Back
Poster Session C
Imaging
Session: (1228–1266) Imaging of Rheumatic Diseases Poster
1229: Erosion Score and Erosive Joint Number Using Radiography: Clinical Implications in Patients with ACPA+ Early RA Treated with Abatacept
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- CP
Chahin Pachai, PhD
Bristol Myers Squibb
Princeton, NJ, United States
Abstract Poster Presenter(s)
Chahin Pachai1, Sean E Connolly2, Yoshiya Tanaka3, Vivian Bykerk4, Tom Huizinga5, Gustavo Citera6, Clifton O. Bingham III7, Shuyan Du1, Godehard Hoexter8, Paul Emery9, Subhashis Banerjee1 and Roy Fleischmann10, 1Bristol Myers Squibb, Princeton, NJ, 2Bristol-Myers Squibb, Morrisville, PA, 3University of Occupational and Environmental Health, Kitakyusyu Fukuoka, Japan, 4Hospital for Special Surgery, New York, NY, 5Leiden University Medical Center, Leiden, Netherlands, 6Instituto de Rehabilitación Psicofísica (IREP), Buenos Aires, Argentina, 7Johns Hopkins University, Baltimore, MD, 8Bristol Myers Squibb GmbH & Co. KGaA, Munich, Germany, 9Leeds Institute of Rheumatic and Musculoskeletal Medicine, University of Leeds, Leeds, United Kingdom, 10University of Texas Southwestern Medical Center and Metroplex Clinical Research Center, Dallas, TX
Background/Purpose: Inhibition of structural joint damage progression is a key outcome measure in RA clinical trials. This can be assessed by progression of joint erosion score (ES) and by an increase in the number of erosive joints (EJ). We evaluated the effects of subcutaneous (SC) abatacept (ABA) treatment over 52 weeks (wks) on structural damage using these measures as well as clinical response in MTX-naive ACPA+ patients (pts) with early RA in a phase 3b study (AVERT-2; NCT02504268).1
Methods: ACPA+ pts with early RA (ACR/EULAR 2010)2 were randomized to SC ABA 125 mg once weekly or SC ABA placebo (PBO), both with oral MTX for 56 wks. In this post hoc analysis, all study pts with X-rays (baseline [BL] and wk 52) and select clinical outcomes available were included. BL and wk 52 X-ray data were evaluated; EJ was assessed and graded by blinded central readers for ES using modified total Sharp/van der Heijde score.3 For ES, average scores from 2 independent radiologists were calculated; for EJ, data from all joints identified by either of the 2 raters were included. Changes from BL ES and EJ (≤ 0 [non-progressors] and > 0 [progressors]) were compared in ABA + MTX vs PBO + MTX treatment arms. In addition, clinical outcomes (Simplified Disease Activity Index [SDAI] remission [≤ 3.3], DAS28 [CRP] < 2.6, and clinical improvement [≥ 80% improvement in SDAI or DAS28 (CRP)])4 were assessed at wk 52.
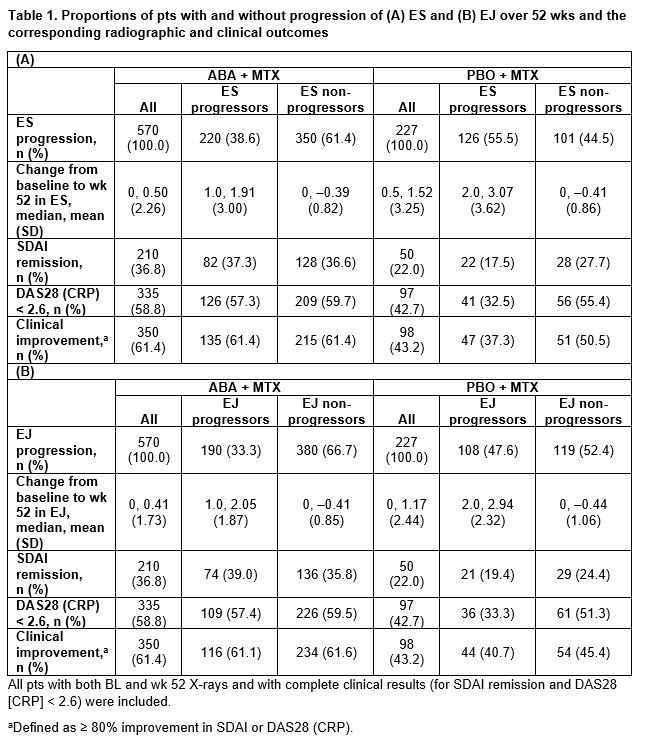
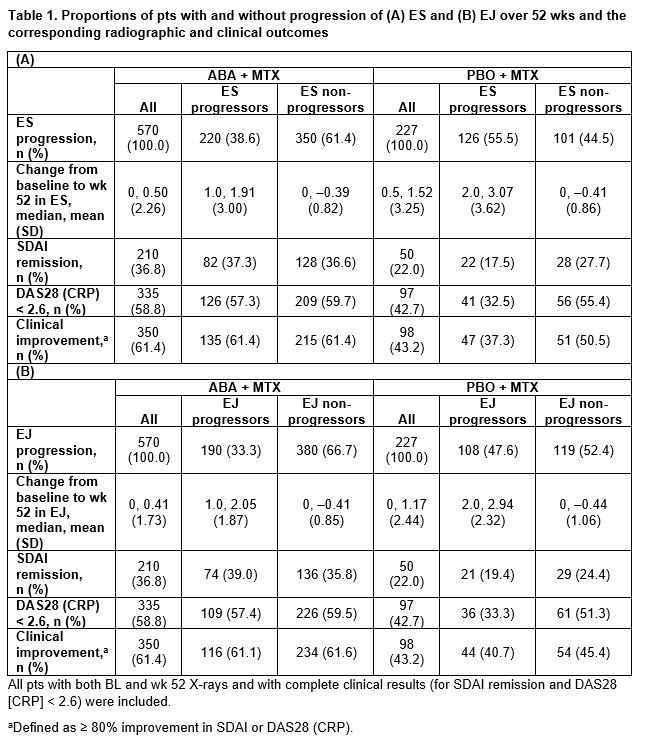
