Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1332–1359) Patient Outcomes, Preferences, and Attitudes Poster II
1340: Nutrition-Related Behaviors and Beliefs - A Survey of Rheumatic Disease Patients
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- SL
Sandy Lee, DO
University of Southern California
Walnut, CA, United States
Abstract Poster Presenter(s)
Sandy Lee1, Leanna Wise2 and Stavros Savvas3, 1University of Southern California, Walnut, CA, 2LAC+USC/Keck Medicine of USC, Pasadena, CA, 3Keck Medicine of USC, Glendale, CA
Background/Purpose: Diet and nutrition have long been of interest to both patients and providers in the treatment of chronic disease. The literature is relatively sparse regarding the role of nutrition in rheumatic disease patients. We surveyed the predominantly Hispanic patients with rheumatic disease at a Los Angeles County safety-net hospital in California to understand their behaviors and beliefs regarding nutrition and rheumatic diseases, as well as to gauge their receptivity towards potential dietary interventions.
Methods: We created a 28-question anonymous survey on a variety of nutrition-related topics. It includes whether patients have tried dietary changes for their rheumatic disease, whether they noted certain foods to affect their disease activity, and barriers and receptivity to dietary interventions. After extensive pilot testing, the survey was distributed, in either English or Spanish, in paper format to patients before their rheumatology appointments.
Results: A total of 117 surveys were collected from April 18, 2022 to May 31, 2022. Participants (Table 1) were predominantly female (86.1%) and Hispanic (85.2%) with a preferred language of Spanish (69.6%). The most frequent diagnoses reported were rheumatoid arthritis (60.7%), systemic lupus erythematosus (28.6%), and fibromyalgia (8.9%). Over a third (38.3%) of patients felt their