Back
Poster Session C
Systemic lupus erythematosus (SLE)
Session: (1440–1485) SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
1453: Prevalence and Associations of Myositis in an Indian Inception Cohort of Lupus
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- LR
Liza Rajasekhar, MD, MBBS
Nizam's Institute of Medical Sciences
Madhapur, Andhra Pradesh, India
Abstract Poster Presenter(s)
Liza Rajasekhar1, Vineetha Shobha2, Meenakshi Ponnana3, Chengappa Kavadichanda4, Ashish J Mathew5, Saumya Ranjan Tripathy6, Manish Rathi7, Parasar Ghosh8, Ranjan Gupta9, Avinash Jain10 and Amita Aggarwal11, 1Nizam's Institute of Medical Sciences, Madhapur, India, 2St. John’s Medical College Hospital, Bangalore, India, 3Nizam's Institute of Medical Sciences, Hyderabad, India, 4JIPMER, Pondicherry, Puducherry, India, 5Rigshospitalet, Copenhagen, Denmark, 6SCB medical college, Cuttack, India, 7PGIMER Chandigarh, Chandigarh, India, 8Govt of West Bengal, Kolkata, India, Kolkata, West Bengal, India, 9All India Institute of Medical Sciences, New Delhi, India, 10SMS Medical College, Lucknow, India, 11Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India
Background/Purpose: Muscle inflammation in systemic lupus erythematosus (SLE) usually presents as generalised myalgia in the presence of active disease elsewhere and responds well to treatment. There is paucity of data on myositis in lupus. We assessed the frequency and association of myositis in an inception cohort of SLE from India (INSPIRE).
