Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1186–1214) Epidemiology and Public Health Poster II
1207: Risk Factors for Major Cardiovascular Events (MACE) in Inflammatory Arthritis: A Time-dependent Analysis on the Inflammatory Burden, Use of DMARDs, NSAIDs, and Steroid
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- HM
Huan Meng, PhD
The Faculty of Medicine, CUHK
Hong Kong, Hong Kong, China
Abstract Poster Presenter(s)
Huan Meng1, Steven H Lam2, Ho So1 and Lai-shan Tam3, 1The Faculty of Medicine, CUHK, Hong Kong, Hong Kong, 2The Chinese university of Hong Kong, Hong Kong, Hong Kong, 3The Chinese University of Hong Kong, Hong Kong, China
Background/Purpose: Inflammatory arthritis (IA) including rheumatoid arthritis (RA) and psoriatic arthritis (PsA) is associated with accelerated atherosclerosis due to systematic inflammation. To elucidate whether inflammatory burden (c-reactive protein [CRP] and erythrocyte sedimentation rate [ESR] levels) and drugs used to suppress inflammation (disease-modifying anti-rheumatic drugs [DMARDs], non-steroidal anti-inflammatory drugs [NSAIDs]) and steroid over time are independently associated with major cardiovascular events (MACE) in patients with IA.
Methods: A population-based cohort of IA patients was identified in the citywide database of the Hong Kong Hospital Authority. IA patients recruited from Jan 2006 to Dec 2015 were followed until the end of 2018. The outcome was the occurrence of a first MACE, defined as unstable angina, acute myocardial infarction, stroke/transient ischemic attack, or death from cardiovascular causes. Cox proportional hazard models with time-varying