disease was affected by what they ate. We evaluated participants' opinions of common food categories that may improve or aggravate disease (Figure 1). Participants noted fruits, vegetables, and white meat (chicken and fish) to improve disease, whereas red meat (pork and beef), desserts, and "fast food" were frequently noted to worsen disease. We also gauged participants' willingness to change dietary patterns if there was a possibility of disease amelioration. The overwhelming majority of participants stated they would be willing to amend their diet if it would lead to improvement in their rheumatic disease (Table 2).
Conclusion: Based on our data, a significant proportion of our primarily Hispanic patient population has noted a correlation between dietary intake and rheumatic disease activity and has trialed some form of dietary intervention. There are clear trends in favor of certain food groups that improve disease activity (such as fruits, vegetables, white meats, beans, nuts, and spices), as well as food groups that seem to have a detrimental effect on disease activity. This "real life" data from our patient population is consistent with prior literature that suggest naturally occurring anti-inflammatory agents such as polyphenolic compounds and polyunsaturated fatty acids may modulate systemic inflammation.
Research in nutrition is still in its formative years, especially regarding systemic autoimmune diseases; however, that should not preclude the rheumatology community from exploring nutrition as a therapeutic intervention. Many patients are willing to explore dietary changes to treat their disease. This promising outlook paves the way for future dietary implementations for a Hispanic rheumatic disease population.
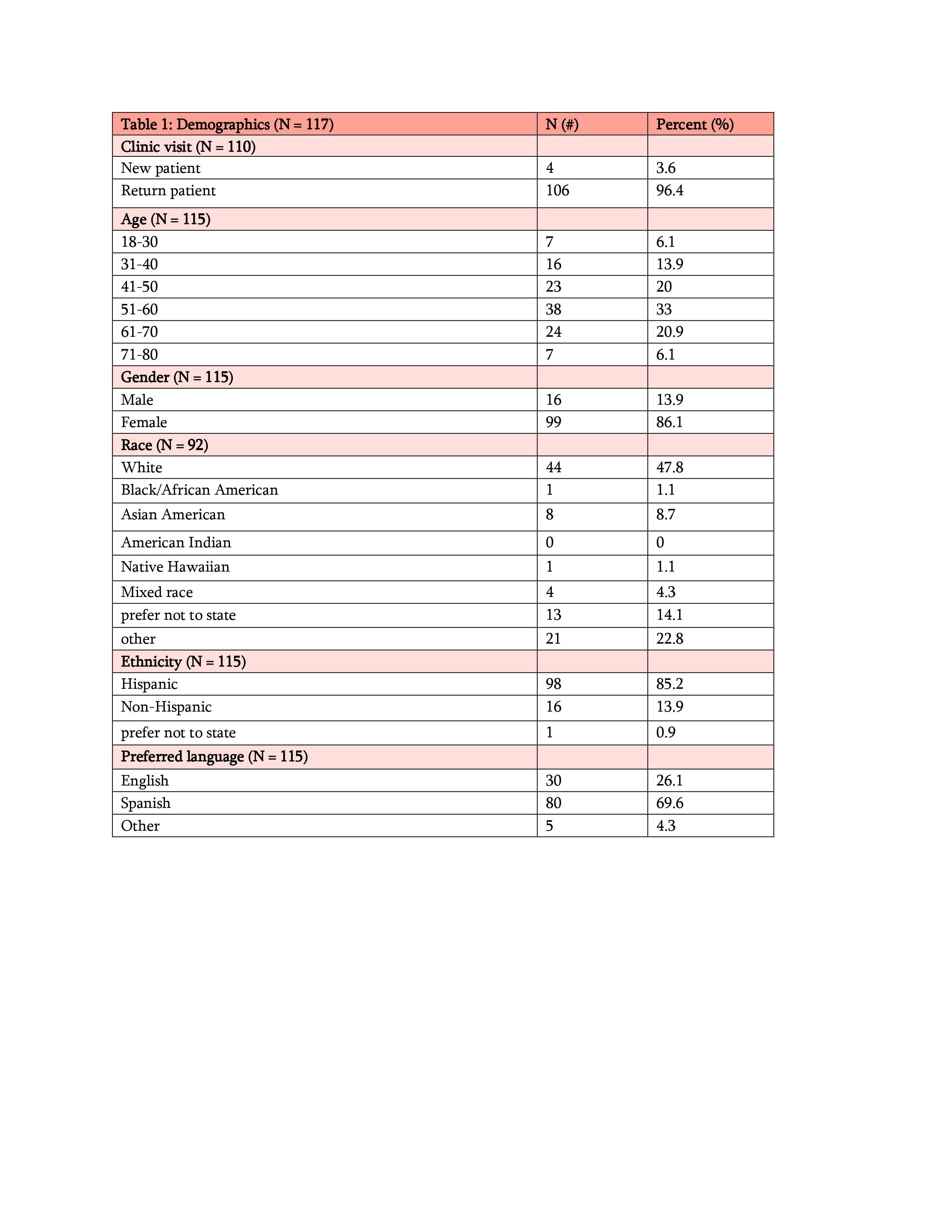
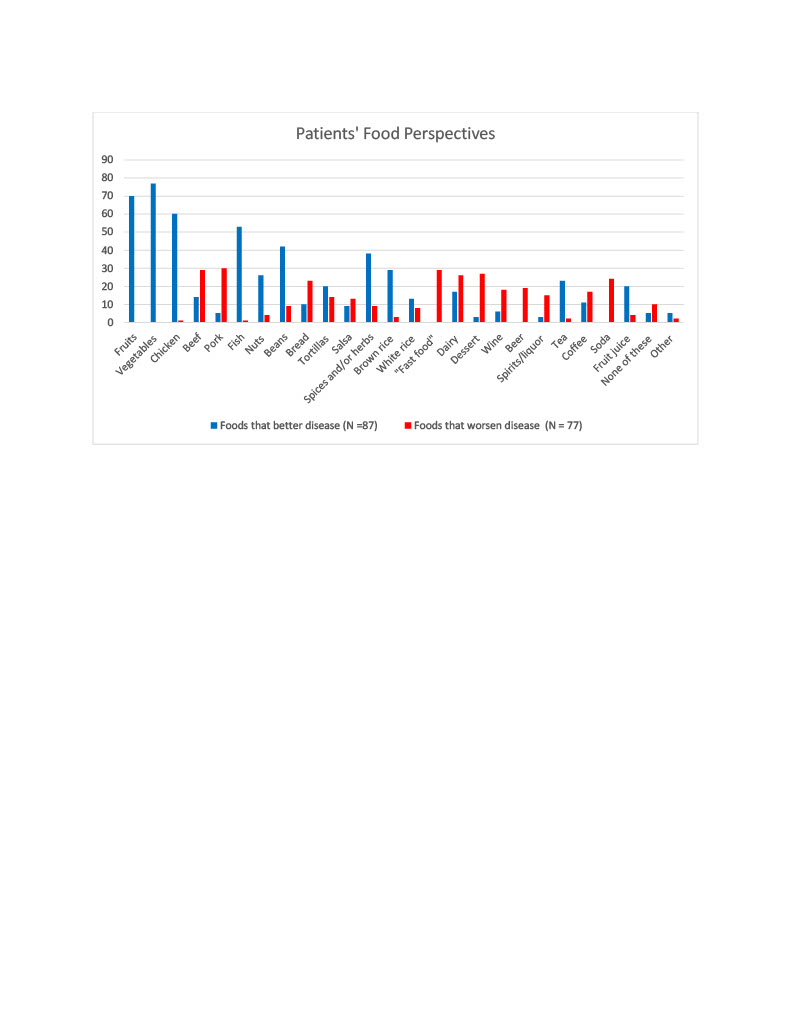 Figure 1: Patients’ perspectives on foods that better disease or worsen disease.
