Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1186–1214) Epidemiology and Public Health Poster II
1190: Multimorbidity in Systemic Sclerosis: Burden and Trends in Prevalence from an Incident Population-based Cohort (1980-2018)
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time

Ashima Makol, MD
Mayo Clinic, Rochester, MN
Rochester, MN, United States
Abstract Poster Presenter(s)
Ashima Makol1, Sara Achenbach1, Alicia Hinze2, Tina Gunderson3 and Cynthia Crowson4, 1Mayo Clinic, Rochester, MN, Rochester, MN, 2Mayo Clinic - Rochester, MN, Rochester, MN, 3Mayo Clinic, Rochester, MN, 4Mayo Clinic, Eyota, MN
Background/Purpose: To estimate the prevalence and trends of multimorbidity (MM; the presence of ≥2 morbidities) in a population-based cohort of patients with Systemic sclerosis (SSc) compared to age-and sex-matched non-SSc comparators.
Methods: A population-based cohort of incident SSc patients in a geographically well-defined area from Jan 1, 1980 to Dec 31, 2018 was identified and compared to a 2:1 cohort of age- and sex-matched non-SSc subjects from the same population. Patients who died or emigrated from the area prior to 1987 were excluded. Patients were followed until death, migration from the geographic area or Dec 31, 2021. Data on 21 morbidities identified by the US Department of Health and Human Services (DHHS) and 13 morbidities included in the Charlson Comorbidity Index (CCI) was retrieved. Cumulative incidence of MM (MM2+) or substantial MM (MM5+; ≥ 5 morbidities) adjusting for the competing risk of death was estimated. Cox models adjusted for age, sex, index year and morbidity count at index date were used to compare cases and comparators. Patients with 2 or 5 morbidities before index date, respectively, were excluded from these analyses.
Results: Between 1980-2018, 85 patients with SSc and 170 age- and sex-matched non SSc comparators (mean age 55.4 y, 91% female, 90% white/non-Hispanic) were identified. Mean length of follow-up was 12.4 y (SD 9.8) for SSc & 15.5 y (SD 9.8) for comparators. At incidence/index date, a significantly higher prevalence of COPD (14% vs 4%, p=0.004), arthritis (33% vs 22%, p=0.054), peripheral vascular disease (40% vs 2%, p< 0.001) and liver disease (5% vs 1%, p=0.04) were noted in patients with SSc. At incidence/index date, while the prevalence of DHHS MM2+ was similar between the 2 groups (44% in SSc vs 41% in comparators, p=0.65), CCI MM2+ was significantly higher among patients with SSc vs comparators (19% vs 7%, p =0.005). The cumulative incidence of DHHS MM2+ during follow-up was similar between SSc and comparators, but the development of DHHS MM5+ was significantly higher among patients with SSc vs. comparators (hazard ratio [HR] 1.58; 95% confidence interval [CI] 1.09-2.31). Concordantly, the cumulative incidence of DHHS MM5+ was higher in SSc patients vs comparators at 10 (44% vs 32%), 15 (52% vs 45%) and 20 (64% vs 58%) years of follow up (Figure). The development of CCI-MM2+ (HR 4.56; 95%CI 3.00-6.93) was significantly higher among SSc patients but CCI-MM5+ did not reach statistical significance after adjustment for morbidity count at index (HR 1.65; 95%CI 0.80-3.43).
Conclusion: To our knowledge, this is the first study to examine multimorbidity in SSc. In this population-based cohort, patients with SSc had a significantly higher burden of multimorbidity at diagnosis, and a much higher risk of developing substantial multimorbidity at follow up than age- and sex-matched individuals without SSc.
