Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1267–1303) Measures and Measurement of Healthcare Quality Poster
1290: Inflammation Is More Prominent Than Joint Damage at Initial Visits of Patients with Inflammatory Arthritides, but Organ Damage and Patient Distress Are as Prominent in Overall Rheumatology Care: Data from a Feasible Physician RheuMetric Checklist
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JS
Juan Schmukler, MD
Rush University Medical Center
Chicago, IL, United States
Abstract Poster Presenter(s)
Juan Schmukler1, Tengfei Li2, Joel Block1 and Theodore Pincus1, 1Rush University Medical Center, Chicago, IL, 2Georgetown University, Washington, DC
Background/Purpose: Most widely-used rheumatology indices, e.g., DAS28, CDAI, SLEDAI, ASDAS, DAPSA, reflect the mission of rheumatologists to control inflammatory activity (INF) to prevent subsequent organ damage. These indices function effectively in selected patients in clinical trials and other clinical research, which generally include only a small minority of patients with any diagnosis. In routine care of unselected patients, the indices may be elevated in many patients by comorbid organ damage (DAM) and/or patient distress (STR), despite little or no inflammatory activity. Quantitative assessment of DAM and STR, as well as INF, is provided by a RheuMetric checklist, with 4 0-10 visual numeric scales (VNS) for physician global assessment (DOCGL), and an estimate of the proportion of DOCGL attributed to INF, DAM, and STR. We analyzed RheuMetric scores in patients at their initial visits and return visits at a rheumatology academic setting
Methods: A retrospective cross-sectional study was performed of RheuMetric checklist 0-10 VNS estimates for DOCGL and estimates of %INF, %DAM, and %STR (total=100%) completed in routine care by the treating rheumatologists. Mean levels of these estimates were analyzed according to primary diagnosis or diagnostic category of inflammatory rheumatic diseases (RA, SLE, SpA, vasculitis and gout), classified as at initial visits or return visits, using descriptive and chi-square statistics
Results: RheuMetric estimates required about 15 seconds to complete. At initial visits, mean DOCGL was 3.9 in all patients (range 3.0–4.9) (Table), attributed 62% to INF in inflammatory diseases, 72% to DAM in osteoarthritis (OA), and 74% to STR in fibromyalgia (FM) (p< 0.001), supporting face validity. In all patients at first visits, INF, DAM, and STR were estimated at 36%, 36%, and 28%, respectively (Table). At return visits, mean DOCGL was marginally lower (better) in inflammatory diseases, 3.7 vs 4.3, but similar in other diagnosis groups, 4.1 vs 3.9 in all patients. At return visits, mean DOCGL was attributed 33% to INF and 49% to DAM in inflammatory diseases, 69% to DAM in OA, and 68% to STR in FM(p< 0.001), while estimates in all patients of INF, DAM, and STR were 22%, 51% and 28%(p=0.05 vs initial visits), respectively (Table). Estimates of % DAM were increased in inflammatory disease diseases, other diagnoses and all patients (p< 0.05) (Table)
Conclusion: RheuMetric physician estimates for inflammation, damage, and patient distress have face validity as % INF, % DAM in OA, and % STR in FM. In patients with inflammatory diseases, DOCGL was attributed more to INF than DAM at first visits, but more to DAM than INF at return visits, reflecting highly effective anti-inflammatory treatments. In all patients, %INF, %DAM, and %STR were similar at first visits, but 50% DAM, 22% INF and 28% STR at return visits. While these findings may be expected, quantitative estimates of damage and distress, in addition to inflammation, may add to clinical decisions and explain why many patients may remain in moderate or high activity according to conventional rheumatology indices, which though considered to be sensitive only to inflammation, also reflect damage and distress.