Figure 1: Patients’ perspectives on foods that better disease or worsen disease.
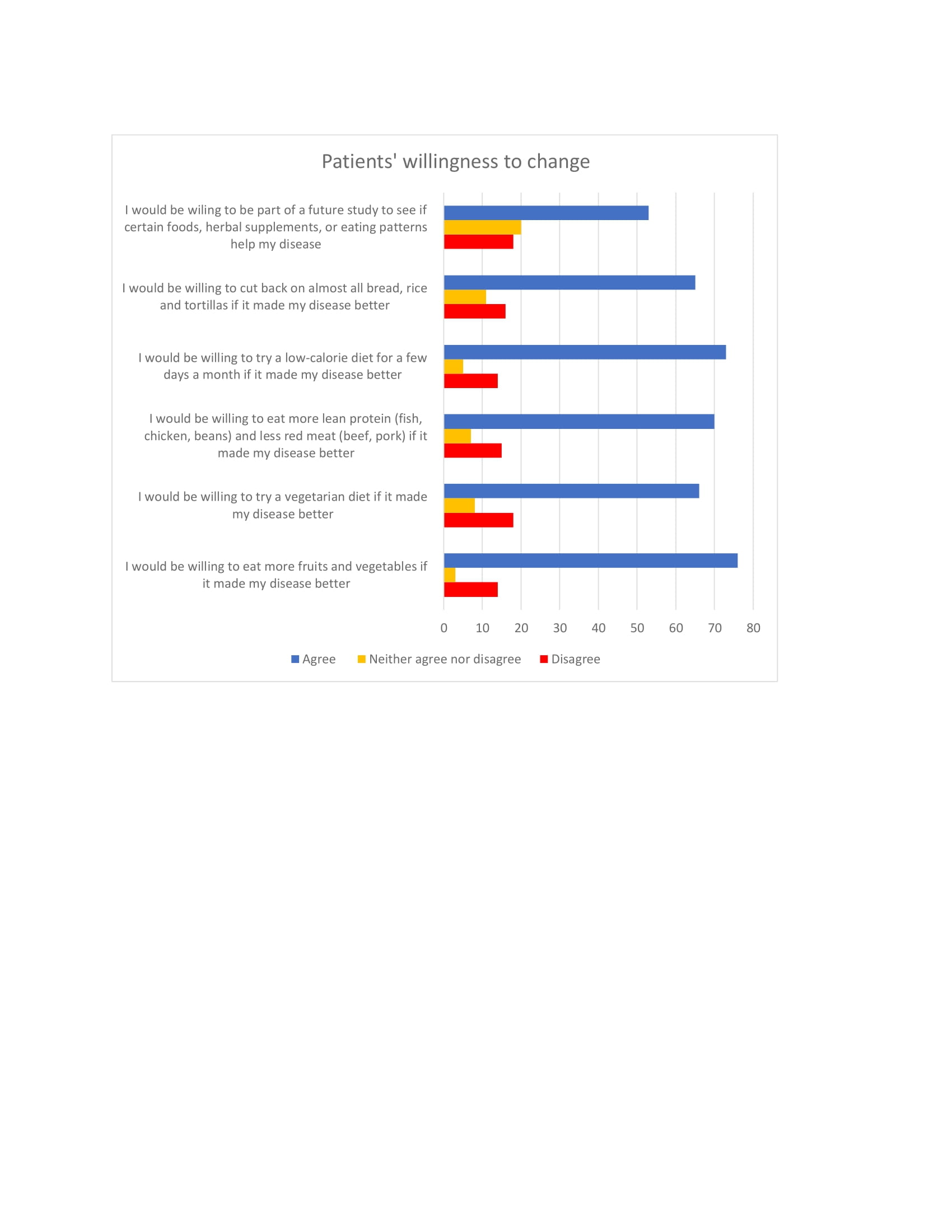 Figure 2: Patients’ willingness to change dietary habits to improve disease.
