Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1332–1359) Patient Outcomes, Preferences, and Attitudes Poster II
1352: Improving Completion Rates of Routine Mental Health Screening for Depression and Anxiety in Paediatric Lupus Outpatient Clinic to Enhance Patient Mental Health Care
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Tala El Tal, MD
University of Toronto/Hospital for Sick Children
Toronto, ON, Canada
Abstract Poster Presenter(s)
Tala El Tal1, Avery Longmore2, Abdulaziz el Mutairi1, Amani Al Bijadi1, Audrea Chen1, Holly Convery1, Dinah Finkelstein3, Linda Hiraki4, Chetana Kulkarni5, Justine Ledochowski6, Neely Lerman1, Karen Leslie7, Deborah Levy8, Sharon Lorber9, Jayne MacMahon10, Jeanine McColl11, Sarah Mossad12, Oscar Mwizerwa10, Lawrence Ng12, Luana Flores Pereira12, Vandana Rawal7, Alaa Shehab1, Evelyn Smith13, Alene Toulany14 and Andrea Knight1, 1The Hospital for Sick Children, Division of Rheumatology, Department of Paediatrics, University of Toronto, Toronto, ON, Canada, 2The Hospital for Sick Children, Department of Paediatrics, University of Toronto, Toronto, ON, Canada, 3The Hospital for Sick Children, Department of Paediatrics, University of Toronto, ON, Canada, Toronto, ON, Canada, 4The Hospital for Sick Children, Division of Rheumatology, Department of Paediatrics, University of Toronto, Genetics and Genome Biology, SickKids Research Institute, Toronto, ON, Canada, 5The Hospital for Sick Children, Division of Child & Youth Mental Health, Department of Psychiatry, University of Toronto, Toronto, ON, Canada, 6The Hospital for Sick Children, Department of Psychology, University of Toronto, Toronto, ON, Canada, 7The Hospital for Sick Children, Division of Adolescent Medicine, Department of Paediatrics, University of Toronto, Toronto, ON, Canada, 8Division of Rheumatology, The Hospital for Sick Children; Child Health Evaluative Services, SickKids Research Institute; Department of Paediatrics, University of Toronto, Toronto, ON, Canada, 9The Hospital for Sick Children, Factor Inwentash Faculty of Social Work, University of Toronto, Toronto, ON, Canada, 10The Hospital for Sick Children, Division of Rheumatology, Department of Paediatrics, Toronto, ON, Canada, 11University of Toronto, Toronto, ON, Canada, 12The Hospital for Sick Children, Toronto, ON, Canada, 13The Hospital for Sick Children, Division of Psychiatry, Department of Paediatrics, University of Toronto,, Toronto, ON, Canada, 14The Hospital for Sick Children, Division of Adolescent Medicine, Department of Paediatrics, University of Toronto,, Toronto, ON, Canada
Background/Purpose: Mental health (MH) problems are prevalent in adolescents with childhood-onset lupus (cSLE), with cross-sectional studies estimating prevalences of 20-60% for depression symptoms and 20-40% for anxiety symptoms. Despite this, MH screening rates are low. Identifying and treating MH symptoms early on is crucial, as they are known to be associated with poor outcomes such as poor adherence to care and quality of life. We aimed to: 1) increase rate of lupus patient (≥ 12-18 yo with no known prior diagnosis of depression and/or anxiety disorder) routine MH screening for depression (Patient Health Questionnaire-9 (PHQ-9)) and anxiety (Generalized Anxiety Disorder-7 (GAD-7)) from 17% to 80%, and if positive, 2) increase percentage of documented initial management (psychoeducation and/or referral to appropriate MH service(s)) from 22% to 80% in pediatric lupus clinic by Sep 2022.
