Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1445: Gastrointestinal Manifestations in Systemic Lupus Erythematosus Are Associated with High Disease Activity and Mortality: A Nationwide Cohort Study from India
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
.jpg)
Pankti Mehta, MD, MBBS, DM
King George's Medical Univeristy
Lucknow, Uttar Pradesh, India
Abstract Poster Presenter(s)
Pankti Mehta1, Akansha Srivastava2, Amita Aggarwal2, Liza Rajasekhar3, Vineetha Shobha4, Chengappa Kavadichanda5, ASHISH JACOB MATHEW6, Parasar Ghosh7, Bidyut Das8, Avinash Jain9, Ranjan Gupta10 and Manish Rathi11, 1King George's Medical University, Lucknow, India, 2Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India, 3Nizam's Institute of Medical Sciences, Madhapur, India, 4St. John’s Medical College Hospital, Bangalore, India, 5JIPMER, Pondicherry, Puducherry, India, 6Christian Medical College, Vellore, Vellore, India, 7Govt of West Bengal, Kolkata, India, Kolkata, West Bengal, India, 8SCB medical college, Cuttack, India, 9SMS Medical College, Lucknow, India, 10All India Institute of Medical Sciences, New Delhi, India, 11PGIMER Chandigarh, Chandigarh, India
Background/Purpose: Gastrointestinal (GI) manifestations of Systemic Lupus Erythematosus (SLE) although rare are often severe. These are difficult to directly attribute to SLE as they can also be associated with drugs, infections and other organ manifestations of SLE. There is a paucity of prospective data on the prevalence, associations and outcomes of GI manifestations in SLE. Thus, we studied the GI manifestations in a prospectively enrolled nationwide cohort of SLE in India.
Methods: Cases with GI manifestations (defined as per BILAG) along with controls (one on either side of the case based on the serial number of recruitment into the cohort; one on either side of the block for consecutive cases) were selected from the database of a nationwide, prospective, multicenter cohort (INSPIRE) of patients with SLE (classified by SLICC classification criteria). Data on demographics, clinical features, investigations, disease activity at baseline and early outcomes were retrieved for analysis.
Data are expressed as mean ± standard deviation and SPSS was used for statistical analysis. Univariate analysis was done using the t-test and chi-square test based on the type of variables; those with a p-value of ≤0.1 were included for multivariate analysis using the forward likelihood test.
Results: Of 2210 patients with SLE enrolled in the INSPIRE registry, 254(11.5%) had GI manifestations, with more than one GI feature in 39 patients. The most common was ascites (193,76%) followed by lupus enteritis (35, 13.8%), lupus pancreatitis (32, 12.6), lupus hepatitis (19, 7.5), lupus peritonitis (6, 2.3), intestinal obstruction and lupus cholecystitis (3, 1.2%) with malabsorption and protein losing enteropathy being the least common (2, 0.7%). The majority were observed within 2.2±3.3 months of presentation with 97(38%) being present at the onset.
On univariate analysis, patients with GI manifestations were significantly younger; had a higher frequency of fever, lupus nephritis, psychosis, seizures and pleural effusion; were more likely to have anemia, lymphopenia, thrombocytopenia, elevated creatinine, low albumin and low complements as compared to controls. There was no difference in the serology between the two groups. SLEDAI 2K and the BILAG score were higher in the cases. (Table 1)
On multivariate analysis, younger age [p=0.03, 0.97(0.95-0.99,)]; high creatinine [0.001, 1.6(1.2-2.1)], low albumin [0.0001, 0.6(0.5-0.8)], presence of pleural effusion [0.0001, 3.3(1.9-5.2)], presence of thrombocytopenia [0.02, 1.6(1.1-2.5)] were significantly associated with GI features. (Figure 1)
Mortality was higher in the cases [10.3 and 5.5%, p=0.04, 1.9(1.1-3.7)] as compared to controls. (Table 1)
Conclusion: GI manifestations were observed in 11.5% of the cohort with ascites being the most common feature. GI involvement is associated with higher disease activity and mortality.
