Back
Poster Session C
Imaging
Session: (1228–1266) Imaging of Rheumatic Diseases Poster
1235: Fibroblast Activation in Psoriasis Patients Assessed by 68Ga-FAPI-04 PET-CT Is Associated with Progression to Psoriatic Arthritis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- FF
Filippo Fagni, MD
University clinic of Erlangen and Friedrich Alexander Universität Erlangen-Nürnberg
Erlangen, Germany
Abstract Poster Presenter(s)
Filippo Fagni1, David Simon2, Arnd Kleyer2, Koray Tascilar2, Jule Taubmann3, Sara Bayat1, Ioanna Minopoulou3, Melek Yalcin Mutlu3, Armin Atzinger4, Torsten Kuwert4, Georg Schett5 and Chrstian Schmidkonz4, 1University Hospital Erlangen; Department of Internal Medicine 3 - Rheumatology and Immunology, Erlangen, Germany, 2Department of Internal Medicine 3 – Rheumatology and Immunology, Friedrich-Alexander-University Erlangen-Nürnberg and Universitätsklinikum Erlangen, 91054 Erlangen, Germany; Deutsches Zentrum Immuntherapie, Friedrich-Alexander-UniversityErlangen-Nürnberg and Universitätsklinikum Erlangen, Erlangen, Germany, 3University Hospital Erlangen, Department of Internal Medicine 3 - Rheumatology and Immunology, Erlangen, Germany, 4Friedrich-Alexander University (FAU) Erlangen-Nuremberg, Erlangen, Germany, 5Universitätsklinikum Erlangen, Erlangen, Germany
Background/Purpose: Prevalence of subclinical inflammatory lesions is high in patients with cutaneous psoriasis and constitutes a -risk constellation for the development of psoriatic arthritis (PsA)1. However, reliable identification of patients at risk for the transition to PsA remains a challenge, as no molecular marker for progression has yet been identified. 68Ga-labelled selective inhibitor of fibroblast activation protein-α (68Ga-FAPI-04) PET-CT imaging is an advanced imaging modality, which uses a radiotracer targeting fibroblast activation protein, allowing the in vivo and non-invasive visualization of fibroblast activity2. Since synovial and entheseal fibroblasts are abnormally activated in PsA3, we speculated that psoriasis patients at risk for developing PsA could be reliably identified by 68Ga-FAPI-04 PET-CT.
Purpose: To identify patterns of 68Ga-FAPI-04 PET-CT activity associated with an increased risk of developing PsA in a longitudinal cohort of patients affected by cutaneous psoriasis.
Methods: A small cohort of patients with cutaneous psoriasis without any clinical signs of PsA (no arthritis/enthesitis/dactylitis/axial involvement) underwent 68Ga-FAPI-04 PET-CT and were followed-up prospectively to assess the development of PsA according to the CASPAR criteria. At baseline and follow-up all patients received clinical investigation for the presence of musculoskeletal disease (tender/swollen joint count (66/68), clinical assessment of 29 entheseal sites, assessment of dactylitis and of clinical symptoms of inflammatory back pain). In addition, skin disease-specific characteristics (disease duration, psoriasis subtype, presence of nail and scalp involvement) were recorded. 68Ga-FAPI-04 PET-CT images were assessed for the presence of radiotracer uptake at synovial and entheseal sites. Increased radioactivity compared with the background uptake was defined as being positive.
Results: Ten psoriasis patients (6 women/4 men) received 68Ga-FAPI-04 PET-CT (Table 1). Seven patients showed 68Ga-FAPI-04 uptake at synovio-entheseal sites (finger joints, shoulders, knees, tarsus, lumbar facet joints and interspinous ligaments, greater trochanter, ischial tuberosity). Six (85.7%) patients with synovio-entheseal 68Ga-FAPI-04 uptake progressed to PsA. The median PsA-free survival time was 207 (160-240) days (Figure 1). All three patients with a negative imaging developed no signs of PsA after a median follow-up of 301 (301-489) days.
Conclusion: The presence of articular fibroblast activation in psoriasis patients is associated with an increased risk of developing PsA. Fibroblast activity detected by 68Ga-FAPI-04 PET-CT could be a potential molecular biomarker for defining patients at high risk for transition to PsA. However, as the size of this cohort of psoriasis patients is very small further analyses will be necessary to corroborate these findings.
