Back
Poster Session C
Imaging
Session: (1228–1266) Imaging of Rheumatic Diseases Poster
1247: Lung Ultrasound in Patients with Connective Tissue Disease-associated Interstitial Lung Disease; Utility of Single Evaluation in Clinical Practice
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SW
Shinji Watanabe, MD
Nippon Medical School
Tokyo, Japan
Abstract Poster Presenter(s)
Shinji Watanabe1, Keina Yomono2, Mikito Suzuki2, Nobuhito Sasaki2, Takahisa Gono2 and Masataka Kuwana2, 1Nippon Medical School Graduate School of Medicine, Bunkyo-ku, Tokyo, Japan, 2Nippon Medical School Graduate School of Medicine, Tokyo, Japan
Background/Purpose: Utility of lung ultrasound (LUS) in evaluation of interstitial lung disease (ILD) has recently attracted attention because of handiness and low invasiveness. The majority of previous reports dealt with systemic sclerosis (SSc)-associated ILD, while it remains unclear how to apply LUS to clinical practice of connective tissue disease (CTD)-associated ILD (CTD-ILD). Using a prospective registry of LUS, we examined i) whether LUS can be a substitute for a prognostic indicator (ILD extent) obtained by high-resolution CT (HRCT) and ii) whether LUS has additional benefits to information obtained from HRCT.
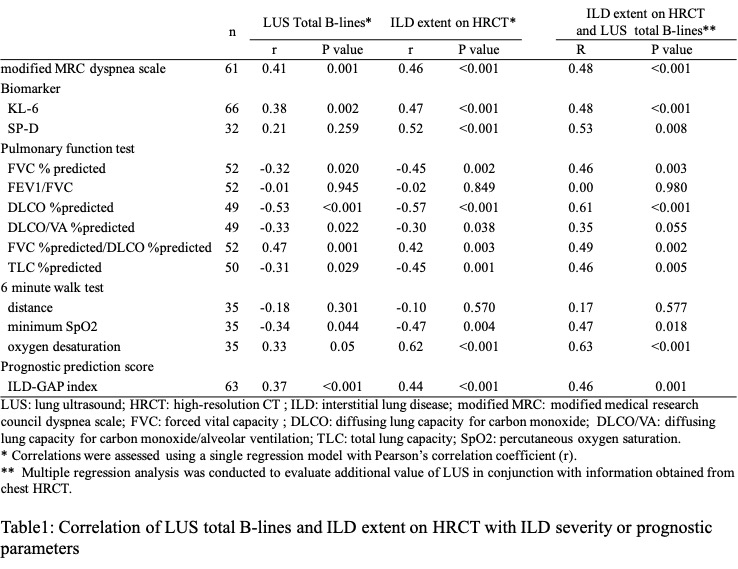
Methods: Patients with CTD-ILD who underwent HRCT and LUS simultaneously were selected from a single-center prospective registry of LUS, based on satisfaction of at least one of classification criteria for idiopathic inflammatory myopathy (IIM), anti-synthetase antibody syndrome (ASS), SSc, rheumatoid arthritis (RA), or mixed connective tissue disease (MCTD); and ILD confirmed by HRCT. Total B-lines were assessed using a 4-8 MHz microconvex transducer at 14 scanning sites. ILD extent on HRCT was semi-quantitatively assessed using an average of five sections according to Goh et al. We used modified MRC dyspnea scale, serum KL-6 and SP-D, forced vital capacity (FVC), diffusing lung capacity for carbon monoxide (DLCO), HRCT pattern, 6-minute walk test (6MWT) parameters, and GAP index as severity or prognostic parameters. Correlations were assessed using a single regression model with Pearson's correlation coefficient (r). Multiple regression analysis was conducted to evaluate additional value of LUS in conjunction with information obtained from chest HRCT.