Figure 2: Patients’ willingness to change dietary habits to improve disease.
Disclosures: S. Lee, None; L. Wise, Aurinia Pharma; S. Savvas, None.
Background/Purpose: Diet and nutrition have long been of interest to both patients and providers in the treatment of chronic disease. The literature is relatively sparse regarding the role of nutrition in rheumatic disease patients. We surveyed the predominantly Hispanic patients with rheumatic disease at a Los Angeles County safety-net hospital in California to understand their behaviors and beliefs regarding nutrition and rheumatic diseases, as well as to gauge their receptivity towards potential dietary interventions.
Methods: We created a 28-question anonymous survey on a variety of nutrition-related topics. It includes whether patients have tried dietary changes for their rheumatic disease, whether they noted certain foods to affect their disease activity, and barriers and receptivity to dietary interventions. After extensive pilot testing, the survey was distributed, in either English or Spanish, in paper format to patients before their rheumatology appointments.
Results: A total of 117 surveys were collected from April 18, 2022 to May 31, 2022. Participants (Table 1) were predominantly female (86.1%) and Hispanic (85.2%) with a preferred language of Spanish (69.6%). The most frequent diagnoses reported were rheumatoid arthritis (60.7%), systemic lupus erythematosus (28.6%), and fibromyalgia (8.9%). Over a third (38.3%) of patients felt their disease was affected by what they ate. We evaluated participants' opinions of common food categories that may improve or aggravate disease (Figure 1). Participants noted fruits, vegetables, and white