Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1186–1214) Epidemiology and Public Health Poster II
1196: Interaction of Cumulative Inflammation with Smoking and Lipids in Risk Modification of Dementia Among Patients with Rheumatoid Arthritis: A Population-based Cohort Study
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- CK
Chanakya Kodishala, MBBS
Mayo Clinic Rochester Minnesota
Rochester, MN, United States
Abstract Poster Presenter(s)
Chanakya Kodishala1, Stephanie Duong2, Cassondra Hulshizer2, Ryan Lennon2, Rabia Javed2, Maria Vassilaki2, Michelle Mielke3, John Davis2, Cynthia Crowson4 and Elena Myasoedova2, 1Mayo Clinic Rochester Minnesota, Rochester, MN, 2Mayo Clinic, Rochester, MN, 3Wake Forest University School of Medicine, Winston-Salem, NC, 4Mayo Clinic, Eyota, MN
Background/Purpose: Patients with rheumatoid arthritis (RA) have increased risk of developing dementia. Systemic inflammation is implicated in the pathogenesis of cognitive decline. However, the association between inflammatory markers and dementia is inconsistent. Also, it is unclear whether inflammation directly contributes to dementia pathology or exerts its effects through other modifiable risk factors. We aimed to study the interaction of inflammatory burden with smoking and lipids as risk modifiers for dementia in an inception cohort of RA.
Methods: This retrospective population-based cohort study included residents of a geographical area who were ≥50 years when they met 1987 ACR criteria for incident RA in 1980-2014. All patients were followed until death/migration or 12/31/2019. Those with dementia before RA incidence were excluded (n=12). Incident dementia was defined as two relevant ICD-9/10 codes at least 30 days apart. Data on socio-demographics, rheumatoid factor (RF)/anti-cyclic citrullinated peptide (anti-CCP) positivity, smoking (current and former), cardio/cerebrovascular disease (CVD), erythrocyte sedimentation rate (ESR), and lipid measures were abstracted from medical records. Cumulative inflammatory burden was estimated by applying the most recent ESR value to each day of follow-up and summing these values. CVD was defined as coronary heart disease/ischemic stroke/CVD death/intermittent claudication/heart failure. Cox models with time-dependent covariates were used to examine association between cumulative ESR and dementia, adjusting for age, sex, and year of RA incidence. Interactions between cumulative ESR or highest ESR in the first year of RA and smoking or lipid measures, i.e., total cholesterol, low and high-density lipoprotein cholesterol (LDL, HDL), triglycerides were also assessed.
Results: The study included 886 patients with RA (mean age 65 years, 65% females, 95% Whites); 63% were RF/anti-CCP positive. While cumulative ESR was not associated with development of dementia (HR 1.03, 95% CI 0.97-1.09) in the total sample, it was significantly associated with increased risk of dementia among smokers (interaction p=0.03; Figure). Adjusting for CVD, the interaction effect persisted but was no longer statistically significant. In patients with seropositive RA, cumulative ESR and ever smoking interacted to increase the risk of dementia (p=0.04). There was a statistically significant interaction between the highest ESR in the first year of RA and baseline LDL (p=0.02), wherein high LDL was associated with increased risk of dementia among patients with normal ESR but with decreased risk of dementia among those with high ESR. No such interactions were found for other lipid measures.
Conclusion: Cumulative inflammation interacts with smoking, resulting in increased risk of dementia. Similarly, there is an interaction between highest ESR and LDL on the risk of dementia. Lipids may have paradoxical association with risk of dementia in RA with potential implications for dementia risk estimation in patients with elevated ESR. Our findings highlight the important role of modifiable risk factors and systemic inflammation in the pathogenesis of dementia in patients with RA.
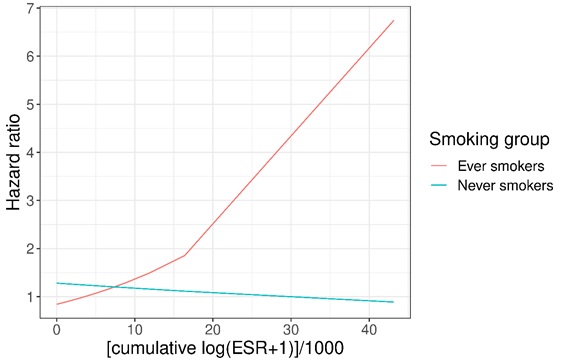 Figure: Interaction of cumulative ESR and smoking
Figure: Interaction of cumulative ESR and smoking
Disclosures: C. Kodishala, None; S. Duong, None; C. Hulshizer, None; R. Lennon, None; R. Javed, None; M. Vassilaki, F. Hoffmann-La Roche, Biogen, F. Hoffmann-La Roche, Avobis Bio, LLC., Amgen, Abbott Laboratories, Johnson and Johnson, Medtronic, AbbVie; M. Mielke, LabCorp, Biogen; J. Davis, Pfizer; C. Crowson, None; E. Myasoedova, None.