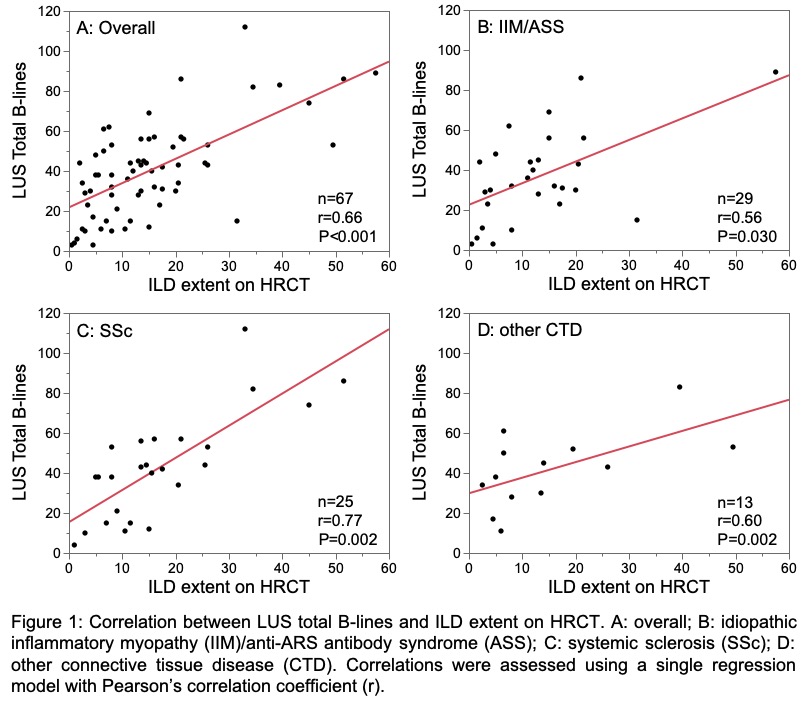
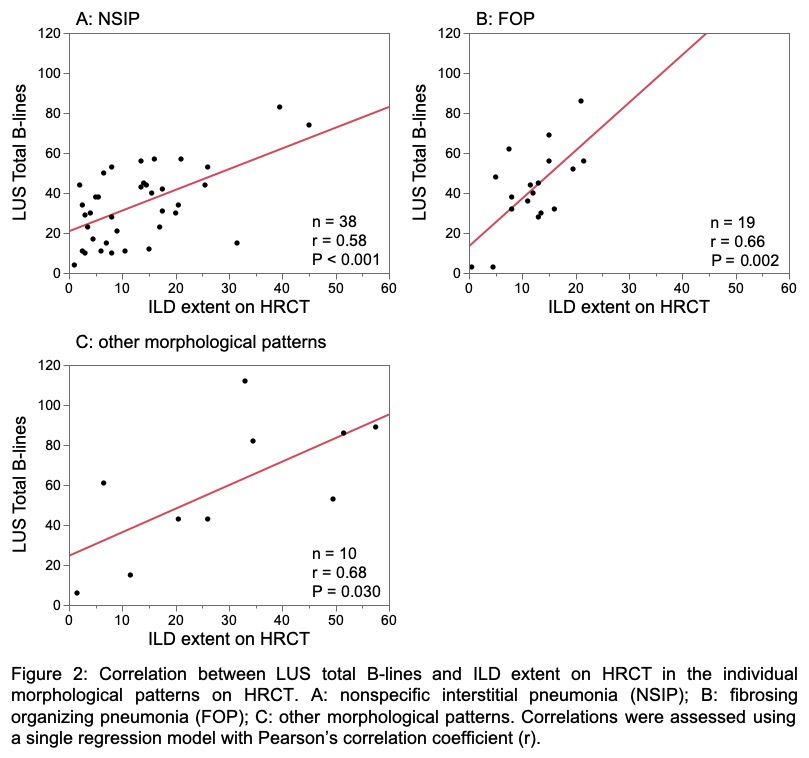
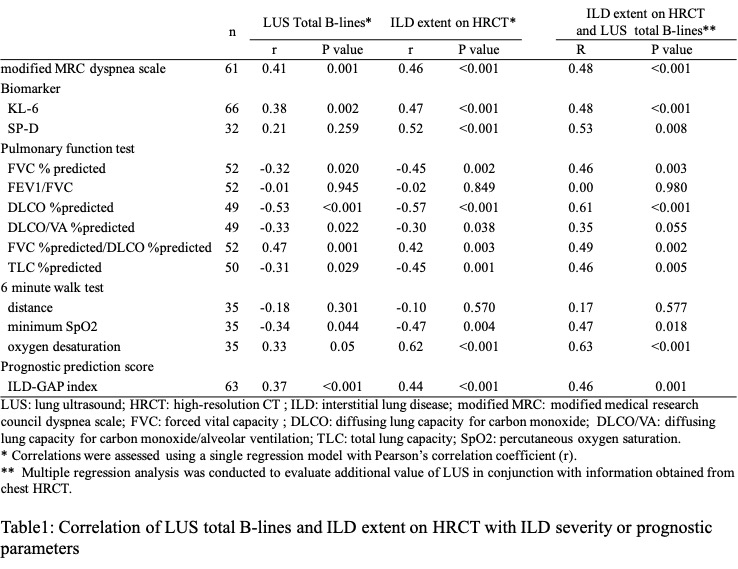
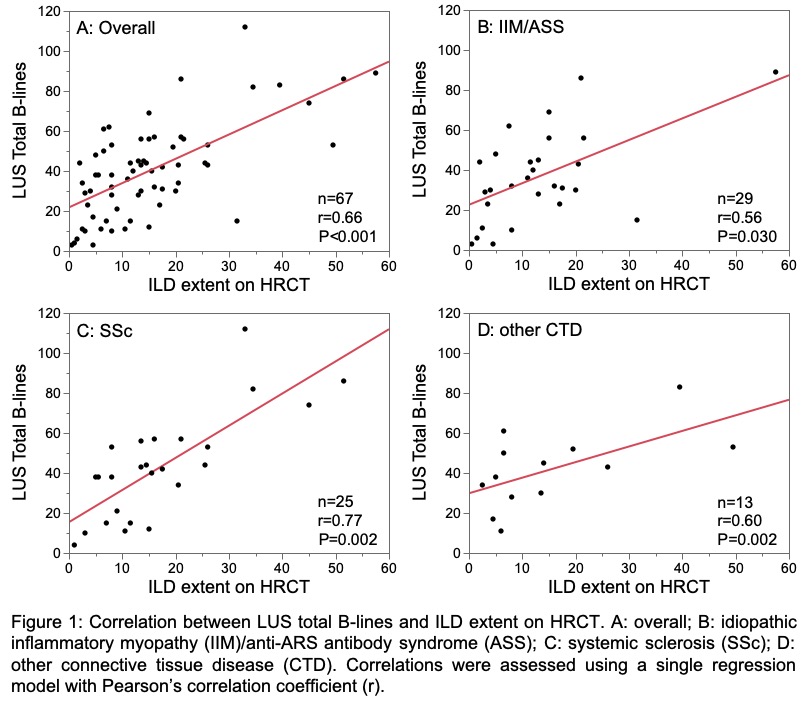
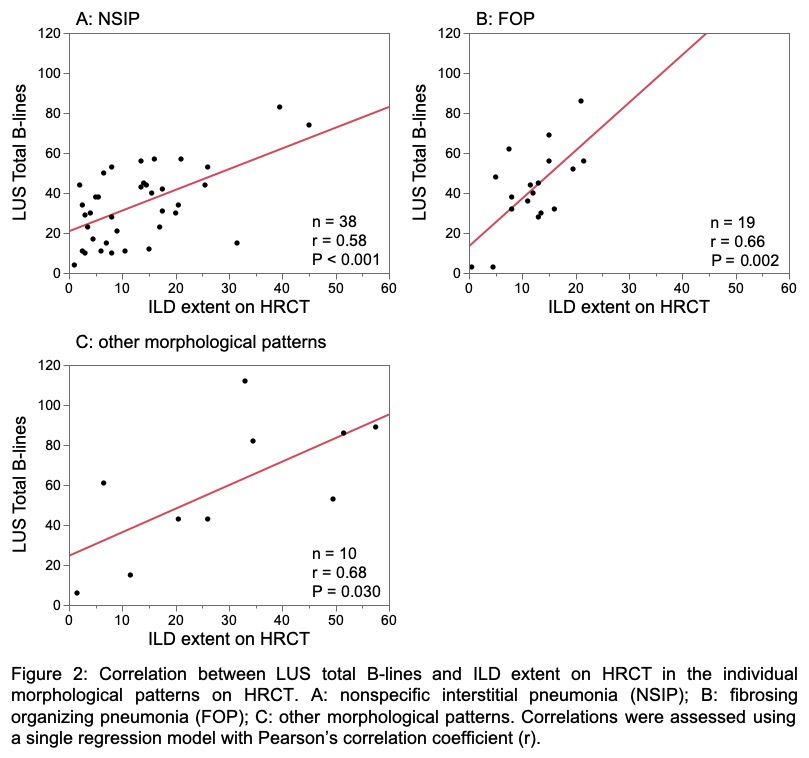
Results: This study enrolled 67 patients, including 29 with IIM/ASS, 25 with SSc, 10 with RA, and 3 with MCTD. LUS total B-lines and ILD extent on HRCT were correlated with each other (r = 0.66, P < 0.001). When the correlations between these indices were examined in individual CTDs, SSc showed better correlation, compared with IIM/ASS (Figure 1), while there was no difference in the correlations among patients with different HRCT morphologic patterns (Figure 2). LUS total B-lines and ILD extent on HRCT correlated individually with modified MRC dyspnea scale, serum KL-6, FVC, DLCO, minimum SpO2 during 6MWT and GAP index, although the correlation coefficient tended to be better for HRCT (Table 1). Multiple regression analysis revealed that there was no improvement of the correlations of ILD extent on HRCT with severity/prognostic markers by incorporating LUS total B-lines as covariates.