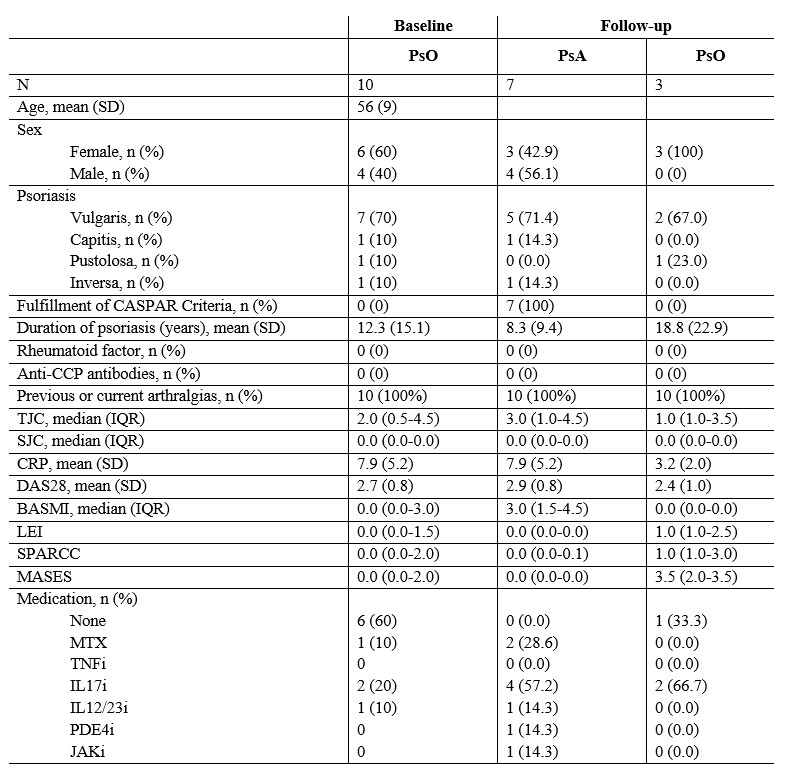 Table 1 – Patient demographic and clinical characteristic at baseline and follow-up
Table 1 – Patient demographic and clinical characteristic at baseline and follow-up
SD: standard deviation; IQR: interquartile range; PsO: psoriasis; PsA: psoriatic arthritis; CASPAR: classification criteria for psoriatic arthritis; CCP: cyclic citrullinated peptide; TJC: tender joint count; SJC: swollen joint count; CRP: C-reactive protein; BASMI: Bath ankylosing spondylitis metrology index; LEI: Leeds enthesitis index; SPARCC: Spondyloarthritis Research Consortium of Canada; MASES: Maastrich Ankylosing Spondylitis Enthesitis Score; MTX: methotrexate; TNFi: tumor necrosis factor inhibition; IL17i: interleukin 17 inhibition; IL12/23i; interleukin 12/23 inhibition, PDE4i: phosphodiesterase 4 inhibition; JAKi; JAK inhibition.
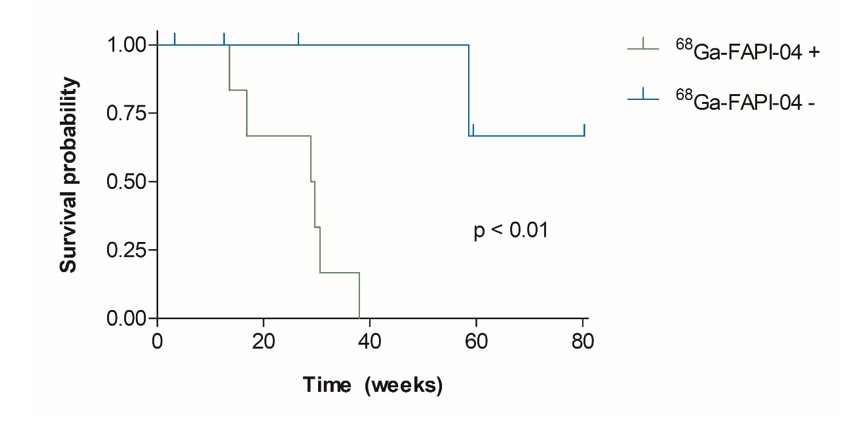 Figure 1 – Kaplan–Meier plots of PsA-free survival according to the presence or absence of any synovio-entheseal 68Ga-FAPI-04 uptake (p < 0.01).