Methods: A multi-disciplinary quality improvement (QI) team (rheumatology, adolescent medicine, social work, psychiatry, and neuropsychology) used electronic health record (EHR) documentation to retrospectively calculate baseline rates of documented depression and anxiety screening using PHQ-4 from July 2021-Dec 2021. We used fishbone diagram/5Whys/Pareto Chart to identify root causes for poor MH routine screening. We developed patient and parent satisfaction surveys to incorporate their experiences. We used the Plan-Do-Study Act (PDSA) method of QI to systematically evaluate and adjust our process in real time, initiated in Feb 2022. The primary outcome measure was the percentage of cSLE patients with documented PHQ-9 and GAD-7 screening since initiation.
Results: The median percentage of cSLE patients with documented PHQ-4 screening at baseline was 17%. The vital few root causes identified included 1) limited MH resources, 2) lack of integration of MH screening into clinic workflow, 3) lack of standardized clinic algorithm for positive screens, 4) lack of MH training of health care providers, and 5) patient/family stigma and misconceptions. Accordingly, change ideas included having patients self-screen using PHQ-9 and GAD-7 instead of health care providers (Figure 1) . A standardized clinical algorithm was developed to manage screening scores (Figure 2). We provided two 2-hour MH workshops to health care providers with emphasis on MH burden, screening