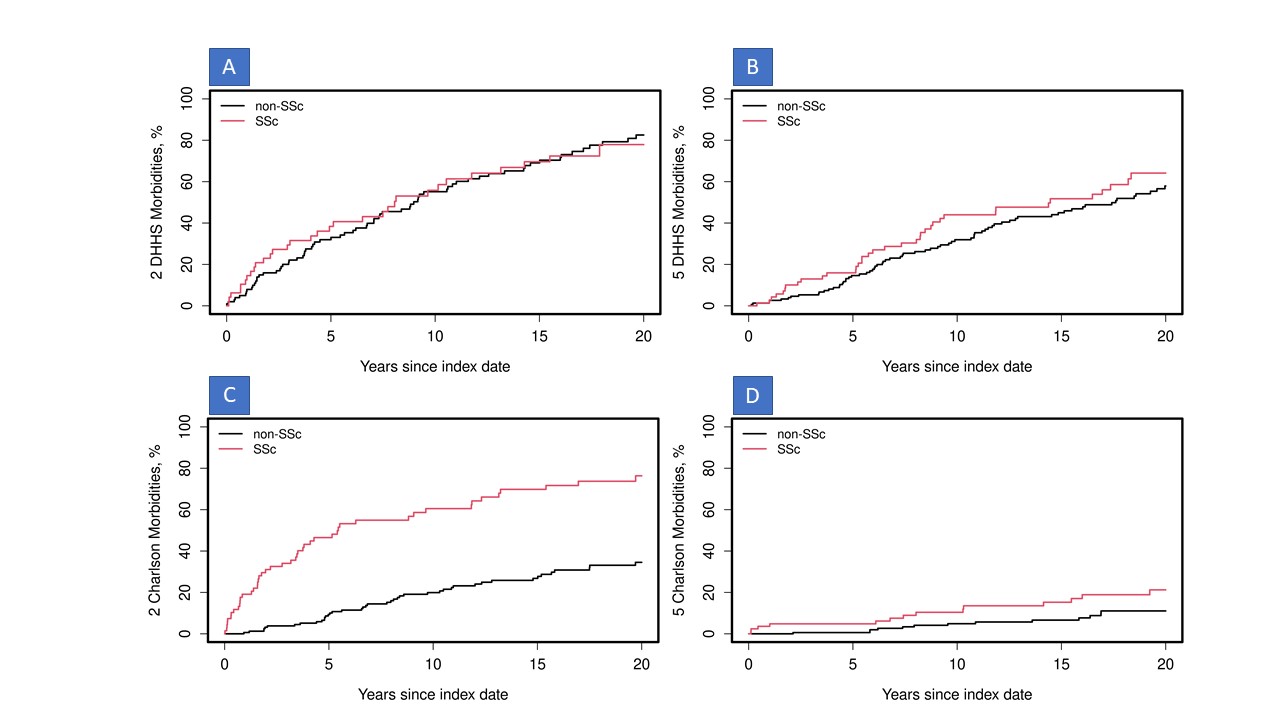 Figure. A and B. Cumulative incidence for time to DHHS-MM2+ and DHHS-MM5+ morbidity events adjusted for the competing risk of death. C and D. Cumulative incidence for time to CCI-MM2+ and CCI-MM5+ events adjusted for the competing risk of death. Patients with 2 and 5 events before index date were excluded, respectively. Abbreviations: DHHS- Department of Health and Human Services; MM- Multimorbidity; CCI-Charlson comorbidity index; SSc-Systemic sclerosis
Figure. A and B. Cumulative incidence for time to DHHS-MM2+ and DHHS-MM5+ morbidity events adjusted for the competing risk of death. C and D. Cumulative incidence for time to CCI-MM2+ and CCI-MM5+ events adjusted for the competing risk of death. Patients with 2 and 5 events before index date were excluded, respectively. Abbreviations: DHHS- Department of Health and Human Services; MM- Multimorbidity; CCI-Charlson comorbidity index; SSc-Systemic sclerosis
Disclosures: A. Makol, Boehringer-Ingelheim; S. Achenbach, None; A. Hinze, None; T. Gunderson, None; C. Crowson, None.
Background/Purpose: To estimate the prevalence and trends of multimorbidity (MM; the presence of ≥2 morbidities) in a population-based cohort of patients with Systemic sclerosis (SSc) compared to age-and sex-matched non-SSc comparators.
Methods: A population-based cohort of incident SSc patients in a geographically well-defined area from Jan 1, 1980 to Dec 31, 2018 was identified and compared to a 2:1 cohort of age- and sex-matched non-SSc subjects from the same population. Patients who died or emigrated from the area prior to 1987 were excluded. Patients were followed until death, migration from the geographic area or Dec 31, 2021. Data on 21 morbidities identified by the US Department of Health and Human Services (DHHS) and 13 morbidities included in the Charlson Comorbidity Index (CCI) was retrieved. Cumulative incidence of MM (MM2+) or substantial MM (MM5+; ≥ 5 morbidities) adjusting for the competing risk of death was estimated. Cox models adjusted for age, sex, index year and morbidity count at index date were used to compare cases and comparators. Patients with 2 or 5 morbidities before index date, respectively, were excluded from these analyses.
Results: Between 1980-2018, 85 patients with SSc and 170 age- and sex-matched non SSc comparators (mean age 55.4 y, 91% female, 90% white/non-Hispanic) were identified. Mean length of follow-up was 12.4 y (SD 9.8) for SSc & 15.5 y (SD 9.8) for comparators. At incidence/index date, a significantly higher prevalence of COPD (14% vs 4%, p=0.004), arthritis (33% vs 22%, p=0.054), peripheral vascular disease (40% vs 2%, p< 0.001) and liver disease (5% vs 1%, p=0.04) were noted in patients with SSc. At incidence/index date, while the prevalence of DHHS MM2+ was similar between the 2 groups (44% in SSc vs 41% in comparators, p=0.65), CCI MM2+ was significantly higher among patients with SSc vs comparators (19% vs 7%, p =0.005). The cumulative incidence of DHHS MM2+ during follow-up was similar between SSc and comparators, but the development of DHHS MM5+ was significantly higher among patients with SSc vs. comparators (hazard ratio [HR] 1.58; 95% confidence interval [CI] 1.09-2.31). Concordantly, the cumulative incidence of DHHS MM5+ was higher in SSc patients vs comparators at 10 (44% vs 32%), 15 (52% vs 45%) and 20 (64% vs 58%) years of follow up (Figure). The development of CCI-MM2+ (HR 4.56; 95%CI 3.00-6.93) was significantly higher among SSc patients but CCI-MM5+ did not reach statistical significance after adjustment for morbidity count at index (HR 1.65; 95%CI 0.80-3.43).