Methods: The INSPIRE database includes patients satisfying the SLICC classification criteria for SLE with disease duration less than 3 years at 10 tertiary care hospitals across India. Myositis was defined by proximal muscle aching/weakness, associated with elevated CPK or LDH or AST or ALT. Other causes/drug induced myopathy or muscle enzyme elevation were excluded. Data on demographics, clinical, lab features, autoantibodies, and disease activity (SLEDAI, BILAG score), damage (SDI) and mortality were retrieved from the electronic database. SLE patients with myositis (cases) were compared with those not having myositis (controls). Difference in means between groups was done using student's t-test and difference in proportions using the chi-square test. Presence of infection, BILAG category A or B disease in any domain, myositis, gender were used as predictors of mortality using binomial logistic regression.
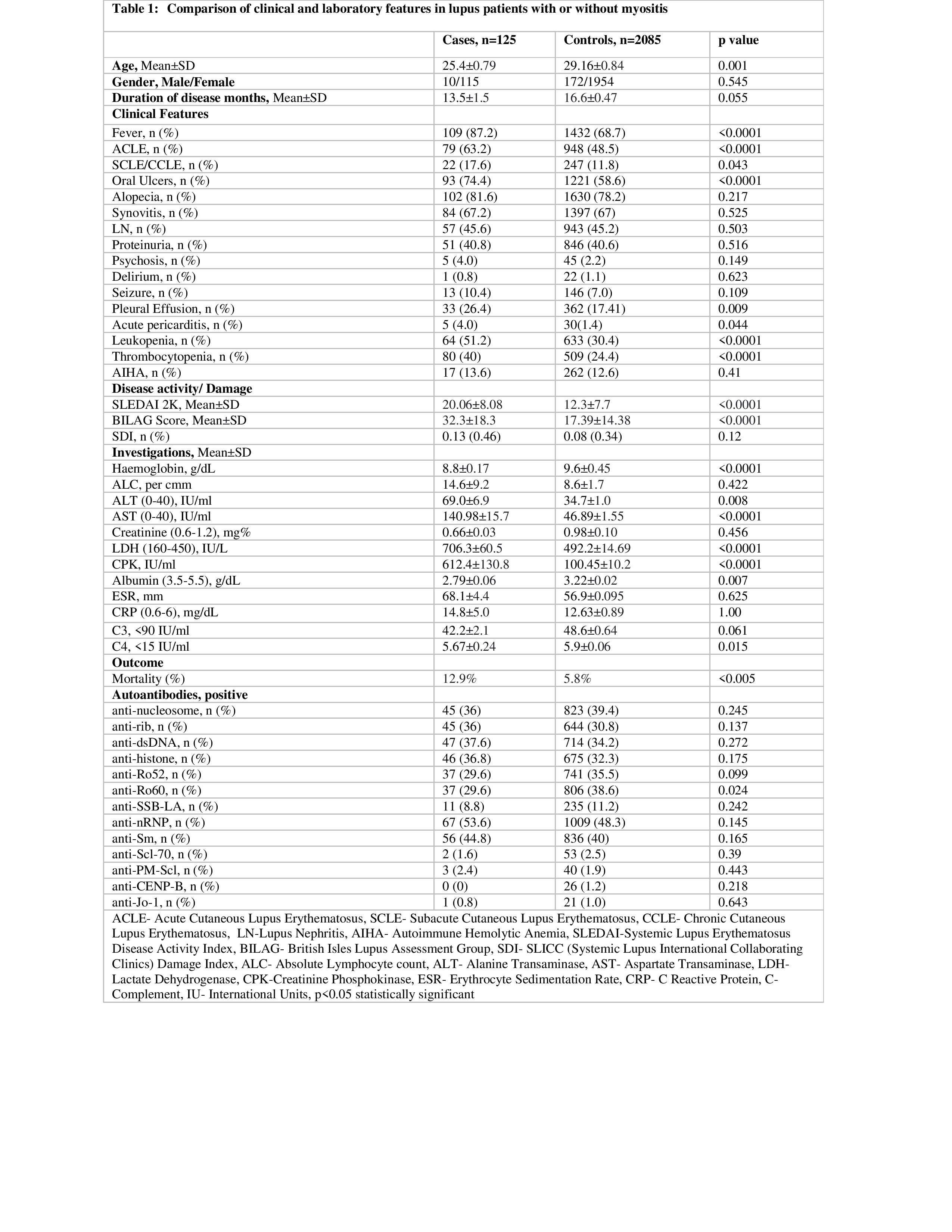
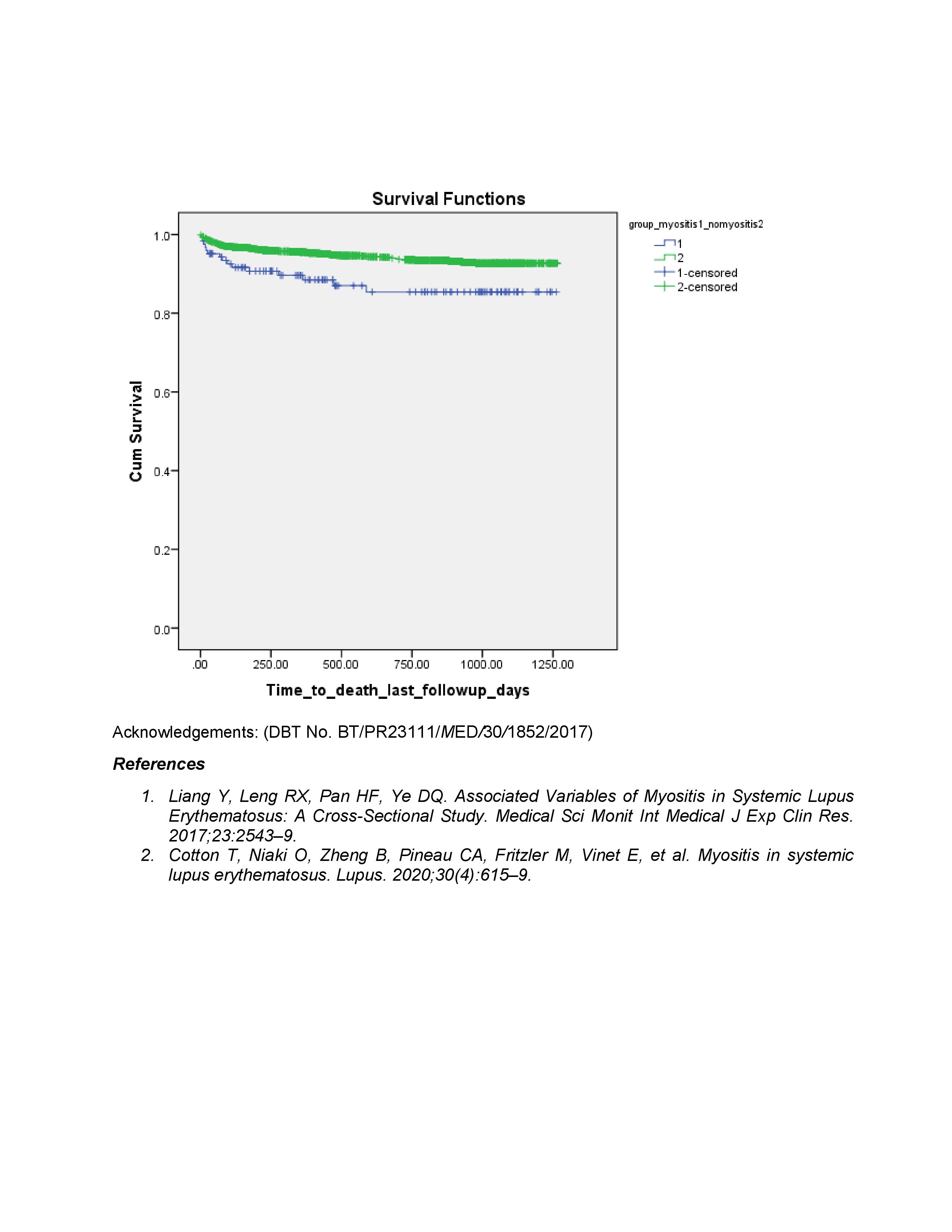
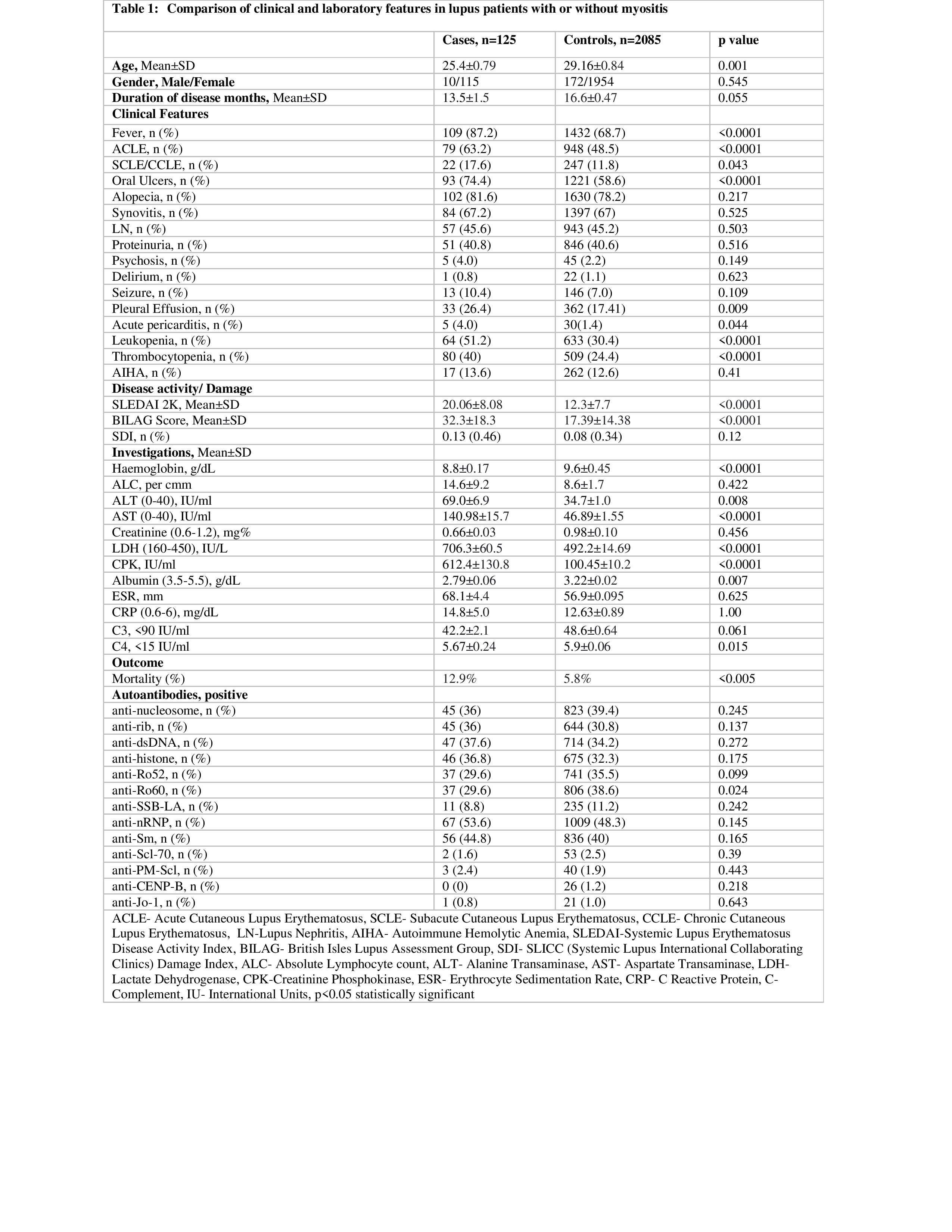
Results: A total of 2210 patients including 2029 (91.8%) females were enrolled in the study. Mean (SD) age at diagnosis was 28.9±0.79 years. Mean (SD) duration of disease was 16.4±0.45 months. Comorbidities included hypothyroidism (16.4%), hypertension in (8.8%), diabetes mellitus (1.6%). 133 patients died during mean follow-up of 22.4±12.5 months.125 (5.6%) patients had myositis, with myalgia present in 88%. On univariate analysis, cases were younger, with more frequent fever, acute cutaneous lupus, oral ulcers, pleural effusion, leukopenia, thrombocytopenia, lower haemoglobin, complements, and albumin and higher ALT, AST, LDH, CPK. SLEDAI and BILAG scores than controls (Table 1). Antibodies to Ro60 were