meat (chicken and fish) to improve disease, whereas red meat (pork and beef), desserts, and "fast food" were frequently noted to worsen disease. We also gauged participants' willingness to change dietary patterns if there was a possibility of disease amelioration. The overwhelming majority of participants stated they would be willing to amend their diet if it would lead to improvement in their rheumatic disease (Table 2).
Conclusion: Based on our data, a significant proportion of our primarily Hispanic patient population has noted a correlation between dietary intake and rheumatic disease activity and has trialed some form of dietary intervention. There are clear trends in favor of certain food groups that improve disease activity (such as fruits, vegetables, white meats, beans, nuts, and spices), as well as food groups that seem to have a detrimental effect on disease activity. This "real life" data from our patient population is consistent with prior literature that suggest naturally occurring anti-inflammatory agents such as polyphenolic compounds and polyunsaturated fatty acids may modulate systemic inflammation.
Research in nutrition is still in its formative years, especially regarding systemic autoimmune diseases; however, that should not preclude the rheumatology community from exploring nutrition as a therapeutic intervention. Many patients are willing to explore dietary changes to treat their disease. This promising outlook paves the way for future dietary implementations for a Hispanic rheumatic disease population.
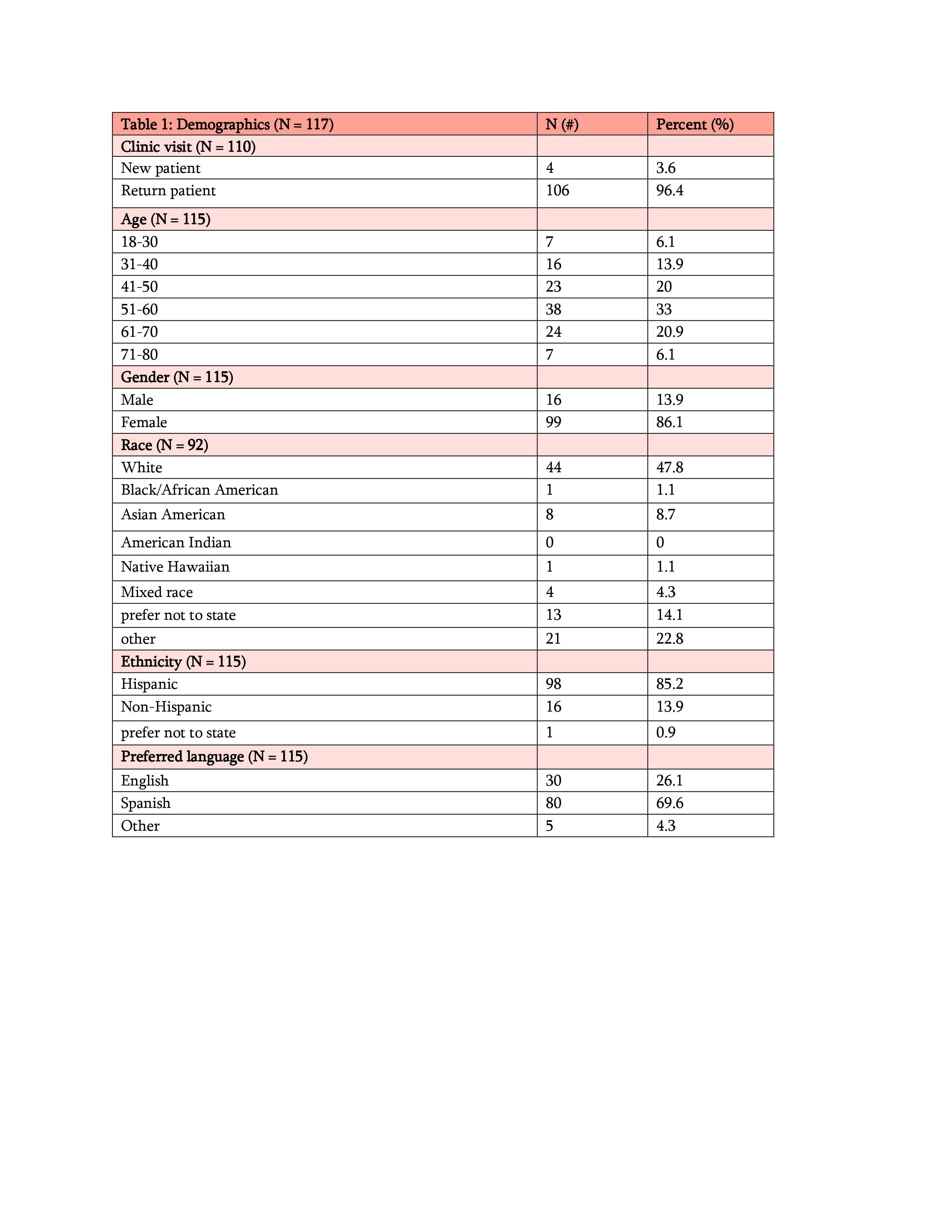
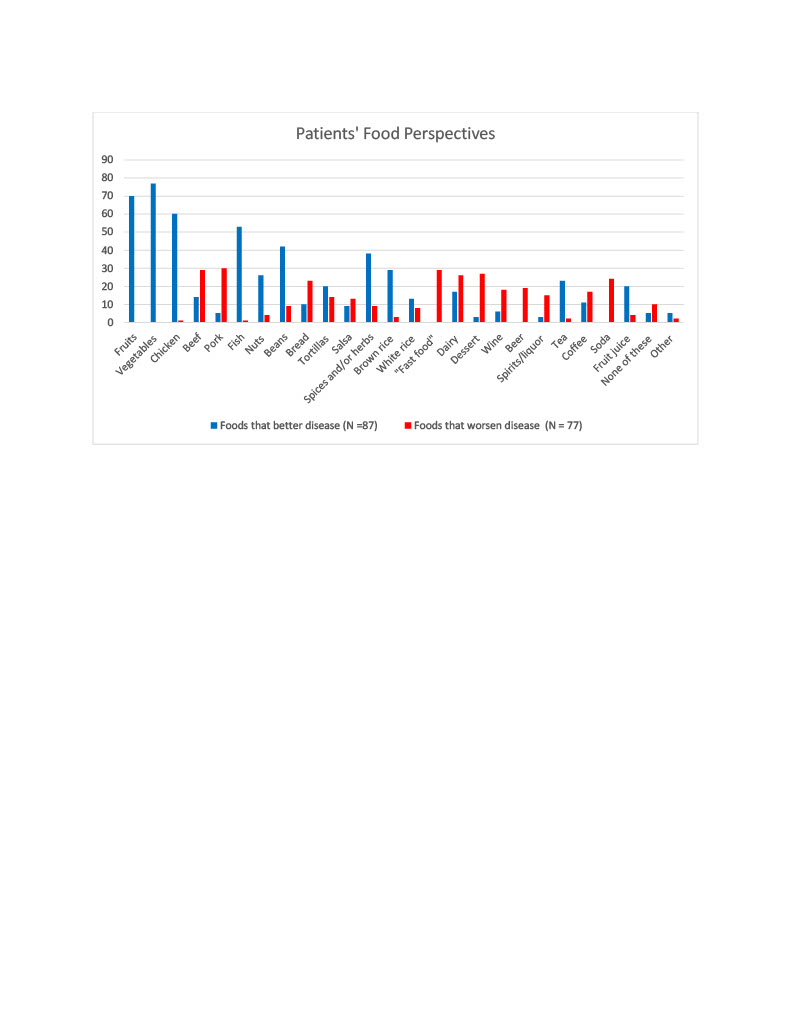 Figure 1: Patients’ perspectives on foods that better disease or worsen disease.