Conclusion: To our knowledge, this is the first study to examine multimorbidity in SSc. In this population-based cohort, patients with SSc had a significantly higher burden of multimorbidity at diagnosis, and a much higher risk of developing substantial multimorbidity at follow up than age- and sex-matched individuals without SSc.
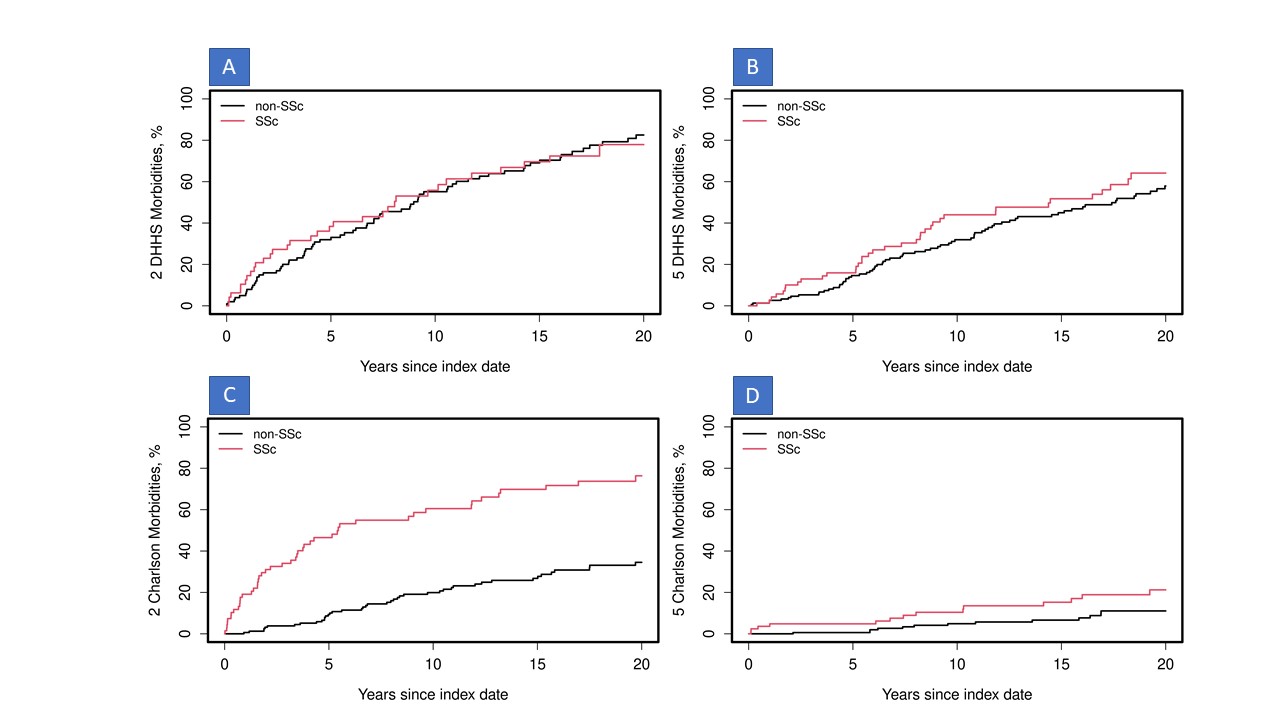 Figure. A and B. Cumulative incidence for time to DHHS-MM2+ and DHHS-MM5+ morbidity events adjusted for the competing risk of death. C and D. Cumulative incidence for time to CCI-MM2+ and CCI-MM5+ events adjusted for the competing risk of death. Patients with 2 and 5 events before index date were excluded, respectively. Abbreviations: DHHS- Department of Health and Human Services; MM- Multimorbidity; CCI-Charlson comorbidity index; SSc-Systemic sclerosis
Figure. A and B. Cumulative incidence for time to DHHS-MM2+ and DHHS-MM5+ morbidity events adjusted for the competing risk of death. C and D. Cumulative incidence for time to CCI-MM2+ and CCI-MM5+ events adjusted for the competing risk of death. Patients with 2 and 5 events before index date were excluded, respectively. Abbreviations: DHHS- Department of Health and Human Services; MM- Multimorbidity; CCI-Charlson comorbidity index; SSc-Systemic sclerosisDisclosures: A. Makol, Boehringer-Ingelheim; S. Achenbach, None; A. Hinze, None; T. Gunderson, None; C. Crowson, None.

