1.2-1.4; p< 0.0001), Antiphospholipid antibodies (OR 3.3; 95%CI 2.9-3.7; p< 0.0001), smoking, valvular heart disease, hypertension and diabetes mellitus were associated with increased odds of hospitalization due to AIS among SLE patients. We observed in-hospital mortality rate of 2.9% and rate of discharge to facilities of 40% among SLE patients admitted due to AIS.
Conclusion: Our study describes epidemiological trend of AIS among SLE patients. Our study concludes that hospitalizations due to AIS among SLE patients has increased during 2010-2018. There are several patient demographics and co-morbidities associated with increased odds of AIS in SLE patients. AIS is also associated with significantly higher morbidity and morality among SLE patients. Further studies are warranted to develop the better risk stratification strategies targeted to improve outcomes among these vulnerable population.
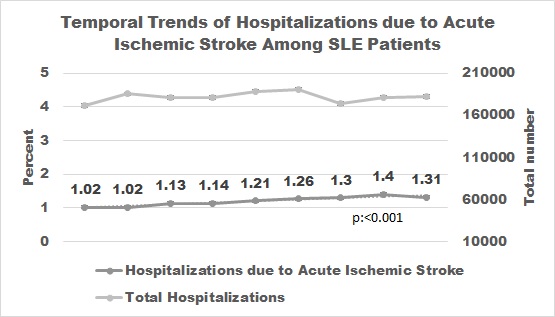 Temporal Trends of Hospitalizations due to Acute Ischemic Stroke in systemic Lupus Erythematosus
Temporal Trends of Hospitalizations due to Acute Ischemic Stroke in systemic Lupus Erythematosus
Disclosures: U. Khan, None; I. Bazigh, None; A. Patel, None; A. Singh, None; N. Ghalib, None; G. Farman, None; S. Muddassir, None; F. Zaidi, None; S. Mughni, None; A. Grunbaum, None.
Background/Purpose: Vascular events, including cerebrovascular accidents (CVA) occur earlier and more frequently in patients with Systemic Lupus Erythematosus (SLE) compared with healthy individuals. Several studies aiming to evaluate the risk of Acute Ischemic Stroke (AIS) and other vascular events in adult patients with SLE concluded that there is a two to three-fold higher risk of stroke in patients with SLE. Apart from the traditional role of accelerated atherosclerosis, anti-phospholipid antibodies (in particular lupus anticoagulant) has been well studied in increasing the risk of future thrombosis. There is paucity of data that describes epidemiological trends and risk factors associated with AIS among SLE patients. Our study aims to utilize the largest national database from the United States to estimate temporal trends, predictors and in-hospital outcomes of hospitalizations due to AIS among SLE patients.
Methods: We extracted hospitalizations among adult SLE patients due to AIS using Nationwide Inpatient Sample (NIS) and Healthcare Cost and Utilization Project (HCUP) data for years 2010-2018. Previously validated ICD-9/10-CM codes were used to identify diagnoses of interest. We then utilized the Cochrane Armitage trend test and multivariate survey logistic regression models to analyze trends and predictors of AIS among SLE patients. We used SAS 9.4 software for analyzing the data.
Results: We identified 19,648 hospitalizations due to primary diagnosis of AIS out of a total of 1,636,848 hospitalizations among SLE patients. We observed an increasing trend of AIS from 1754 (1.0%) in 2010 to 2385 (1.3%) in 2018 (p:< 0.001). Even after adjusting with demographics and patient characteristics, AIS hospitalizations increased by 4% annually (OR 1.04; 95%CI 1.03-1.05; p< 0.0001). SLE patients with AIS were more likely to be older, male and African American. In multivariable survey regression analysis, male gender (OR 1.2; 95%CI 1.1-1.4; p< 0.0001), increasing age (OR 1.3; 95%CI 1.2-1.3; p< 0.0001), African American ethnicity (OR 1.3; 95%CI 1.2-1.4; p< 0.0001), Antiphospholipid antibodies (OR 3.3; 95%CI 2.9-3.7; p< 0.0001), smoking, valvular heart disease, hypertension and diabetes mellitus were associated with increased odds of hospitalization due to AIS among SLE patients. We observed in-hospital mortality rate of 2.9% and rate of discharge to facilities of 40% among SLE patients admitted due to AIS.
Conclusion: Our study describes epidemiological trend of AIS among SLE patients. Our study concludes that hospitalizations due to AIS among SLE patients has increased during 2010-2018. There are several patient demographics and co-morbidities associated with increased odds of AIS in SLE patients. AIS is also associated with significantly higher morbidity and morality among SLE patients. Further studies are warranted to develop the better risk stratification strategies targeted to improve outcomes among these vulnerable population.
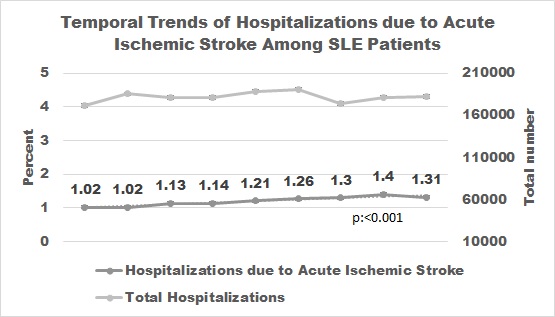 Temporal Trends of Hospitalizations due to Acute Ischemic Stroke in systemic Lupus Erythematosus
Temporal Trends of Hospitalizations due to Acute Ischemic Stroke in systemic Lupus Erythematosus Disclosures: U. Khan, None; I. Bazigh, None; A. Patel, None; A. Singh, None; N. Ghalib, None; G. Farman, None; S. Muddassir, None; F. Zaidi, None; S. Mughni, None; A. Grunbaum, None.