Results: The proportions of progressors by ES and EJ scoring were higher in the PBO + MTX vs the ABA + MTX arm (ES, 55.5 vs 38.6%; EJ, 47.6 vs 33.3%; respectively; Table 1A and 1B). The proportion of ES progressors was slightly higher (Table 1A) than EJ progressors (Table 1B) in both arms. Over 52 wks, progression of structural damage from BL was numerically higher in the PBO + MTX vs the ABA + MTX arm among progressors (mean ES, 3.1 vs 1.9; mean EJ, 2.9 vs 2.1; respectively) and all pts (mean ES, 1.5 vs 0.5; mean EJ, 1.2 vs 0.4; respectively) (Table 1A and 1B). In the ABA + MTX arm, clinical outcomes were similar for progressors and non-progressors for both ES and EJ. In the PBO + MTX arm, clinical outcomes were better in non-progressors vs progressors, and were larger with ES than EJ (differences: ES, 10–23%; EJ, 5–18%; respectively; Table 1A and 1B).
Conclusion: In ACPA+ pts with early RA, abatacept provided similar clinical efficacy in pts with and without progression of structural damage. In contrast, in pts treated with MTX alone, the progression of structural damage over 52 wks was associated with worse clinical outcomes. Structural and clinical response rates were generally consistent between ES and EJ methodologies. Abatacept + MTX was more effective than MTX alone in reducing the progression of structural damage over 52 wks.
1Emery P, et al. Arthritis Rheum 2018;70:abs563.
2Aletaha D, et al. Arthritis Rheum2010;62:2569–2581.
3van der Heijde D. J Rheumatol2000;27:261–263.
4Smolen J, et al. Arthritis Res Ther 2019;21:231–239.
Medical writing: Fiona Boswell (Caudex), funded by Bristol Myers Squibb.
Disclosures: C. Pachai, Bristol Myers Squibb; S. Connolly, Bristol Myers Squibb; Y. Tanaka, Lilly, AbbVie, Bristol Myers Squibb, Chugai, Daiichi Sankyo, Eisai, Pfizer, Mitsubishi Tanabe, GlaxoSmithKline, Asahi Kasei, Takeda, Astellas, Janssen, Novartis, Sanofi, UCB, YL Biologics, MSD, Ono, Taisho Toyama, Celltrion, Gilead, Boehringer-Ingelheim, Corrona, Kowa, Amgen, AstraZeneca, AstraZeneca, Eli Lilly; V. Bykerk, Janssen, Bristol Myers Squibb, Crossbridge, Pfizer, Sanofi Aventis, Brainstorm Therapeutics, Amgen, UCB, Gilead, Genzyme Corporation, Regeneron; T. Huizinga, None; G. Citera, AbbVie, Amgen, Bristol Myers Squibb, Gema, Janssen, Pfizer, Sandoz, Boehringer Ingelheim; C. Bingham III, AbbVie, Janssen, Pfizer, Sanofi, Bristol Myers Squibb, Eli Lilly; S. Du, Bristol Myers Squibb; G. Hoexter, Bristol Myers Squibb GmbH & Co. KGaA; P. Emery, AbbVie, Amgen, Bristol Myers Squibb, Celltrion, Eli Lilly, Gilead, Novartis, Pfizer, Roche, Samsung; S. Banerjee, Bristol Myers Squibb; R. Fleischmann, AbbVie, Amgen, Bristol Myers Squibb, Eli Lilly, Galvani, Gilead, GlaxoSmithKline, Janssen, Novartis, Pfizer, UCB, Galapagos.