tools, suicide risk assessment and safety planning. Over 50% of patients (n= 23) and parents (n=18) surveyed felt comfortable with routine MH screening, preferably in-person, and supported ongoing MH inquiry at future visits. Patients emphasized privacy and confidentiality. Thus far, 37 cSLE patients were screened, of which 59% (n=16) and 30% (n=11) had positive screens on PHQ-9 and/or GAD-7 respectively, of whom 25% (n=4) and 18% (n=2) had at least moderate scores respectively. Six cSLE patients were referred and seen by appropriate MH service. Majority screened (n=36) received psychoeducation and MH handout.
Conclusion: Routine formal depression and anxiety screening is feasible in a busy subspecialty clinic. Next steps include ongoing screening, and ensuring appropriate follow-up plan for positive screened patients.
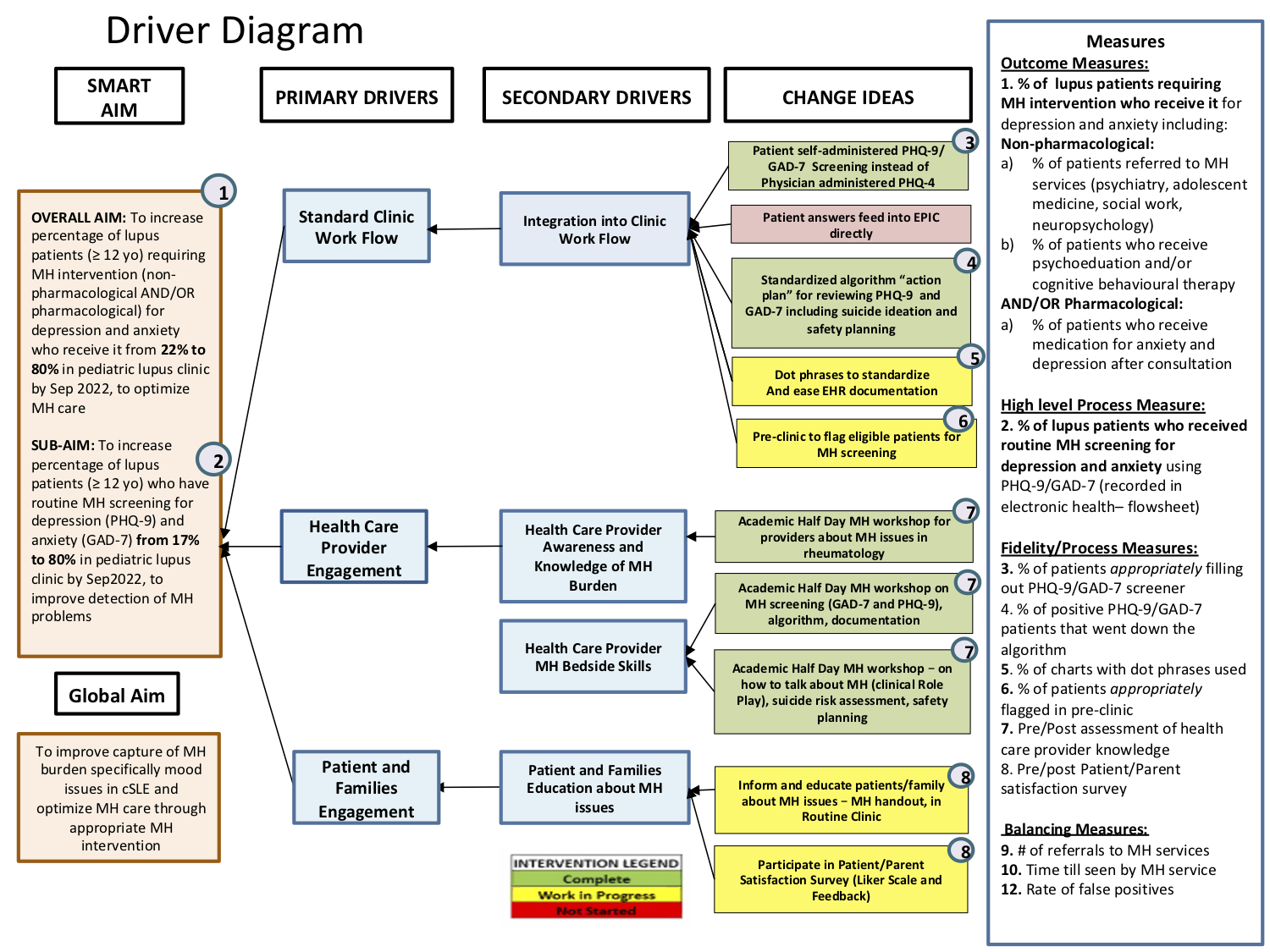 Figure 1: Driver Diagram – this includes aims, primary and secondary drivers, change ideas, and measures (outcome, process, and balancing measures).
Figure 1: Driver Diagram – this includes aims, primary and secondary drivers, change ideas, and measures (outcome, process, and balancing measures).
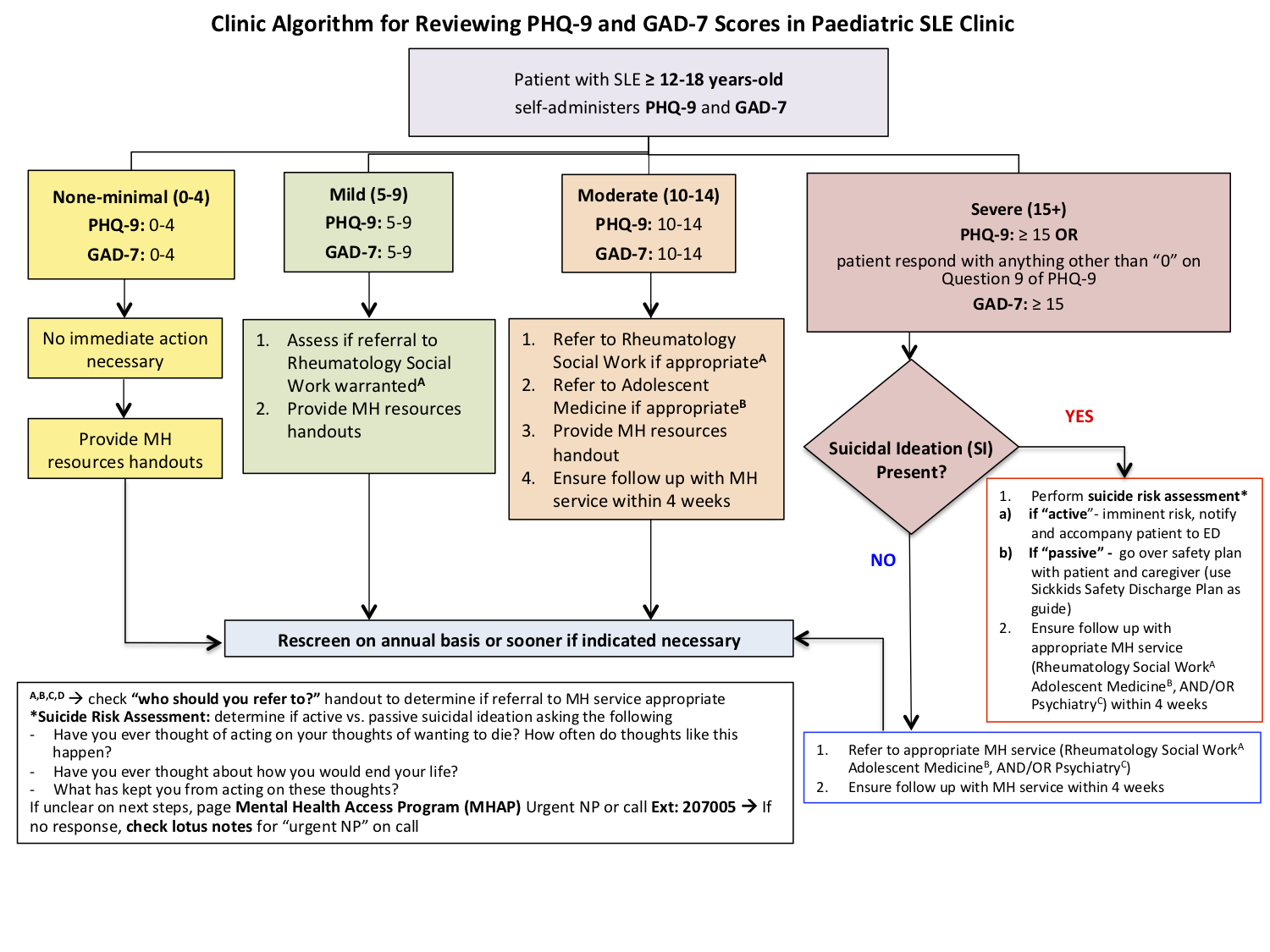 Figure 2: Clinic Algorithm used to assess and review scores from the PHQ-9 and GAD-7 Mental Health (MH) screening, categorized into none-minimal (0-4), mild (5-9), moderate (10-14), and severe (+15).