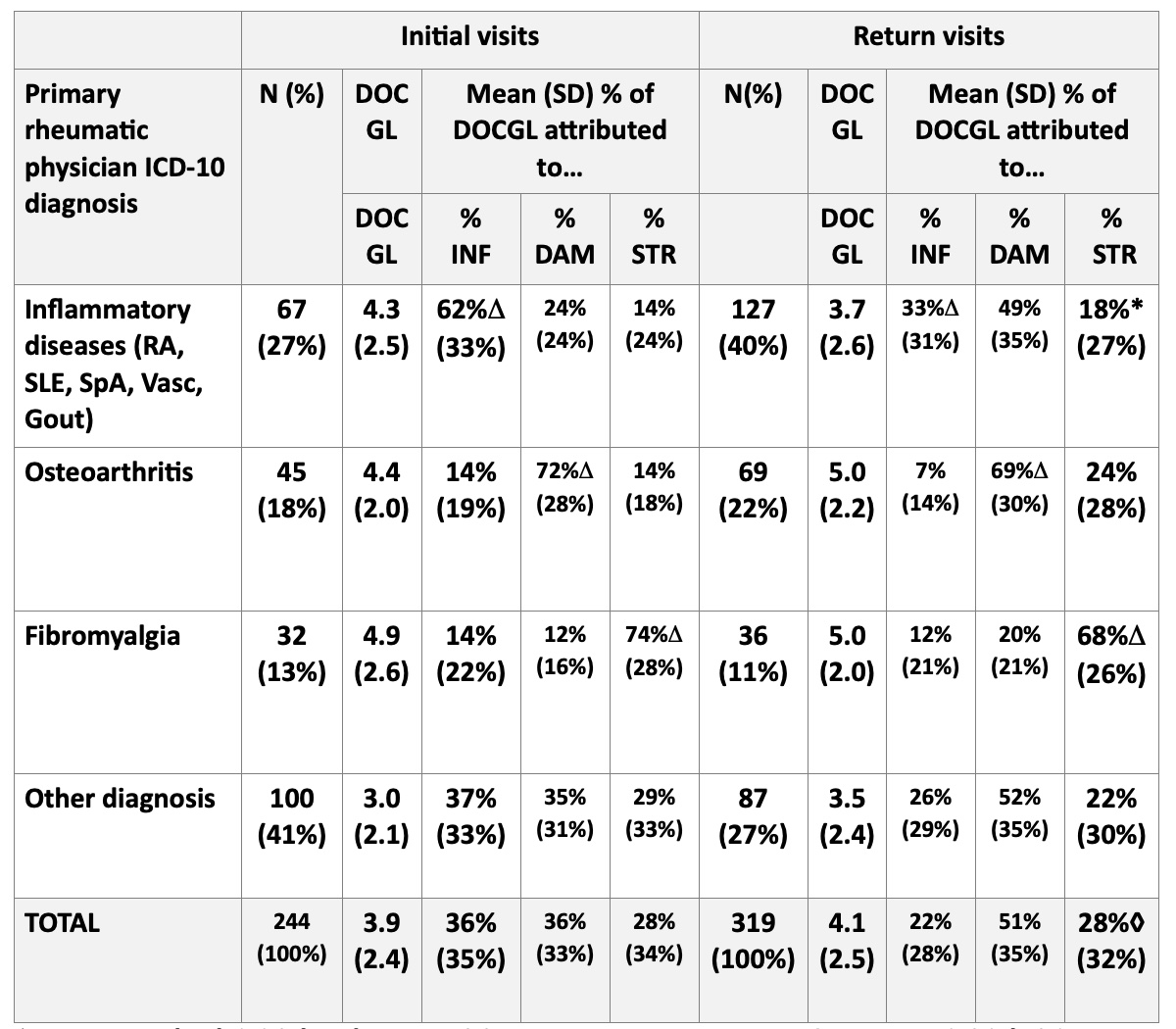 Table: Cross sectional analysis of mean (standard deviation) for 0-10 physician global estimate (DOCGL) and % of DOCGL attributed to inflammation (%INF), damage (%DAM), and patient distress (%STR) (Total=100%) at 244 initial visits compared to 319 return visits according to
Table: Cross sectional analysis of mean (standard deviation) for 0-10 physician global estimate (DOCGL) and % of DOCGL attributed to inflammation (%INF), damage (%DAM), and patient distress (%STR) (Total=100%) at 244 initial visits compared to 319 return visits according to
diagnosis or diagnostic group
Δ p < 0.001 at both initial and return visits. *p < 0.001 vs initial visits, ◊p=0.05 vs initial visits
Disclosures: J. Schmukler, None; T. Li, None; J. Block, None; T. Pincus, Medical History Services, LLC, Medical History Services LLC.