CRP and ESR levels and drugs used were analyzed to identify the risk of having MACE in IA patients.
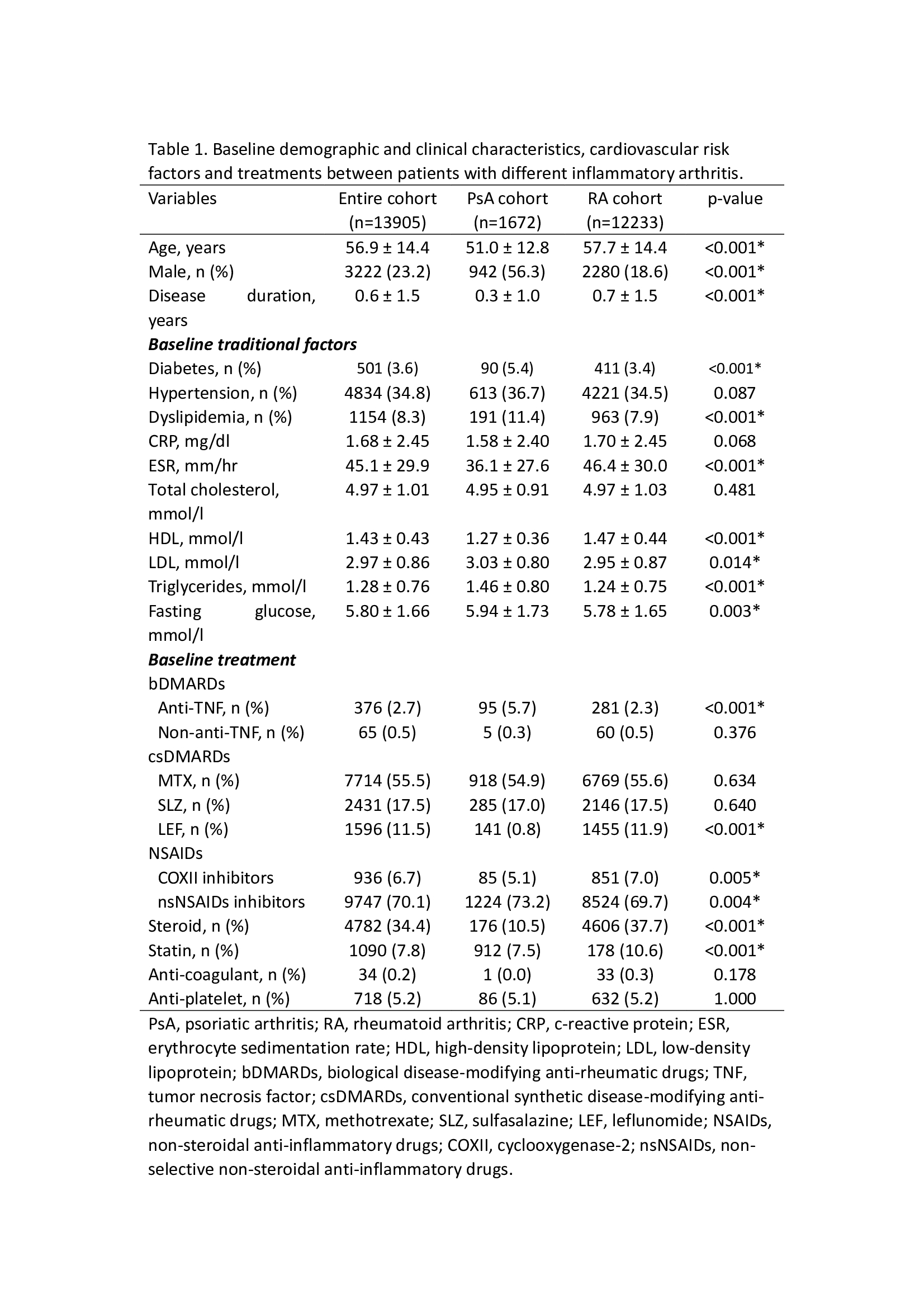
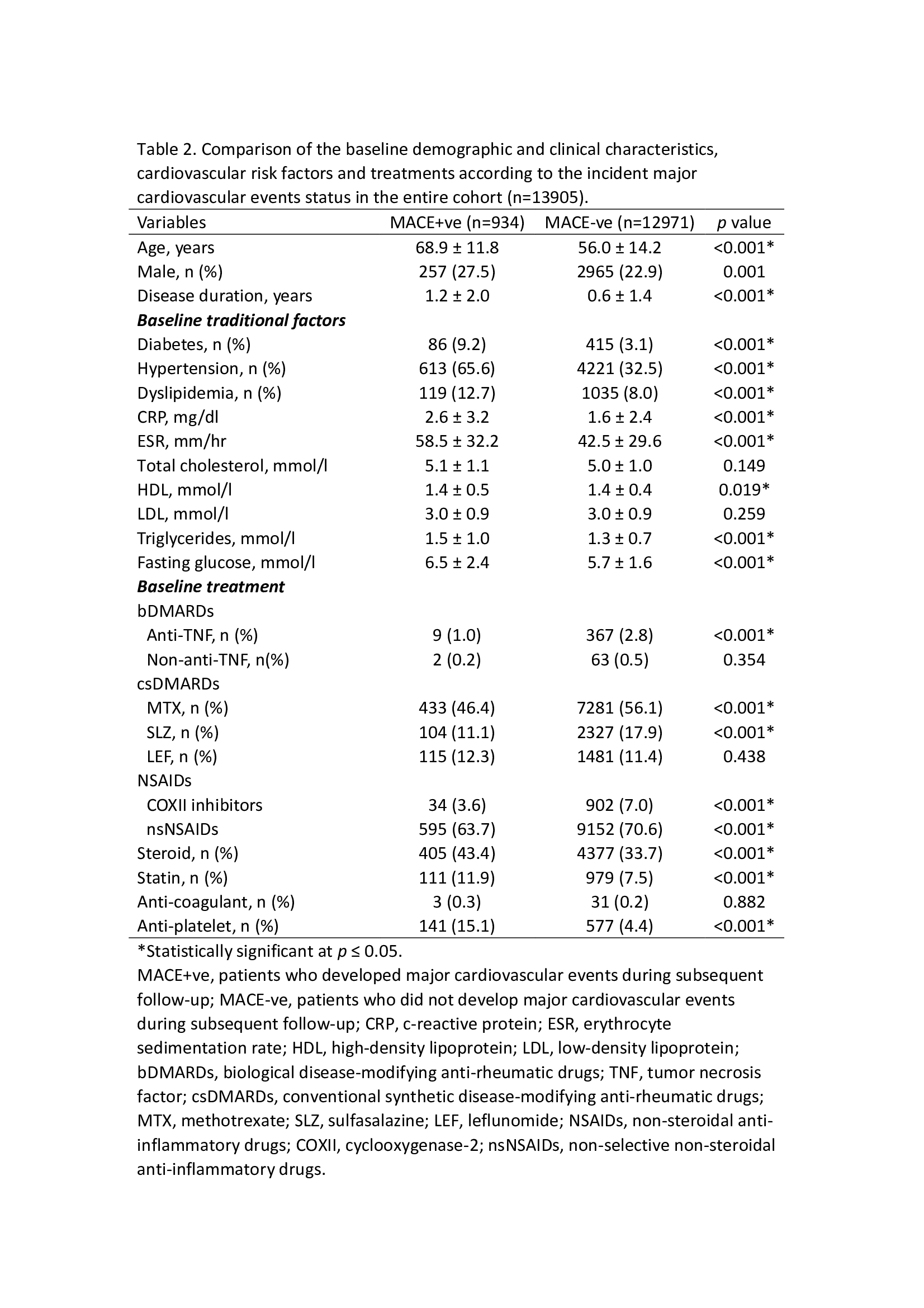
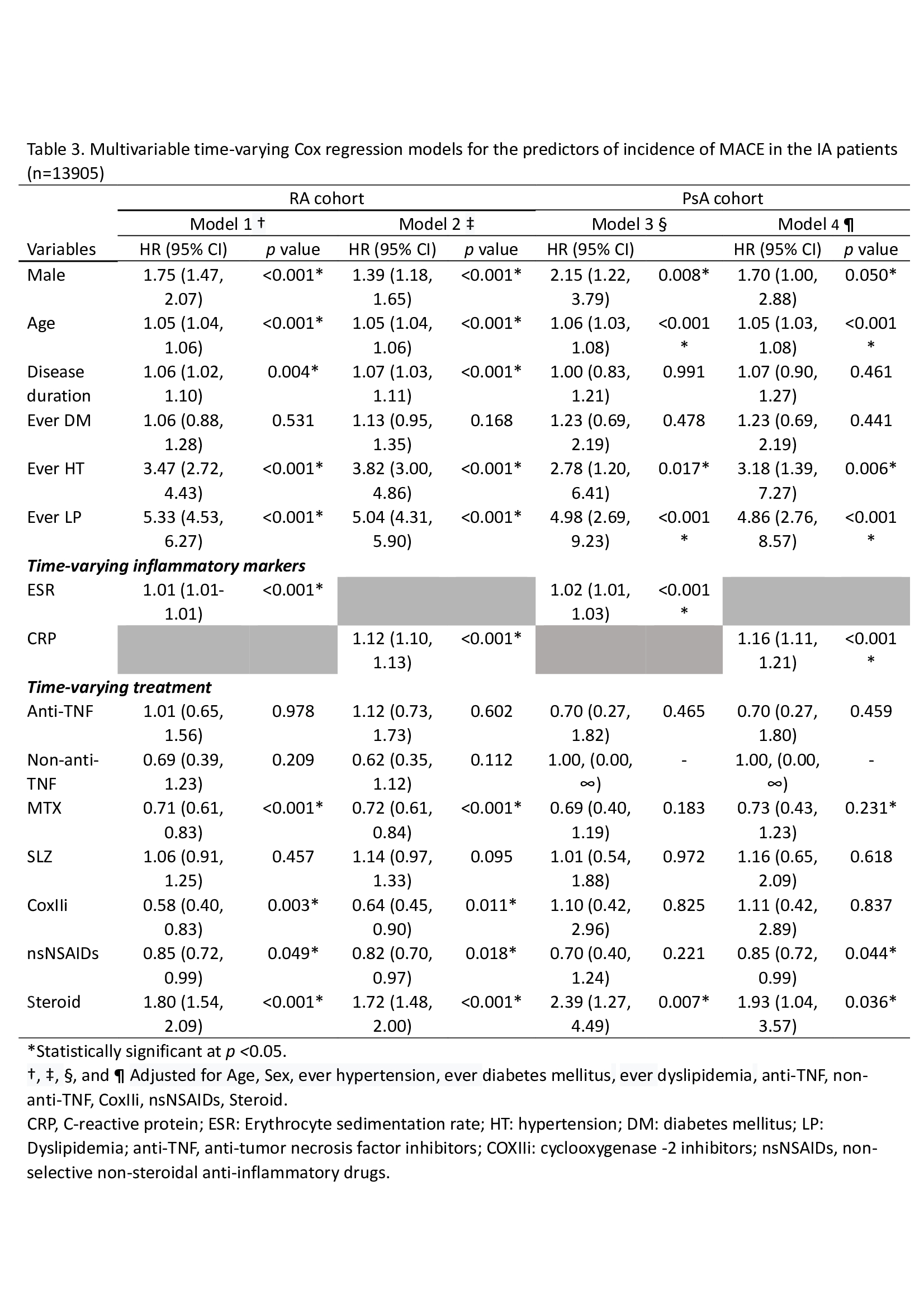
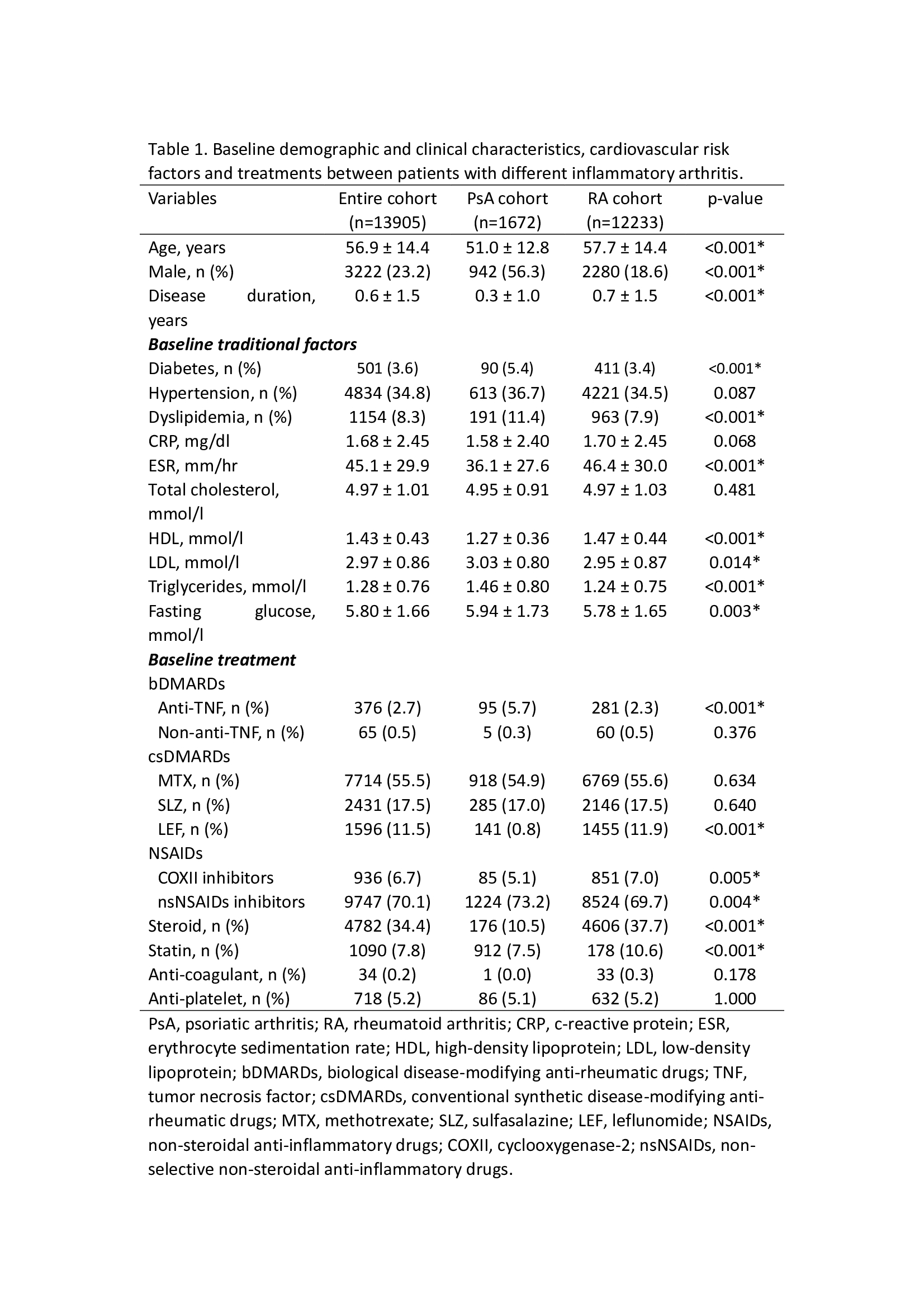
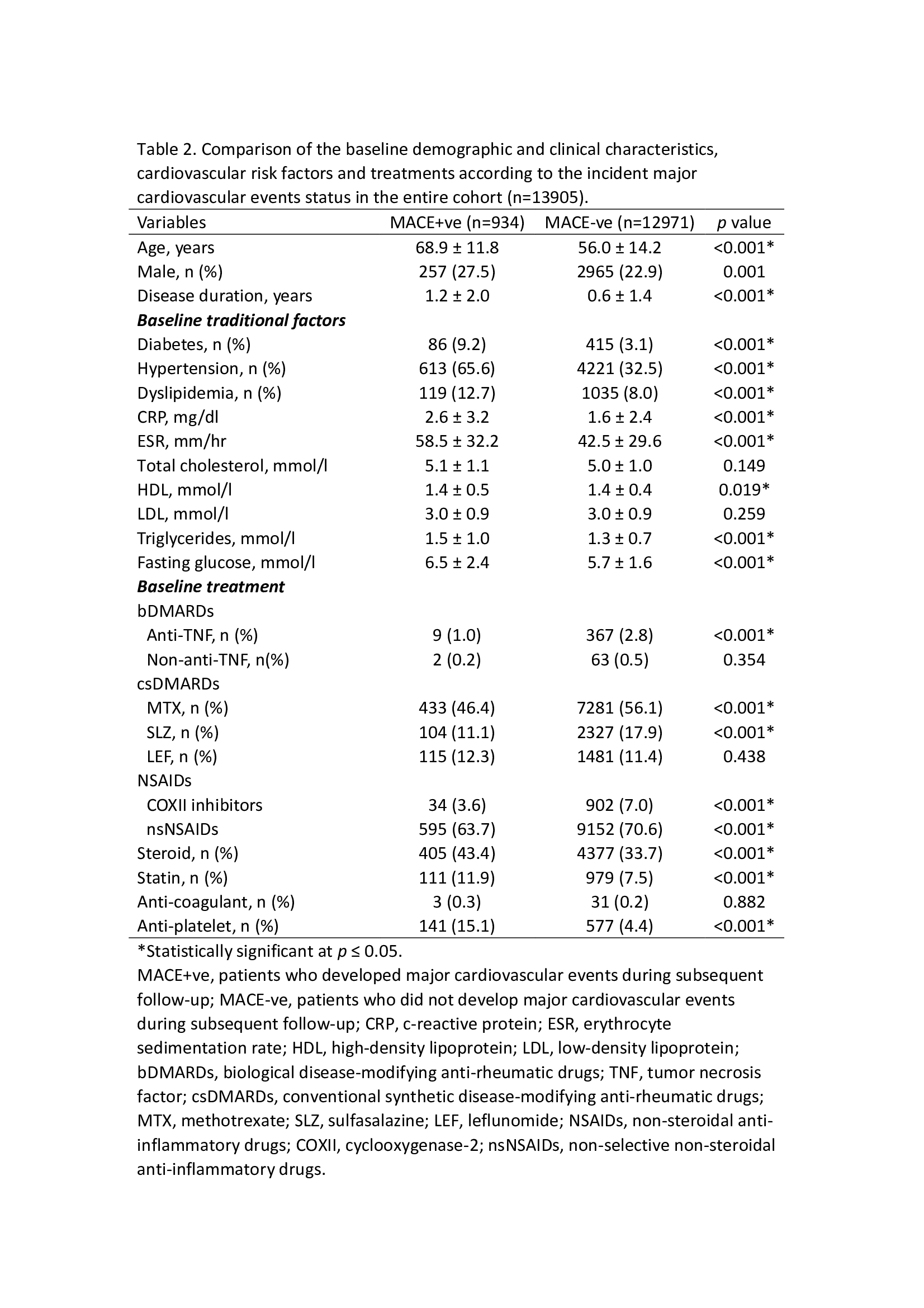
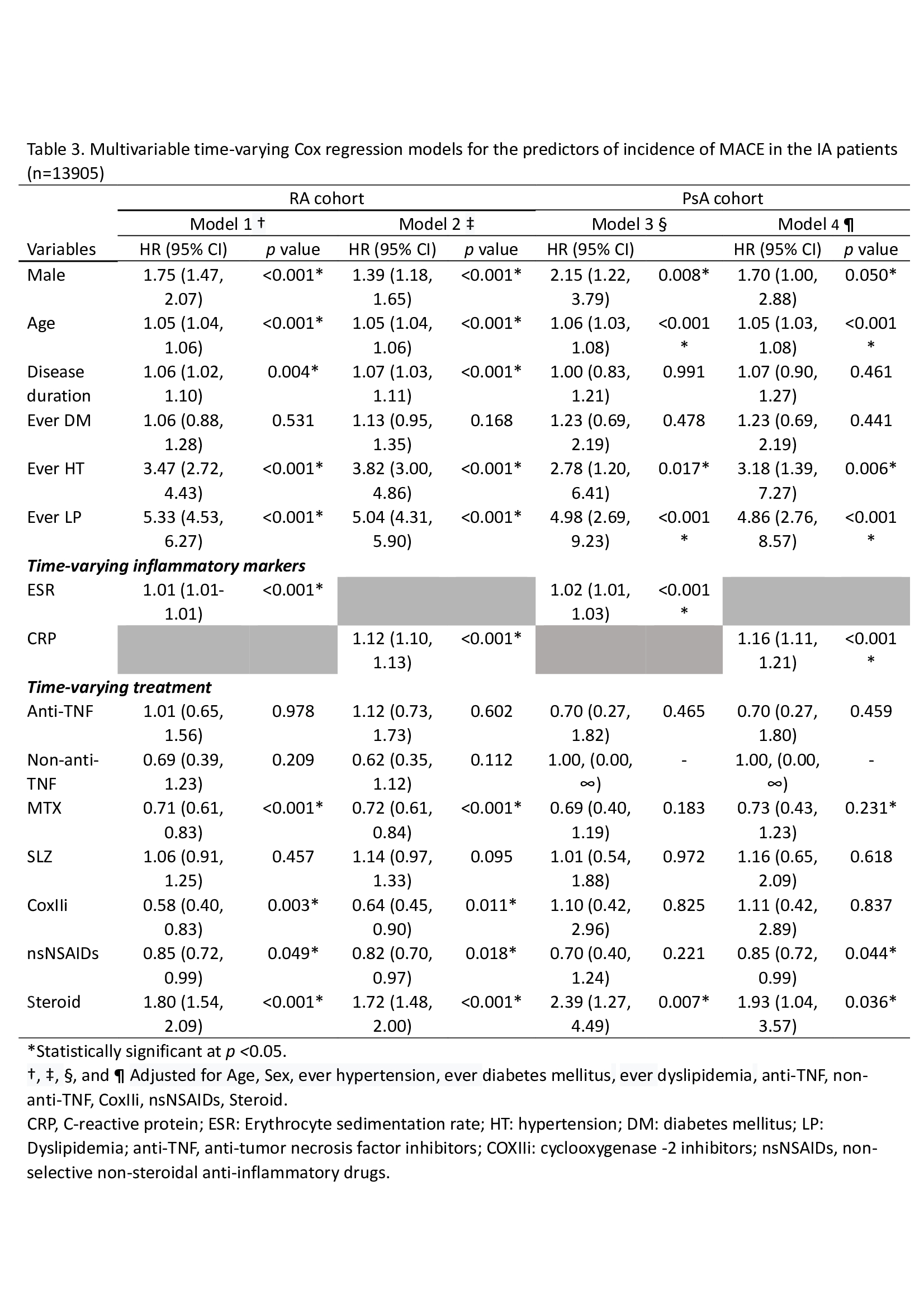
Results: A total of 13,905 (12,233 RA patients, 1,672 PsA patients) patients with IA were recruited (Table 1), with 119,571 patient-years follow-up. 934 (7.0 %) patients developed a first MACE. At baseline, the