Figure 1: Patients’ perspectives on foods that better disease or worsen disease. 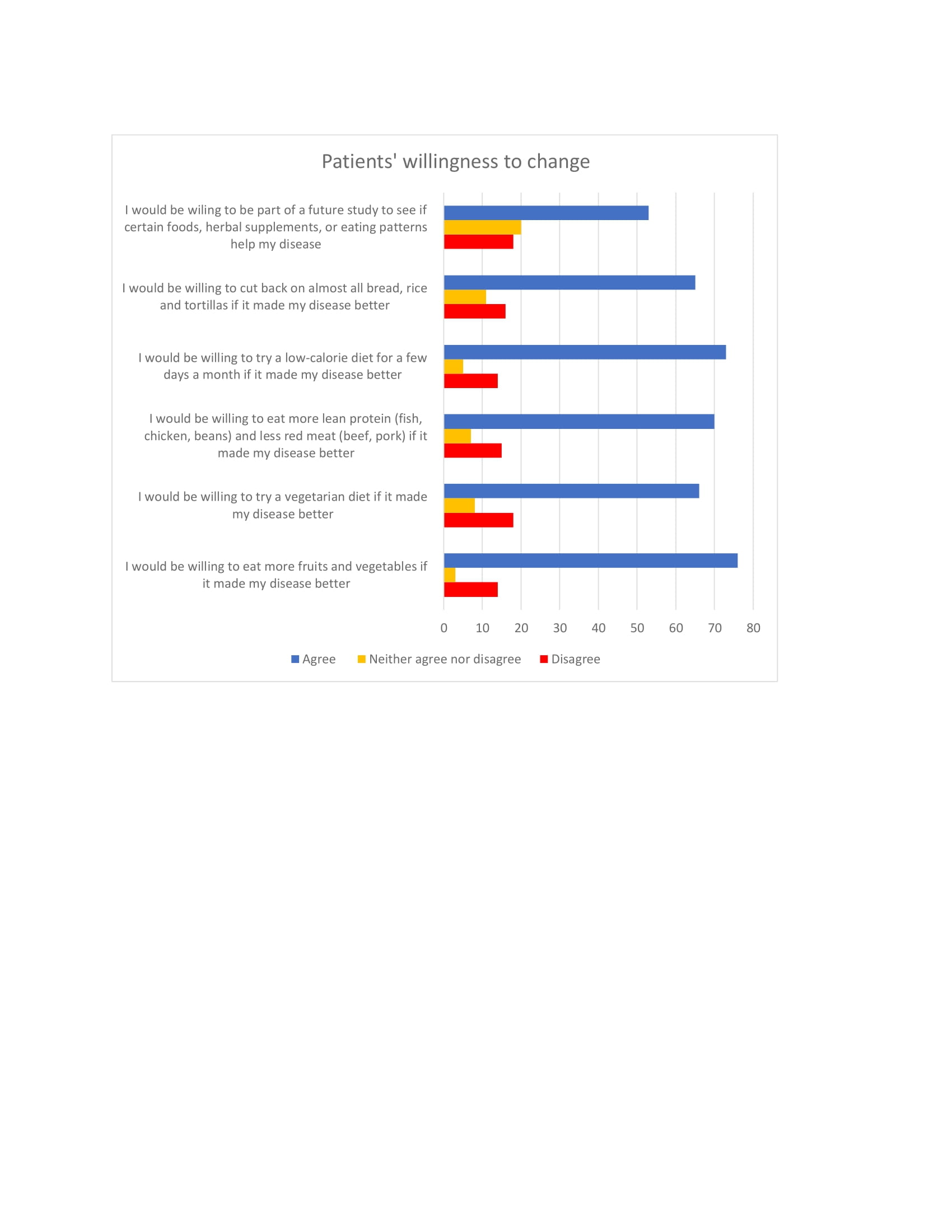 Figure 2: Patients’ willingness to change dietary habits to improve disease.
Figure 2: Patients’ willingness to change dietary habits to improve disease. Disclosures: S. Lee, None; L. Wise, Aurinia Pharma; S. Savvas, None.