Background/Purpose: Inhibition of structural joint damage progression is a key outcome measure in RA clinical trials. This can be assessed by progression of joint erosion score (ES) and by an increase in the number of erosive joints (EJ). We evaluated the effects of subcutaneous (SC) abatacept (ABA) treatment over 52 weeks (wks) on structural damage using these measures as well as clinical response in MTX-naive ACPA+ patients (pts) with early RA in a phase 3b study (AVERT-2; NCT02504268).1
Methods: ACPA+ pts with early RA (ACR/EULAR 2010)2 were randomized to SC ABA 125 mg once weekly or SC ABA placebo (PBO), both with oral MTX for 56 wks. In this post hoc analysis, all study pts with X-rays (baseline [BL] and wk 52) and select clinical outcomes available were included. BL and wk 52 X-ray data were evaluated; EJ was assessed and graded by blinded central readers for ES using modified total Sharp/van der Heijde score.3 For ES, average scores from 2 independent radiologists were calculated; for EJ, data from all joints identified by either of the 2 raters were included. Changes from BL ES and EJ (≤ 0 [non-progressors] and > 0 [progressors]) were compared in ABA + MTX vs PBO + MTX treatment arms. In addition, clinical outcomes (Simplified Disease Activity Index [SDAI] remission [≤ 3.3], DAS28 [CRP] < 2.6, and clinical improvement [≥ 80% improvement in SDAI or DAS28 (CRP)])4 were assessed at wk 52.
Results: The proportions of progressors by ES and EJ scoring were higher in the PBO + MTX vs the ABA + MTX arm (ES, 55.5 vs 38.6%; EJ, 47.6 vs 33.3%; respectively; Table 1A and 1B). The proportion of ES progressors was slightly higher (Table 1A) than EJ progressors (Table 1B) in both arms. Over 52 wks, progression of structural damage from BL was numerically higher in the PBO + MTX vs the ABA + MTX arm among progressors (mean ES, 3.1 vs 1.9; mean EJ, 2.9 vs 2.1; respectively) and all pts (mean ES, 1.5 vs 0.5; mean EJ, 1.2 vs 0.4; respectively) (Table 1A and 1B). In the ABA + MTX arm, clinical outcomes were similar for progressors and non-progressors for both ES and EJ. In the PBO + MTX arm, clinical outcomes were better in non-progressors vs progressors, and were larger with ES than EJ (differences: ES, 10–23%; EJ, 5–18%; respectively; Table 1A and 1B).
Conclusion: In ACPA+ pts with early RA, abatacept provided similar clinical efficacy in pts with and without progression of structural damage. In contrast, in pts treated with MTX alone, the progression of structural damage over 52 wks was associated with worse clinical outcomes. Structural and clinical response rates were generally consistent between ES and EJ methodologies. Abatacept + MTX was more effective than MTX alone in reducing the progression of structural damage over 52 wks.
1Emery P, et al. Arthritis Rheum 2018;70:abs563.
2Aletaha D, et al. Arthritis Rheum2010;62:2569–2581.
3van der Heijde D. J Rheumatol2000;27:261–263.
4Smolen J, et al. Arthritis Res Ther 2019;21:231–239.
Medical writing: Fiona Boswell (Caudex), funded by Bristol Myers Squibb.
Disclosures: C. Pachai, Bristol Myers Squibb; S. Connolly, Bristol Myers Squibb; Y. Tanaka, Lilly, AbbVie, Bristol Myers Squibb, Chugai, Daiichi Sankyo, Eisai, Pfizer, Mitsubishi Tanabe, GlaxoSmithKline, Asahi Kasei, Takeda, Astellas, Janssen, Novartis, Sanofi, UCB, YL Biologics, MSD, Ono, Taisho Toyama, Celltrion, Gilead, Boehringer-Ingelheim, Corrona, Kowa, Amgen, AstraZeneca, AstraZeneca, Eli Lilly; V. Bykerk, Janssen, Bristol Myers Squibb, Crossbridge, Pfizer, Sanofi Aventis, Brainstorm Therapeutics, Amgen, UCB, Gilead, Genzyme Corporation, Regeneron; T. Huizinga, None; G. Citera, AbbVie, Amgen, Bristol Myers Squibb, Gema, Janssen, Pfizer, Sandoz, Boehringer Ingelheim; C. Bingham III, AbbVie, Janssen, Pfizer, Sanofi, Bristol Myers Squibb, Eli Lilly; S. Du, Bristol Myers Squibb; G. Hoexter, Bristol Myers Squibb GmbH & Co. KGaA; P. Emery, AbbVie, Amgen, Bristol Myers Squibb, Celltrion, Eli Lilly, Gilead, Novartis, Pfizer, Roche, Samsung; S. Banerjee, Bristol Myers Squibb; R. Fleischmann, AbbVie, Amgen, Bristol Myers Squibb, Eli Lilly, Galvani, Gilead, GlaxoSmithKline, Janssen, Novartis, Pfizer, UCB, Galapagos.