Background/Purpose: Most widely-used rheumatology indices, e.g., DAS28, CDAI, SLEDAI, ASDAS, DAPSA, reflect the mission of rheumatologists to control inflammatory activity (INF) to prevent subsequent organ damage. These indices function effectively in selected patients in clinical trials and other clinical research, which generally include only a small minority of patients with any diagnosis. In routine care of unselected patients, the indices may be elevated in many patients by comorbid organ damage (DAM) and/or patient distress (STR), despite little or no inflammatory activity. Quantitative assessment of DAM and STR, as well as INF, is provided by a RheuMetric checklist, with 4 0-10 visual numeric scales (VNS) for physician global assessment (DOCGL), and an estimate of the proportion of DOCGL attributed to INF, DAM, and STR. We analyzed RheuMetric scores in patients at their initial visits and return visits at a rheumatology academic setting
Methods: A retrospective cross-sectional study was performed of RheuMetric checklist 0-10 VNS estimates for DOCGL and estimates of %INF, %DAM, and %STR (total=100%) completed in routine care by the treating rheumatologists. Mean levels of these estimates were analyzed according to primary diagnosis or diagnostic category of inflammatory rheumatic diseases (RA, SLE, SpA, vasculitis and gout), classified as at initial visits or return visits, using descriptive and chi-square statistics
Results: RheuMetric estimates required about 15 seconds to complete. At initial visits, mean DOCGL was 3.9 in all patients (range 3.0–4.9) (Table), attributed 62% to INF in inflammatory diseases, 72% to DAM in osteoarthritis (OA), and 74% to STR in fibromyalgia (FM) (p< 0.001), supporting face validity. In all patients at first visits, INF, DAM, and STR were estimated at 36%, 36%, and 28%, respectively (Table). At return visits, mean DOCGL was marginally lower (better) in inflammatory diseases, 3.7 vs 4.3, but similar in other diagnosis groups, 4.1 vs 3.9 in all patients. At return visits, mean DOCGL was attributed 33% to INF and 49% to DAM in inflammatory diseases, 69% to DAM in OA, and 68% to STR in FM(p< 0.001), while estimates in all patients of INF, DAM, and STR were 22%, 51% and 28%(p=0.05 vs initial visits), respectively (Table). Estimates of % DAM were increased in inflammatory disease diseases, other diagnoses and all patients (p< 0.05) (Table)
Conclusion: RheuMetric physician estimates for inflammation, damage, and patient distress have face validity as % INF, % DAM in OA, and % STR in FM. In patients with inflammatory diseases, DOCGL was attributed more to INF than DAM at first visits, but more to DAM than INF at return visits, reflecting highly effective anti-inflammatory treatments. In all patients, %INF, %DAM, and %STR were similar at first visits, but 50% DAM, 22% INF and 28% STR at return visits. While these findings may be expected, quantitative estimates of damage and distress, in addition to inflammation, may add to clinical decisions and explain why many patients may remain in moderate or high activity according to conventional rheumatology indices, which though considered to be sensitive only to inflammation, also reflect damage and distress.