Background/Purpose: Patients with rheumatoid arthritis (RA) have increased risk of developing dementia. Systemic inflammation is implicated in the pathogenesis of cognitive decline. However, the association between inflammatory markers and dementia is inconsistent. Also, it is unclear whether inflammation directly contributes to dementia pathology or exerts its effects through other modifiable risk factors. We aimed to study the interaction of inflammatory burden with smoking and lipids as risk modifiers for dementia in an inception cohort of RA.
Methods: This retrospective population-based cohort study included residents of a geographical area who were ≥50 years when they met 1987 ACR criteria for incident RA in 1980-2014. All patients were followed until death/migration or 12/31/2019. Those with dementia before RA incidence were excluded (n=12). Incident dementia was defined as two relevant ICD-9/10 codes at least 30 days apart. Data on socio-demographics, rheumatoid factor (RF)/anti-cyclic citrullinated peptide (anti-CCP) positivity, smoking (current and former), cardio/cerebrovascular disease (CVD), erythrocyte sedimentation rate (ESR), and lipid measures were abstracted from medical records. Cumulative inflammatory burden was estimated by applying the most recent ESR value to each day of follow-up and summing these values. CVD was defined as coronary heart disease/ischemic stroke/CVD death/intermittent claudication/heart failure. Cox models with time-dependent covariates were used to examine association between cumulative ESR and dementia, adjusting for age, sex, and year of RA incidence. Interactions between cumulative ESR or highest ESR in the first year of RA and smoking or lipid measures, i.e., total cholesterol, low and high-density lipoprotein cholesterol (LDL, HDL), triglycerides were also assessed.
Results: The study included 886 patients with RA (mean age 65 years, 65% females, 95% Whites); 63% were RF/anti-CCP positive. While cumulative ESR was not associated with development of dementia (HR 1.03, 95% CI 0.97-1.09) in the total sample, it was significantly associated with increased risk of dementia among smokers (interaction p=0.03; Figure). Adjusting for CVD, the interaction effect persisted but was no longer statistically significant. In patients with seropositive RA, cumulative ESR and ever smoking interacted to increase the risk of dementia (p=0.04). There was a statistically significant interaction between the highest ESR in the first year of RA and baseline LDL (p=0.02), wherein high LDL was associated with increased risk of dementia among patients with normal ESR but with decreased risk of dementia among those with high ESR. No such interactions were found for other lipid measures.
Conclusion: Cumulative inflammation interacts with smoking, resulting in increased risk of dementia. Similarly, there is an interaction between highest ESR and LDL on the risk of dementia. Lipids may have paradoxical association with risk of dementia in RA with potential implications for dementia risk estimation in patients with elevated ESR. Our findings highlight the important role of modifiable risk factors and systemic inflammation in the pathogenesis of dementia in patients with RA.
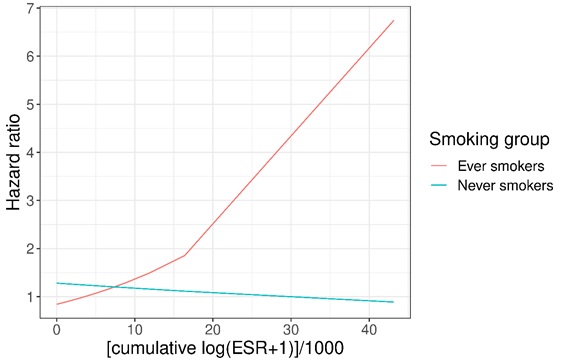 Figure: Interaction of cumulative ESR and smoking
Figure: Interaction of cumulative ESR and smokingDisclosures: C. Kodishala, None; S. Duong, None; C. Hulshizer, None; R. Lennon, None; R. Javed, None; M. Vassilaki, F. Hoffmann-La Roche, Biogen, F. Hoffmann-La Roche, Avobis Bio, LLC., Amgen, Abbott Laboratories, Johnson and Johnson, Medtronic, AbbVie; M. Mielke, LabCorp, Biogen; J. Davis, Pfizer; C. Crowson, None; E. Myasoedova, None.