more frequent in patients with myositis. Twelve cases had muscle damage as assessed by SDI. Patients with myositis had a significantly lower survival (87% vs 94%, p< 0.001, Figure 1). Univariate analysis identified fever, SLEDAI and CPK as the predictors of myositis at p< 0.05. Binomial logistic regression identified infection as a predictor of mortality at p< 0.03.
Conclusion: The prevalence of myositis in an Indian lupus cohort with early, very active disease was 5.6 %. Those with myositis had more active disease elsewhere, had similar damage but lower survival than those without. Myositis was not a predictor of mortality.
 Survival in patients with Myositis
Survival in patients with Myositis
Disclosures: L. Rajasekhar, None; V. Shobha, None; M. Ponnana, None; C. Kavadichanda, None; A. Mathew, None; S. Tripathy, None; M. Rathi, None; P. Ghosh, None; R. Gupta, None; A. Jain, None; A. Aggarwal, None.
Background/Purpose: Muscle inflammation in systemic lupus erythematosus (SLE) usually presents as generalised myalgia in the presence of active disease elsewhere and responds well to treatment. There is paucity of data on myositis in lupus. We assessed the frequency and association of myositis in an inception cohort of SLE from India (INSPIRE).
Methods: The INSPIRE database includes patients satisfying the SLICC classification criteria for SLE with disease duration less than 3 years at 10 tertiary care hospitals across India. Myositis was defined by proximal muscle aching/weakness, associated with elevated CPK or LDH or AST or ALT. Other causes/drug induced myopathy or muscle enzyme elevation were excluded. Data