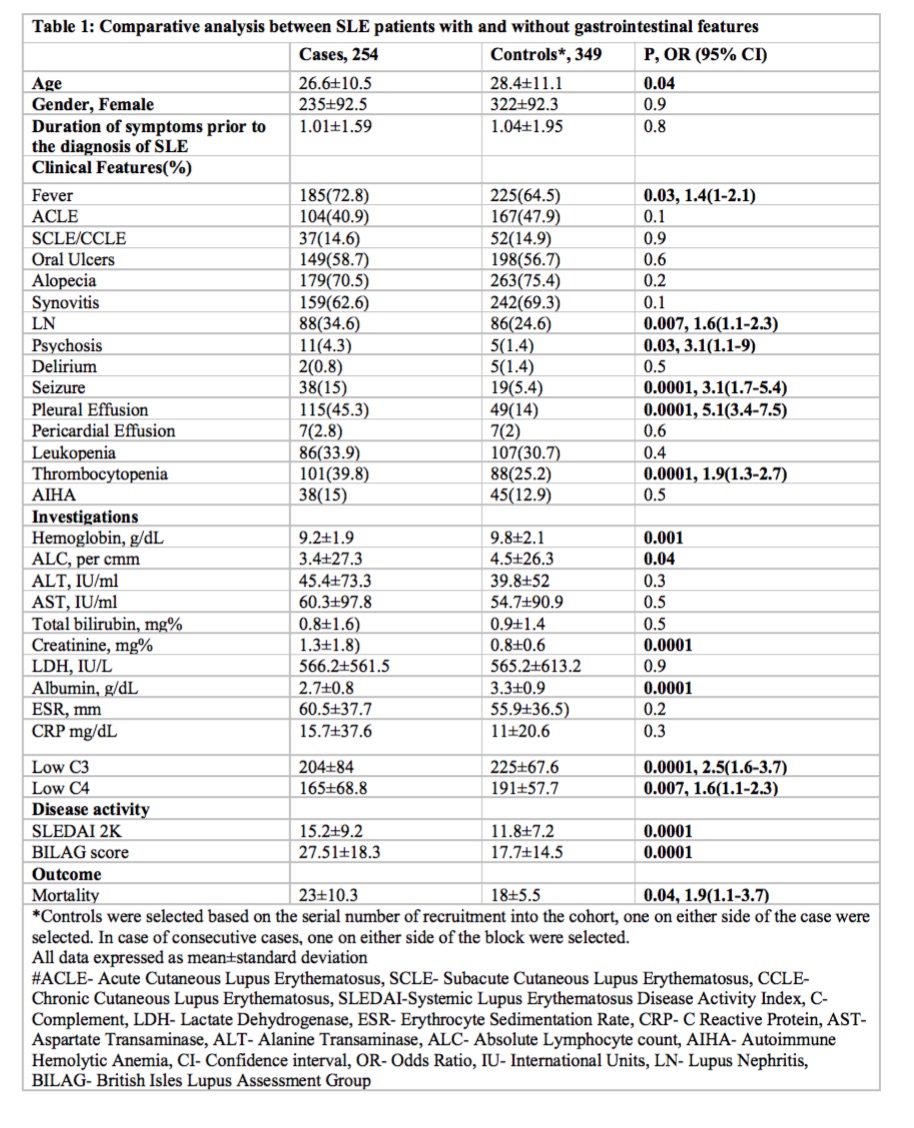
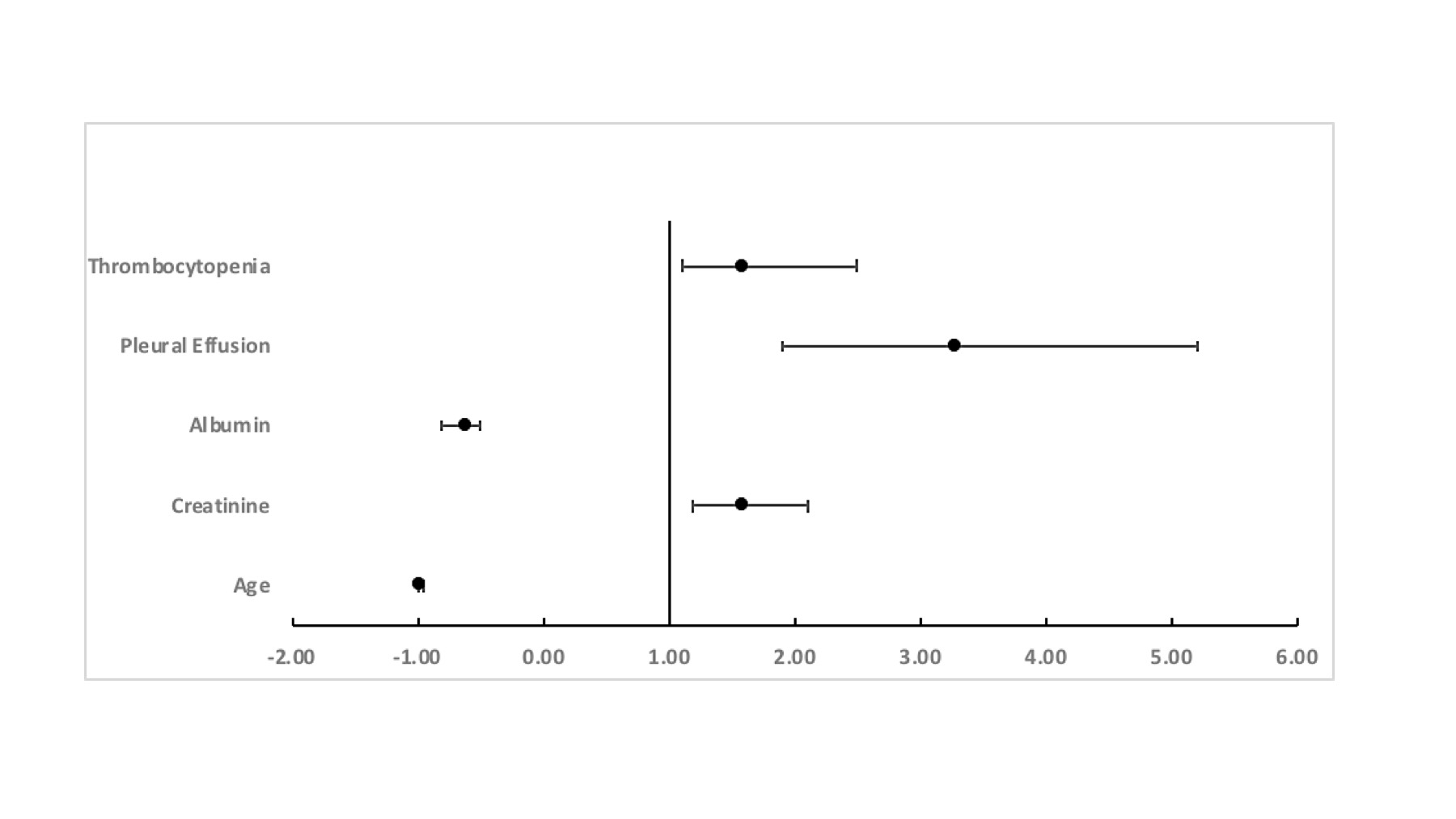 Figure 1: Association of gastrointestinal manifestations on multivariate analysis as compared with controls
Figure 1: Association of gastrointestinal manifestations on multivariate analysis as compared with controls
Disclosures: P. Mehta, None; A. Srivastava, None; A. Aggarwal, None; L. Rajasekhar, None; V. Shobha, None; C. Kavadichanda, None; A. MATHEW, None; P. Ghosh, None; B. Das, None; A. Jain, None; R. Gupta, None; M. Rathi, None.
Background/Purpose: Gastrointestinal (GI) manifestations of Systemic Lupus Erythematosus (SLE) although rare are often severe. These are difficult to directly attribute to SLE as they can also be associated with drugs, infections and other organ manifestations of SLE. There is a paucity of prospective data on the prevalence, associations and outcomes of GI manifestations in SLE. Thus, we studied the GI manifestations in a prospectively enrolled nationwide cohort of SLE in India.
Methods: Cases with GI manifestations (defined as per BILAG) along with controls (one on either side of the case based on the serial number of recruitment into the cohort; one on either side of the block for consecutive cases) were selected from the database of a nationwide, prospective, multicenter cohort (INSPIRE) of patients with SLE (classified by SLICC classification criteria). Data on demographics, clinical features, investigations, disease activity at baseline and early outcomes were retrieved for analysis.
Data are expressed as mean ± standard deviation and SPSS was used for statistical analysis. Univariate analysis was done using the t-test and chi-square test based on the type of variables; those with a p-value of ≤0.1 were included for multivariate analysis using the forward likelihood test.
Results: Of 2210 patients with SLE enrolled in the INSPIRE registry, 254(11.5%) had GI manifestations, with more than one GI feature in 39 patients. The most common was ascites (193,76%) followed by lupus enteritis (35, 13.8%), lupus pancreatitis (32, 12.6), lupus hepatitis (19, 7.5), lupus peritonitis (6, 2.3), intestinal obstruction and lupus cholecystitis (3, 1.2%) with malabsorption and protein losing enteropathy being the least common (2, 0.7%). The majority were observed within 2.2±3.3 months of presentation with 97(38%) being present at the onset.