Figure 1 – Kaplan–Meier plots of PsA-free survival according to the presence or absence of any synovio-entheseal 68Ga-FAPI-04 uptake (p < 0.01).
Disclosures: F. Fagni, None; D. Simon, None; A. Kleyer, None; K. Tascilar, Gılead, AbbVie/Abbott, UCB, Eli Lilly; J. Taubmann, None; S. Bayat, None; I. Minopoulou, None; M. Yalcin Mutlu, None; A. Atzinger, None; T. Kuwert, None; G. Schett, None; C. Schmidkonz, None.
Background/Purpose: Prevalence of subclinical inflammatory lesions is high in patients with cutaneous psoriasis and constitutes a -risk constellation for the development of psoriatic arthritis (PsA)1. However, reliable identification of patients at risk for the transition to PsA remains a challenge, as no molecular marker for progression has yet been identified. 68Ga-labelled selective inhibitor of fibroblast activation protein-α (68Ga-FAPI-04) PET-CT imaging is an advanced imaging modality, which uses a radiotracer targeting fibroblast activation protein, allowing the in vivo and non-invasive visualization of fibroblast activity2. Since synovial and entheseal fibroblasts are abnormally activated in PsA3, we speculated that psoriasis patients at risk for developing PsA could be reliably identified by 68Ga-FAPI-04 PET-CT.
Purpose: To identify patterns of 68Ga-FAPI-04 PET-CT activity associated with an increased risk of developing PsA in a longitudinal cohort of patients affected by cutaneous psoriasis.
Methods: A small cohort of patients with cutaneous psoriasis without any clinical signs of PsA (no arthritis/enthesitis/dactylitis/axial involvement) underwent 68Ga-FAPI-04 PET-CT and were followed-up prospectively to assess the development of PsA according to the CASPAR criteria. At baseline and follow-up all patients received clinical investigation for the presence of musculoskeletal disease (tender/swollen joint count (66/68), clinical assessment of 29 entheseal sites, assessment of dactylitis and of clinical symptoms of inflammatory back pain). In addition, skin disease-specific characteristics (disease duration, psoriasis subtype, presence of nail and scalp involvement) were recorded. 68Ga-FAPI-04 PET-CT images were assessed for the presence of radiotracer uptake at synovial and entheseal sites. Increased radioactivity compared with the background uptake was defined as being positive.
Results: Ten psoriasis patients (6 women/4 men) received 68Ga-FAPI-04 PET-CT (Table 1). Seven patients showed 68Ga-FAPI-04 uptake at synovio-entheseal sites (finger joints, shoulders, knees, tarsus, lumbar facet joints and interspinous ligaments, greater trochanter, ischial tuberosity). Six (85.7%) patients with synovio-entheseal 68Ga-FAPI-04 uptake progressed to PsA. The median PsA-free survival time was 207 (160-240) days (Figure 1). All three patients with a negative imaging developed no signs of PsA after a median follow-up of 301 (301-489) days.
Conclusion: The presence of articular fibroblast activation in psoriasis patients is associated with an increased risk of developing PsA. Fibroblast activity detected by 68Ga-FAPI-04 PET-CT could be a potential molecular biomarker for defining patients at high risk for transition to PsA. However, as the size of this cohort of psoriasis patients is very small further analyses will be necessary to corroborate these findings.