on demographics, clinical, lab features, autoantibodies, and disease activity (SLEDAI, BILAG score), damage (SDI) and mortality were retrieved from the electronic database. SLE patients with myositis (cases) were compared with those not having myositis (controls). Difference in means between groups was done using student's t-test and difference in proportions using the chi-square test. Presence of infection, BILAG category A or B disease in any domain, myositis, gender were used as predictors of mortality using binomial logistic regression.
Results: A total of 2210 patients including 2029 (91.8%) females were enrolled in the study. Mean (SD) age at diagnosis was 28.9±0.79 years. Mean (SD) duration of disease was 16.4±0.45 months. Comorbidities included hypothyroidism (16.4%), hypertension in (8.8%), diabetes mellitus (1.6%). 133 patients died during mean follow-up of 22.4±12.5 months.125 (5.6%) patients had myositis, with myalgia present in 88%. On univariate analysis, cases were younger, with more frequent fever, acute cutaneous lupus, oral ulcers, pleural effusion, leukopenia, thrombocytopenia, lower haemoglobin, complements, and albumin and higher ALT, AST, LDH, CPK. SLEDAI and BILAG scores than controls (Table 1). Antibodies to Ro60 were more frequent in patients with myositis. Twelve cases had muscle damage as assessed by SDI. Patients with myositis had a significantly lower survival (87% vs 94%, p< 0.001, Figure 1). Univariate analysis identified fever, SLEDAI and CPK as the predictors of myositis at p< 0.05. Binomial logistic regression identified infection as a predictor of mortality at p< 0.03.