Figure 2: Clinic Algorithm used to assess and review scores from the PHQ-9 and GAD-7 Mental Health (MH) screening, categorized into none-minimal (0-4), mild (5-9), moderate (10-14), and severe (+15).
Disclosures: T. El Tal, None; A. Longmore, None; A. el Mutairi, None; A. Al Bijadi, None; A. Chen, None; H. Convery, None; D. Finkelstein, None; L. Hiraki, None; C. Kulkarni, None; J. Ledochowski, None; N. Lerman, None; K. Leslie, None; D. Levy, None; S. Lorber, None; J. MacMahon, None; J. McColl, None; S. Mossad, None; O. Mwizerwa, None; L. Ng, None; L. Flores Pereira, None; V. Rawal, None; A. Shehab, None; E. Smith, None; A. Toulany, None; A. Knight, None.
Background/Purpose: Mental health (MH) problems are prevalent in adolescents with childhood-onset lupus (cSLE), with cross-sectional studies estimating prevalences of 20-60% for depression symptoms and 20-40% for anxiety symptoms. Despite this, MH screening rates are low. Identifying and treating MH symptoms early on is crucial, as they are known to be associated with poor outcomes such as poor adherence to care and quality of life. We aimed to: 1) increase rate of lupus patient (≥ 12-18 yo with no known prior diagnosis of depression and/or anxiety disorder) routine MH screening for depression (Patient Health Questionnaire-9 (PHQ-9)) and anxiety (Generalized Anxiety Disorder-7 (GAD-7)) from 17% to 80%, and if positive, 2) increase percentage of documented initial management (psychoeducation and/or referral to appropriate MH service(s)) from 22% to 80% in pediatric lupus clinic by Sep 2022.