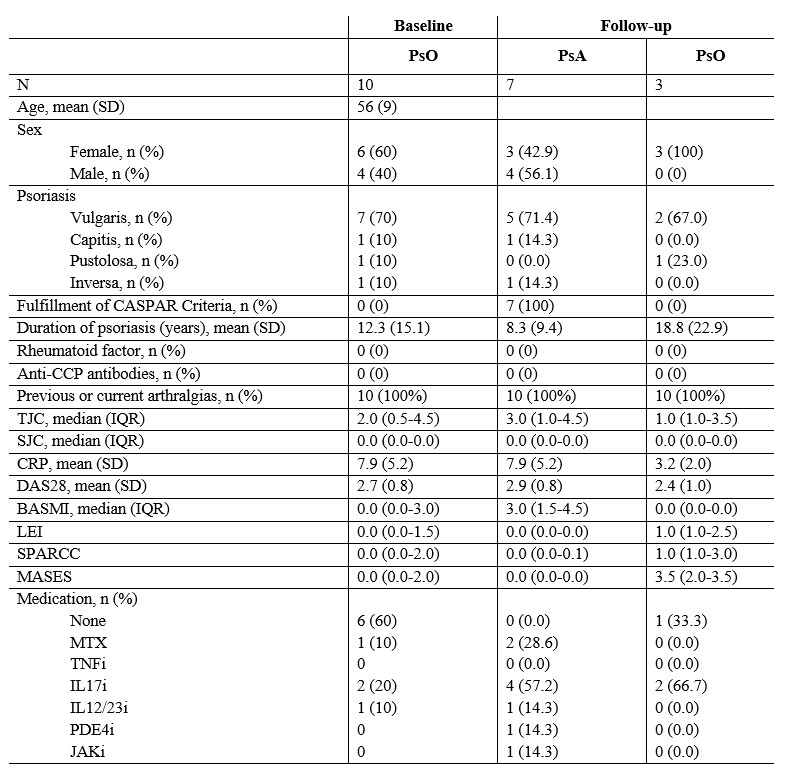 Table 1 – Patient demographic and clinical characteristic at baseline and follow-up
Table 1 – Patient demographic and clinical characteristic at baseline and follow-upSD: standard deviation; IQR: interquartile range; PsO: psoriasis; PsA: psoriatic arthritis; CASPAR: classification criteria for psoriatic arthritis; CCP: cyclic citrullinated peptide; TJC: tender joint count; SJC: swollen joint count; CRP: C-reactive protein; BASMI: Bath ankylosing spondylitis metrology index; LEI: Leeds enthesitis index; SPARCC: Spondyloarthritis Research Consortium of Canada; MASES: Maastrich Ankylosing Spondylitis Enthesitis Score; MTX: methotrexate; TNFi: tumor necrosis factor inhibition; IL17i: interleukin 17 inhibition; IL12/23i; interleukin 12/23 inhibition, PDE4i: phosphodiesterase 4 inhibition; JAKi; JAK inhibition.
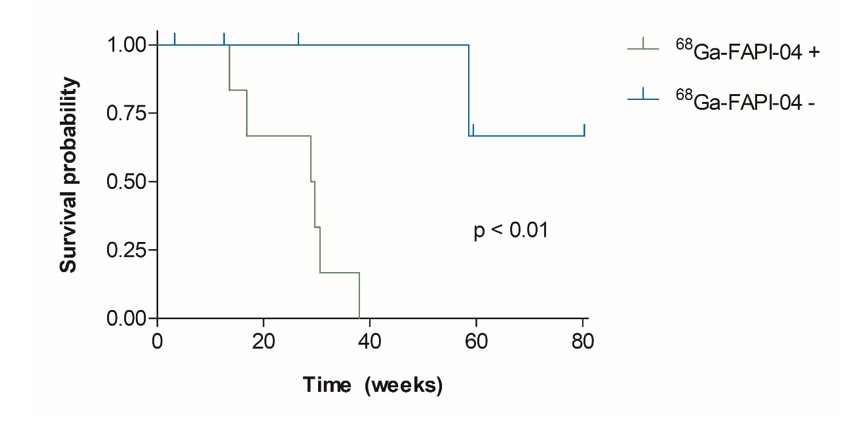 Figure 1 – Kaplan–Meier plots of PsA-free survival according to the presence or absence of any synovio-entheseal 68Ga-FAPI-04 uptake (p < 0.01).
Figure 1 – Kaplan–Meier plots of PsA-free survival according to the presence or absence of any synovio-entheseal 68Ga-FAPI-04 uptake (p < 0.01).Disclosures: F. Fagni, None; D. Simon, None; A. Kleyer, None; K. Tascilar, Gılead, AbbVie/Abbott, UCB, Eli Lilly; J. Taubmann, None; S. Bayat, None; I. Minopoulou, None; M. Yalcin Mutlu, None; A. Atzinger, None; T. Kuwert, None; G. Schett, None; C. Schmidkonz, None.