Conclusion: The prevalence of myositis in an Indian lupus cohort with early, very active disease was 5.6 %. Those with myositis had more active disease elsewhere, had similar damage but lower survival than those without. Myositis was not a predictor of mortality.
 Survival in patients with Myositis
Survival in patients with Myositis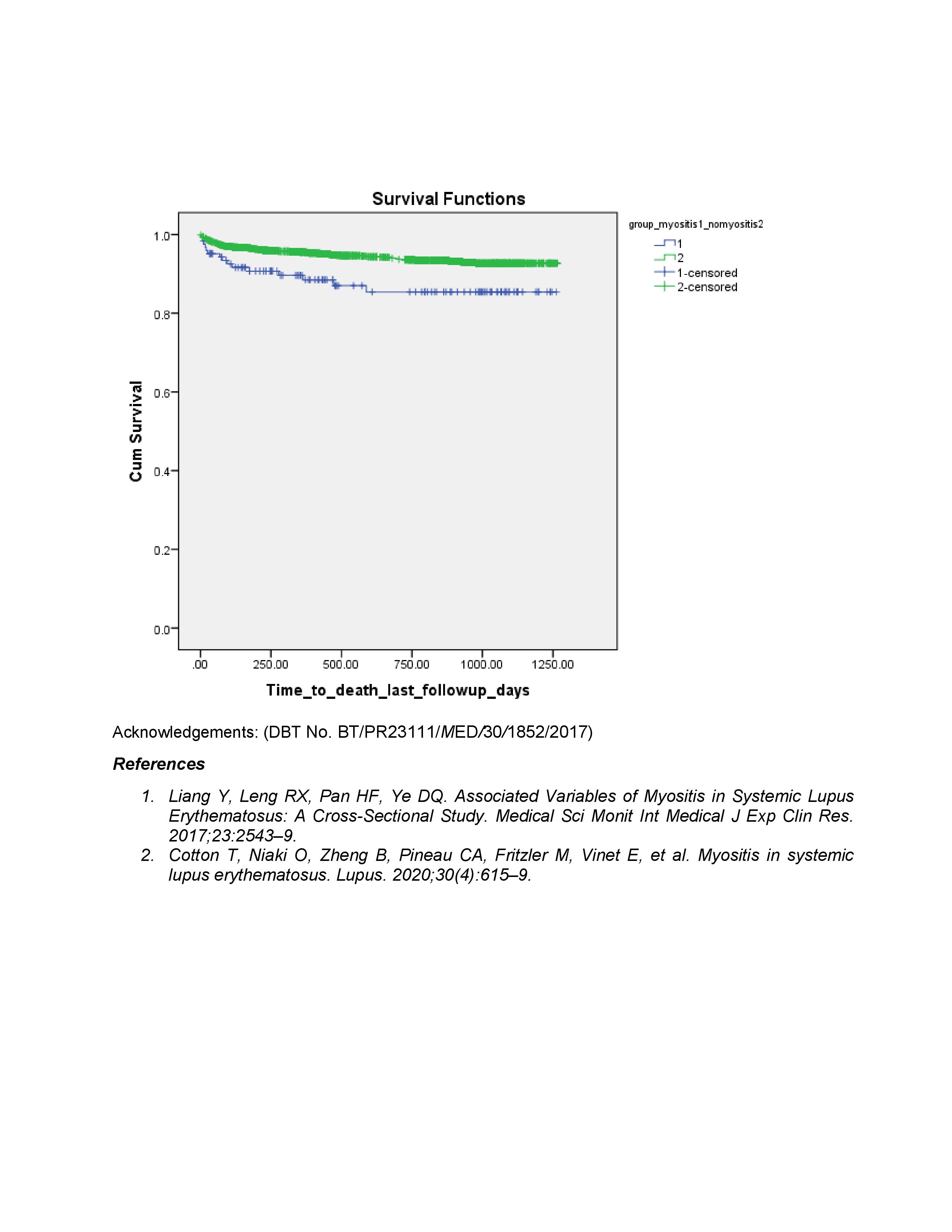
Disclosures: L. Rajasekhar, None; V. Shobha, None; M. Ponnana, None; C. Kavadichanda, None; A. Mathew, None; S. Tripathy, None; M. Rathi, None; P. Ghosh, None; R. Gupta, None; A. Jain, None; A. Aggarwal, None.