Conclusion: LUS total B-lines were generally correlated with the ILD extent on HRCT in patients with CTD-ILD, especially in those with SSc-ILD. LUS total B-lines were correlated with many ILD severity/prognostic parameters, but we failed to demonstrate no additive role of LUS on top of HRCT at least in a single evaluation.
Disclosures: S. Watanabe, None; K. Yomono, None; M. Suzuki, None; N. Sasaki, None; T. Gono, Astellas, Asahi Kasei, Boehringer Ingelheim, Bristol Myers Squibb, Chugai, Daiichi Sankyo, Eli Lilly, Janssen, Mitsubishi Tanabe, Ono Pharmacetuicals; M. Kuwana, Boehringer-Ingelheim, Ono pharmaceuticals, Mochida, AbbVie/Abbott, Astellas, Janssen, Bayer, Corbus, Horizon.
Background/Purpose: Utility of lung ultrasound (LUS) in evaluation of interstitial lung disease (ILD) has recently attracted attention because of handiness and low invasiveness. The majority of previous reports dealt with systemic sclerosis (SSc)-associated ILD, while it remains unclear how to apply LUS to clinical practice of connective tissue disease (CTD)-associated ILD (CTD-ILD). Using a prospective registry of LUS, we examined i) whether LUS can be a substitute for a prognostic indicator (ILD extent) obtained by high-resolution CT (HRCT) and ii) whether LUS has additional benefits to information obtained from HRCT.
Methods: Patients with CTD-ILD who underwent HRCT and LUS simultaneously were selected from a single-center prospective registry of LUS, based on satisfaction of at least one of classification criteria for idiopathic inflammatory myopathy (IIM), anti-synthetase antibody syndrome (ASS), SSc, rheumatoid arthritis (RA), or mixed connective tissue disease (MCTD); and ILD confirmed by HRCT. Total B-lines were assessed using a 4-8 MHz microconvex transducer at 14 scanning sites. ILD extent on HRCT was semi-quantitatively assessed using an average of five sections according to Goh et al. We used modified MRC dyspnea scale, serum KL-6 and SP-D, forced vital capacity (FVC), diffusing lung capacity for carbon monoxide (DLCO), HRCT pattern, 6-minute walk test (6MWT) parameters, and GAP index as severity or prognostic parameters. Correlations were assessed using a single regression model with Pearson's correlation coefficient (r). Multiple regression analysis was conducted to evaluate additional value of LUS in conjunction with information obtained from chest HRCT.
Results: This study enrolled 67 patients, including 29 with IIM/ASS, 25 with SSc, 10 with RA, and 3 with MCTD. LUS total B-lines and ILD extent on HRCT were correlated with each other (r = 0.66, P < 0.001). When the correlations between these indices were examined in individual CTDs, SSc showed better correlation, compared with IIM/ASS (Figure 1), while there was no difference in the correlations among patients with different HRCT morphologic patterns (Figure 2). LUS total B-lines and ILD extent on HRCT correlated individually with modified MRC dyspnea scale, serum KL-6, FVC, DLCO, minimum SpO2 during 6MWT and GAP index, although the correlation coefficient tended to be better for HRCT (Table 1). Multiple regression analysis revealed that there was no improvement of the correlations of ILD extent on HRCT with severity/prognostic markers by incorporating LUS total B-lines as covariates.
Conclusion: LUS total B-lines were generally correlated with the ILD extent on HRCT in patients with CTD-ILD, especially in those with SSc-ILD. LUS total B-lines were correlated with many ILD severity/prognostic parameters, but we failed to demonstrate no additive role of LUS on top of HRCT at least in a single evaluation.
Disclosures: S. Watanabe, None; K. Yomono, None; M. Suzuki, None; N. Sasaki, None; T. Gono, Astellas, Asahi Kasei, Boehringer Ingelheim, Bristol Myers Squibb, Chugai, Daiichi Sankyo, Eli Lilly, Janssen, Mitsubishi Tanabe, Ono Pharmacetuicals; M. Kuwana, Boehringer-Ingelheim, Ono pharmaceuticals, Mochida, AbbVie/Abbott, Astellas, Janssen, Bayer, Corbus, Horizon.