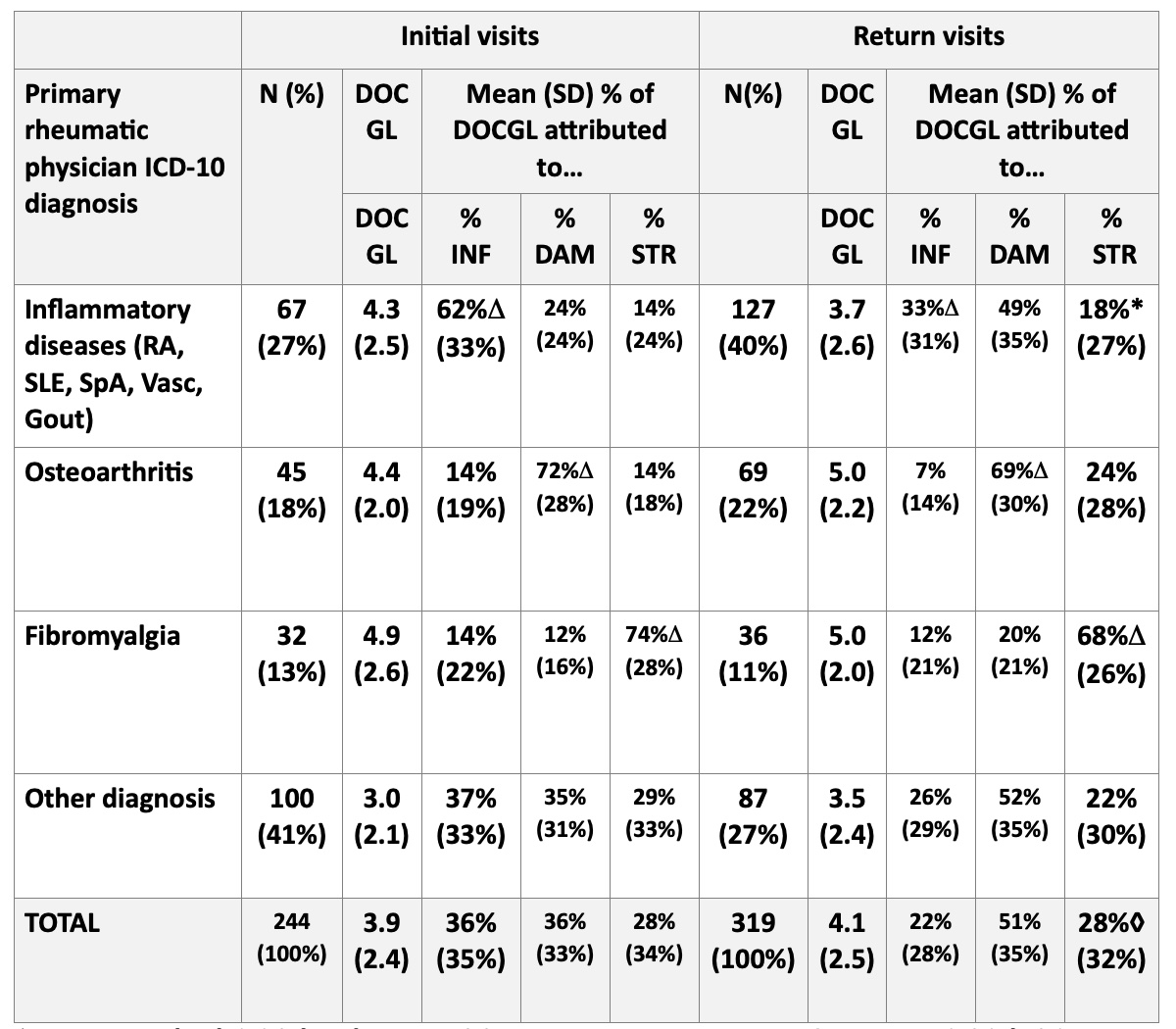 Table: Cross sectional analysis of mean (standard deviation) for 0-10 physician global estimate (DOCGL) and % of DOCGL attributed to inflammation (%INF), damage (%DAM), and patient distress (%STR) (Total=100%) at 244 initial visits compared to 319 return visits according to
Table: Cross sectional analysis of mean (standard deviation) for 0-10 physician global estimate (DOCGL) and % of DOCGL attributed to inflammation (%INF), damage (%DAM), and patient distress (%STR) (Total=100%) at 244 initial visits compared to 319 return visits according todiagnosis or diagnostic group
Δ p < 0.001 at both initial and return visits. *p < 0.001 vs initial visits, ◊p=0.05 vs initial visits
Disclosures: J. Schmukler, None; T. Li, None; J. Block, None; T. Pincus, Medical History Services, LLC, Medical History Services LLC.