Methods: A multi-disciplinary quality improvement (QI) team (rheumatology, adolescent medicine, social work, psychiatry, and neuropsychology) used electronic health record (EHR) documentation to retrospectively calculate baseline rates of documented depression and anxiety screening using PHQ-4 from July 2021-Dec 2021. We used fishbone diagram/5Whys/Pareto Chart to identify root causes for poor MH routine screening. We developed patient and parent satisfaction surveys to incorporate their experiences. We used the Plan-Do-Study Act (PDSA) method of QI to systematically evaluate and adjust our process in real time, initiated in Feb 2022. The primary outcome measure was the percentage of cSLE patients with documented PHQ-9 and GAD-7 screening since initiation.
Results: The median percentage of cSLE patients with documented PHQ-4 screening at baseline was 17%. The vital few root causes identified included 1) limited MH resources, 2) lack of integration of MH screening into clinic workflow, 3) lack of standardized clinic algorithm for positive screens, 4) lack of MH training of health care providers, and 5) patient/family stigma and misconceptions. Accordingly, change ideas included having patients self-screen using PHQ-9 and GAD-7 instead of health care providers (Figure 1) . A standardized clinical algorithm was developed to manage screening scores (Figure 2). We provided two 2-hour MH workshops to health care providers with emphasis on MH burden, screening tools, suicide risk assessment and safety planning. Over 50% of patients (n= 23) and parents (n=18) surveyed felt comfortable with routine MH screening, preferably in-person, and supported ongoing MH inquiry at future visits. Patients emphasized privacy and confidentiality. Thus far, 37 cSLE patients were screened, of which 59% (n=16) and 30% (n=11) had positive screens on PHQ-9 and/or GAD-7 respectively, of whom 25% (n=4) and 18% (n=2) had at least moderate scores respectively. Six cSLE patients were referred and seen by appropriate MH service. Majority screened (n=36) received psychoeducation and MH handout.
Conclusion: Routine formal depression and anxiety screening is feasible in a busy subspecialty clinic. Next steps include ongoing screening, and ensuring appropriate follow-up plan for positive screened patients.