MACE+ve group were older (68.9±11.8 vs 56.0±14.2, p< 0.001), had more traditional cardiovascular risk factors, higher levels of CRP (2.6±3.2 vs 1.6±2.4, p< 0.001) and ESR (58.8±32.2 vs 42.5±29.6, p< 0.001), more exposure to steroid (43.4% vs 33.7%, p< 0.001) and less exposure to anti-tumor necrosis factor inhibitors (anti-TNF) (1.0% vs 2.8%, p< 0.001), methotrexate (MTX) (46.5% vs 56.1%, p< 0.001), COXII inhibitors (COXIIi) (3.6% vs 7.0%, p< 0.001), non-selective NSAIDs (nsNSAIDs) (63.7% vs 70.6%, p< 0.001) compared to MACE-ve group (Table 2). After adjusting for age, sex, traditional cardiovascular comorbidities using multivariable cox regression analysis, higher inflammatory burden (as reflected by the time-varying ESR levels [hazard ratio {HR} 1.01, 95% confidence interval {CI} 1.01-1.01, p< 0.001] in RA and [HR 1.02, 95%CI 1.01-1.03, p< 0.001] in PsA), time-varying CRP ([HR 1.12, 95% CI 1.10-1.13, p< 0.001] in RA and [HR 1.16, 95% CI 1.11-1.21, p< 0.001] in PsA) and the use of steroid ([HR 1.72-1.80] in RA and [HR 1.93-2.39] in PsA) were independently associated with a higher risk of developing MACE. In contrast, exposure to MTX (HR 1.71-1.72), COXIIi (HR 0.58-0.64) and nsNSAIDs (HR 0.82-0.85) had a protective effect against MACE in RA cohort in the multivariate model. While biologic DMARDs were not associated with MACE in both RA and PsA (Table 3).
Conclusion: Increased inflammatory burden as reflected by elevated ESR and CRP level over time, and increased exposure to steroid were independently associated with increased risk of MACE in IA, while the risk was significantly reduced with MTX and NSAIDs use in RA patients.