On univariate analysis, patients with GI manifestations were significantly younger; had a higher frequency of fever, lupus nephritis, psychosis, seizures and pleural effusion; were more likely to have anemia, lymphopenia, thrombocytopenia, elevated creatinine, low albumin and low complements as compared to controls. There was no difference in the serology between the two groups. SLEDAI 2K and the BILAG score were higher in the cases. (Table 1)
On multivariate analysis, younger age [p=0.03, 0.97(0.95-0.99,)]; high creatinine [0.001, 1.6(1.2-2.1)], low albumin [0.0001, 0.6(0.5-0.8)], presence of pleural effusion [0.0001, 3.3(1.9-5.2)], presence of thrombocytopenia [0.02, 1.6(1.1-2.5)] were significantly associated with GI features. (Figure 1)
Mortality was higher in the cases [10.3 and 5.5%, p=0.04, 1.9(1.1-3.7)] as compared to controls. (Table 1)
Conclusion: GI manifestations were observed in 11.5% of the cohort with ascites being the most common feature. GI involvement is associated with higher disease activity and mortality.
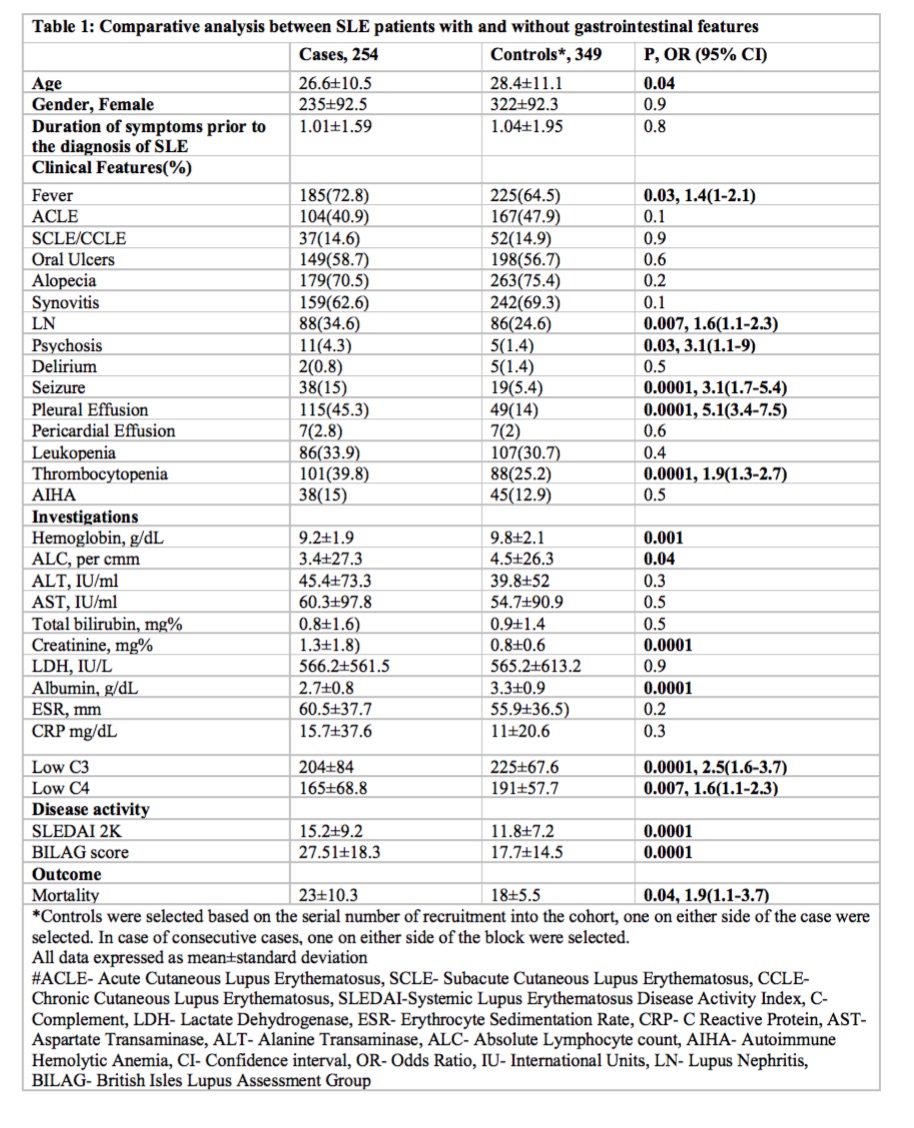
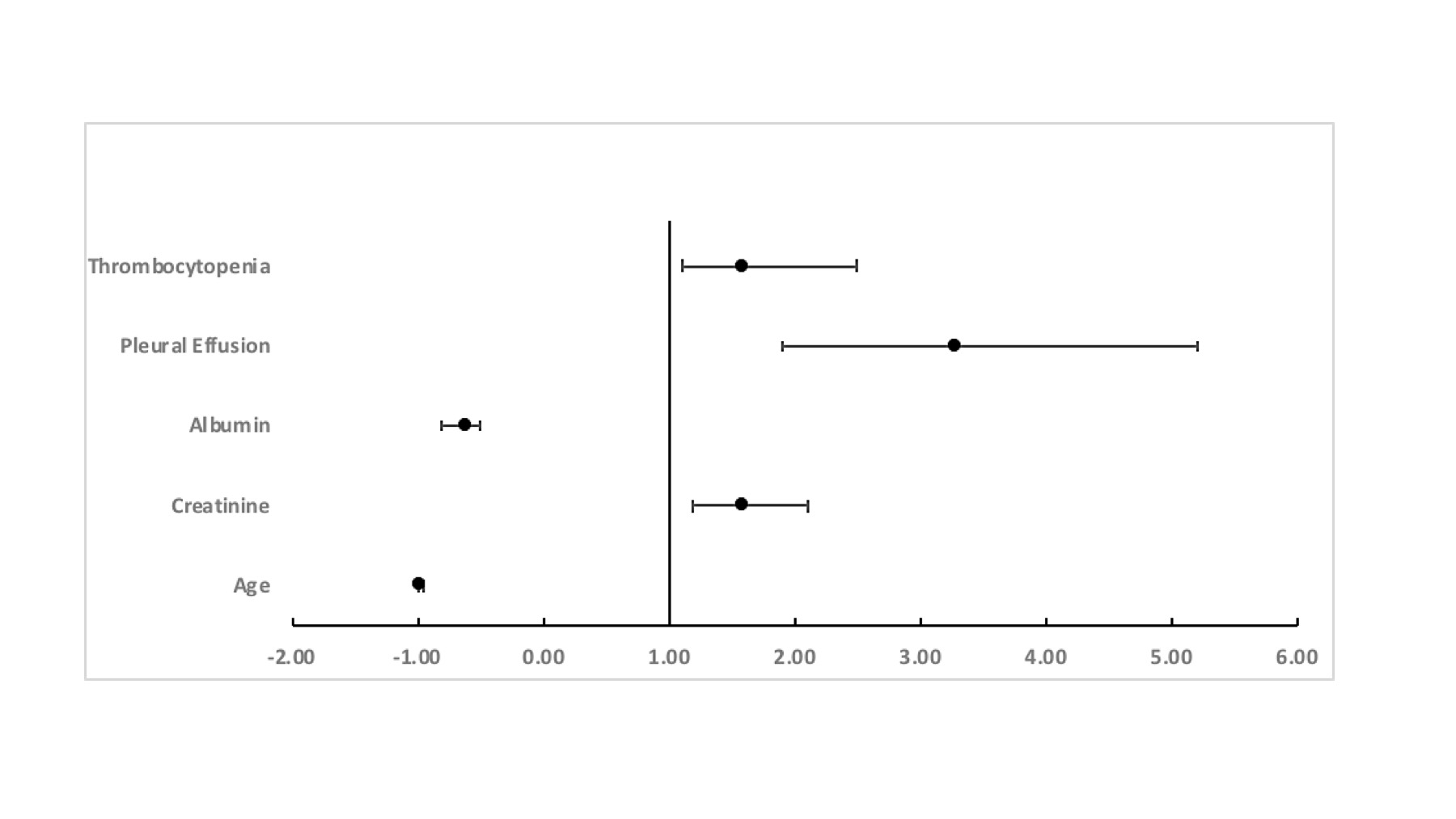 Figure 1: Association of gastrointestinal manifestations on multivariate analysis as compared with controls
Figure 1: Association of gastrointestinal manifestations on multivariate analysis as compared with controlsDisclosures: P. Mehta, None; A. Srivastava, None; A. Aggarwal, None; L. Rajasekhar, None; V. Shobha, None; C. Kavadichanda, None; A. MATHEW, None; P. Ghosh, None; B. Das, None; A. Jain, None; R. Gupta, None; M. Rathi, None.