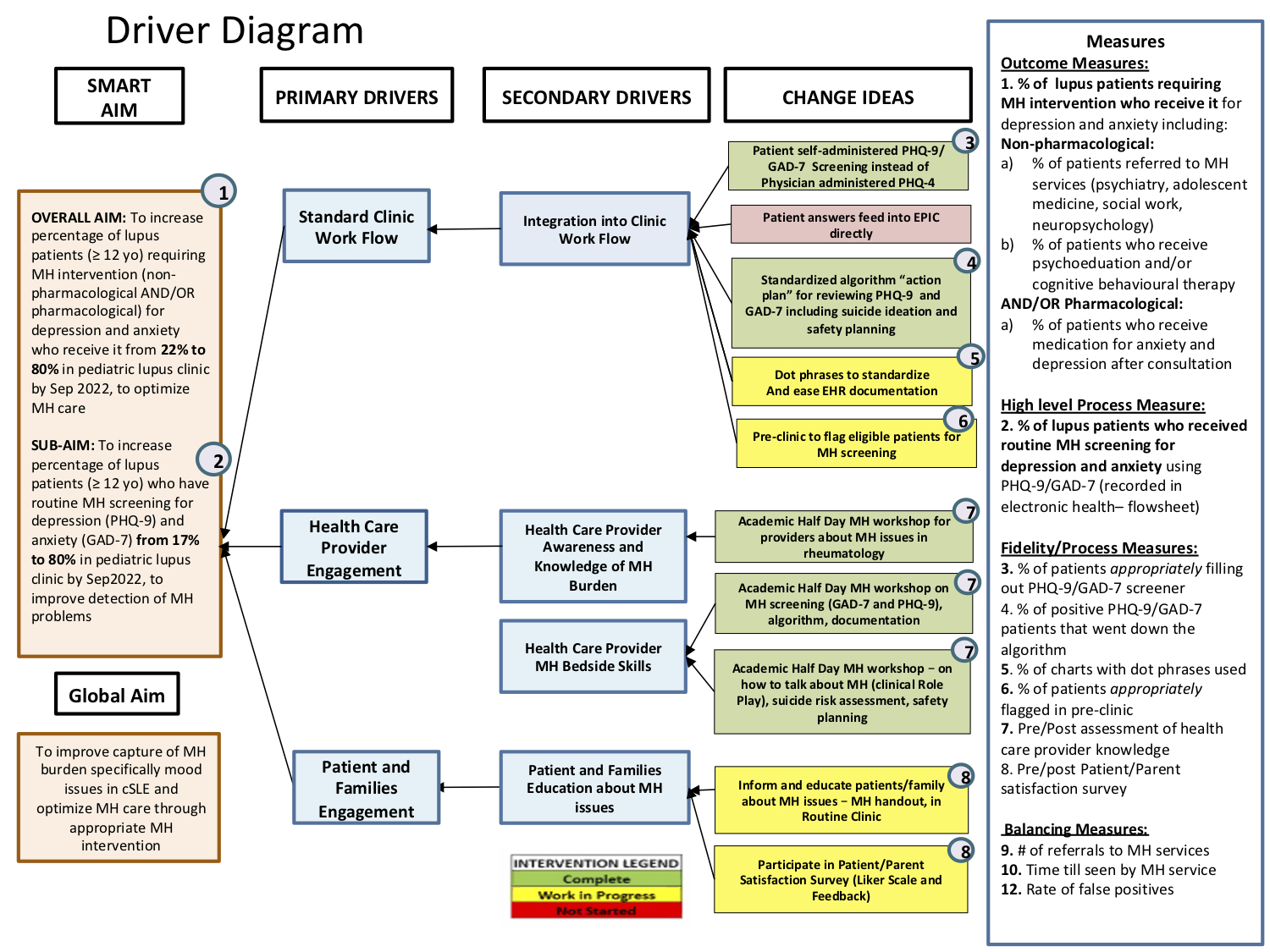 Figure 1: Driver Diagram – this includes aims, primary and secondary drivers, change ideas, and measures (outcome, process, and balancing measures).
Figure 1: Driver Diagram – this includes aims, primary and secondary drivers, change ideas, and measures (outcome, process, and balancing measures). 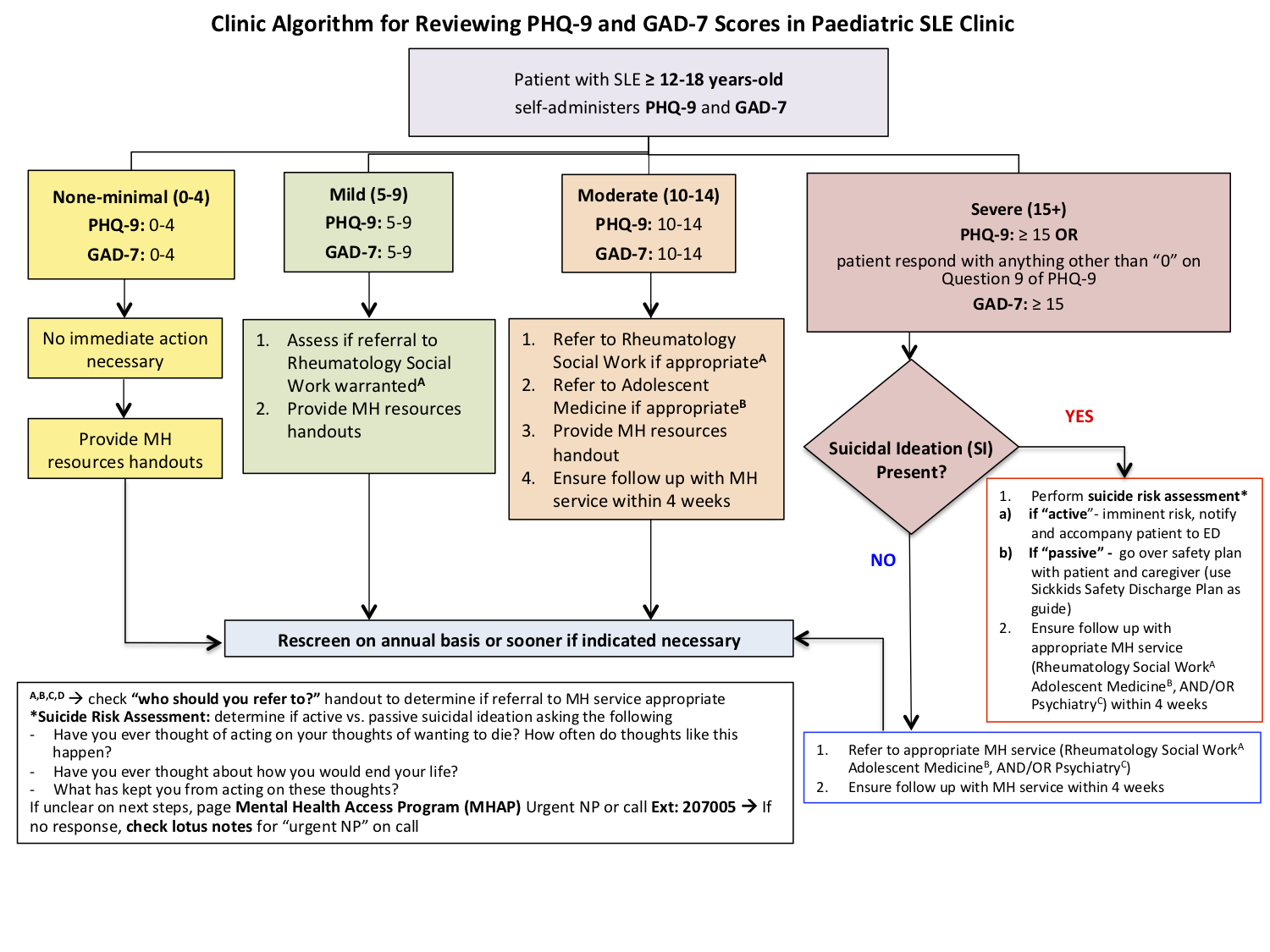 Figure 2: Clinic Algorithm used to assess and review scores from the PHQ-9 and GAD-7 Mental Health (MH) screening, categorized into none-minimal (0-4), mild (5-9), moderate (10-14), and severe (+15).
Figure 2: Clinic Algorithm used to assess and review scores from the PHQ-9 and GAD-7 Mental Health (MH) screening, categorized into none-minimal (0-4), mild (5-9), moderate (10-14), and severe (+15). Disclosures: T. El Tal, None; A. Longmore, None; A. el Mutairi, None; A. Al Bijadi, None; A. Chen, None; H. Convery, None; D. Finkelstein, None; L. Hiraki, None; C. Kulkarni, None; J. Ledochowski, None; N. Lerman, None; K. Leslie, None; D. Levy, None; S. Lorber, None; J. MacMahon, None; J. McColl, None; S. Mossad, None; O. Mwizerwa, None; L. Ng, None; L. Flores Pereira, None; V. Rawal, None; A. Shehab, None; E. Smith, None; A. Toulany, None; A. Knight, None.