Disclosures: H. Meng, None; S. Lam, None; H. So, None; L. Tam, AbbVie, Amgen, Boehringer-Ingelheim, Eli Lilly, GlaxoSmithKlein(GSK), Janssen, Novartis, Pfizer, Sanofi, AstraZeneca.
Background/Purpose: Inflammatory arthritis (IA) including rheumatoid arthritis (RA) and psoriatic arthritis (PsA) is associated with accelerated atherosclerosis due to systematic inflammation. To elucidate whether inflammatory burden (c-reactive protein [CRP] and erythrocyte sedimentation rate [ESR] levels) and drugs used to suppress inflammation (disease-modifying anti-rheumatic drugs [DMARDs], non-steroidal anti-inflammatory drugs [NSAIDs]) and steroid over time are independently associated with major cardiovascular events (MACE) in patients with IA.
Methods: A population-based cohort of IA patients was identified in the citywide database of the Hong Kong Hospital Authority. IA patients recruited from Jan 2006 to Dec 2015 were followed until the end of 2018. The outcome was the occurrence of a first MACE, defined as unstable angina, acute myocardial infarction, stroke/transient ischemic attack, or death from cardiovascular causes. Cox proportional hazard models with time-varying CRP and ESR levels and drugs used were analyzed to identify the risk of having MACE in IA patients.
Results: A total of 13,905 (12,233 RA patients, 1,672 PsA patients) patients with IA were recruited (Table 1), with 119,571 patient-years follow-up. 934 (7.0 %) patients developed a first MACE. At baseline, the MACE+ve group were older (68.9±11.8 vs 56.0±14.2, p< 0.001), had more traditional cardiovascular risk factors, higher levels of CRP (2.6±3.2 vs 1.6±2.4, p< 0.001) and ESR (58.8±32.2 vs 42.5±29.6, p< 0.001), more exposure to steroid (43.4% vs 33.7%, p< 0.001) and less exposure to anti-tumor necrosis factor inhibitors (anti-TNF) (1.0% vs 2.8%, p< 0.001), methotrexate (MTX) (46.5% vs 56.1%, p< 0.001), COXII inhibitors (COXIIi) (3.6% vs 7.0%, p< 0.001), non-selective NSAIDs (nsNSAIDs) (63.7% vs 70.6%, p< 0.001) compared to MACE-ve group (Table 2). After adjusting for age, sex, traditional cardiovascular comorbidities using multivariable cox regression analysis, higher inflammatory burden (as reflected by the time-varying ESR levels [hazard ratio {HR} 1.01, 95% confidence interval {CI} 1.01-1.01, p< 0.001] in RA and [HR 1.02, 95%CI 1.01-1.03, p< 0.001] in PsA), time-varying CRP ([HR 1.12, 95% CI 1.10-1.13, p< 0.001] in RA and [HR 1.16, 95% CI 1.11-1.21, p< 0.001] in PsA) and the use of steroid ([HR 1.72-1.80] in RA and [HR 1.93-2.39] in PsA) were independently associated with a higher risk of developing MACE. In contrast, exposure to MTX (HR 1.71-1.72), COXIIi (HR 0.58-0.64) and nsNSAIDs (HR 0.82-0.85) had a protective effect against MACE in RA cohort in the multivariate model. While biologic DMARDs were not associated with MACE in both RA and PsA (Table 3).
Conclusion: Increased inflammatory burden as reflected by elevated ESR and CRP level over time, and increased exposure to steroid were independently associated with increased risk of MACE in IA, while the risk was significantly reduced with MTX and NSAIDs use in RA patients.
Disclosures: H. Meng, None; S. Lam, None; H. So, None; L. Tam, AbbVie, Amgen, Boehringer-Ingelheim, Eli Lilly, GlaxoSmithKlein(GSK), Janssen, Novartis, Pfizer, Sanofi, AstraZeneca.

