Back
Poster Session A
Vasculitis
Session: (0458–0497) Vasculitis – Non-ANCA-Associated and Related Disorders Poster I: Giant Cell Arteritis
0497: Classification Criteria and Existing Pre-Test Probability Stratification Tools Perform Poorly in Diagnosing Giant Cell Arteritis
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- VY
Victor Yang, MBBS
Austin Health
Heidelberg, Victoria, Australia
Abstract Poster Presenter(s)
Victor Yang1, Christopher McMaster1, Claire Owen2, Jessica Leung3, Bonnia Liu1, Russell Buchanan4 and David Liew4, 1Austin Health, Melbourne, Australia, 2Austin Health, Malvern East, Australia, 3Austin Health, Preston, Victoria, Australia, 4Austin Health, Heidelberg, Australia
Background/Purpose: The 2022 ACR/EULAR GCA classification criteria are a major advance which will underpin future scientific advancement by classifying patients already diagnosed with primary systemic vasculitis, which is the purpose they are designed for. Unfortunately, they will inevitably be inappropriately employed for diagnosis by some, despite clear communication to the contrary. Given that temporal artery biopsy and imaging techniques insufficiently delineate many patients, the clinical diagnosis of GCA is frequently reliant on likelihood ratio calculation. Pre-test probability stratification tools integrate much of this calculation, but are currently underutilized. We sought to examine the performance of classification criteria and existing stratification tools in the diagnosis of GCA.
Methods: We examined the performance of the 2022 and 1990 ACR/EULAR classification criteria, and the Southend GCA pre-test probability score. We included all patients at our center between 2011 to 2020 who were considered sufficiently likely to have had GCA as to have had a temporal artery biopsy, and on retrospective chart review compared clinical characteristics based on the eventual diagnosis after at least six months. Diagnostic GCA imaging was only rarely used at our center during this time period, but any patients who had undergone this were excluded. We determined independently predictive variables based on regularization via LASSO regression.
Results: In this current set of 268 patients, 66 patients were eventually diagnosed with GCA, including 46 with a positive TAB. The remaining 128 patients (i.e. mimics) had a broad array of other diagnoses, and in 74 patients, no final diagnosis was attributed. Notably, the only non-laboratory disease manifestations positively predicting GCA were jaw pain and diplopia (Figure), although fever and inflammatory arthritis predicted mimics. The strongest predictor was a higher serum platelet count, similar to findings elsewhere, although most patients had normal reporting range values. The 2022 ACR/EULAR criteria achieved a receiver operating characteristic area under the curve (AUC) of 0.72 (95% CI 0.64-0.79), similar to the 1990 criteria achieving an AUC of 0.75 (95% CI 0.68-0.82); performance dropped further when temporal artery biopsy was excluded. The Southend GCAPS achieved an AUC of 0.63 (95% CI 0.55-0.71), with the GCAPS high-risk cut-off (GCAPS≥13) had a sensitivity of 17% and a specificity of 90%. The optimal cut-off by Youden's index was GCAPS≥8, with a sensitivity of 89% but only specificity of 35%.
Conclusion: While this is just one center's experience, in this study the ACR/EULAR classification criteria appear inappropriate for diagnostic purposes. Other conventional factors, such as single clinical or laboratory characteristics and existing stratification tools, are also insufficient in isolation to make a diagnosis. Appropriate compound diagnostic tools need to be developed for GCA diagnosis. While machine learning using collaborative data sets will likely lead to advances in supporting the diagnosis of biopsy-negative GCA, explainability, rigorous validation, and regulation are likely to engender clinical confidence.
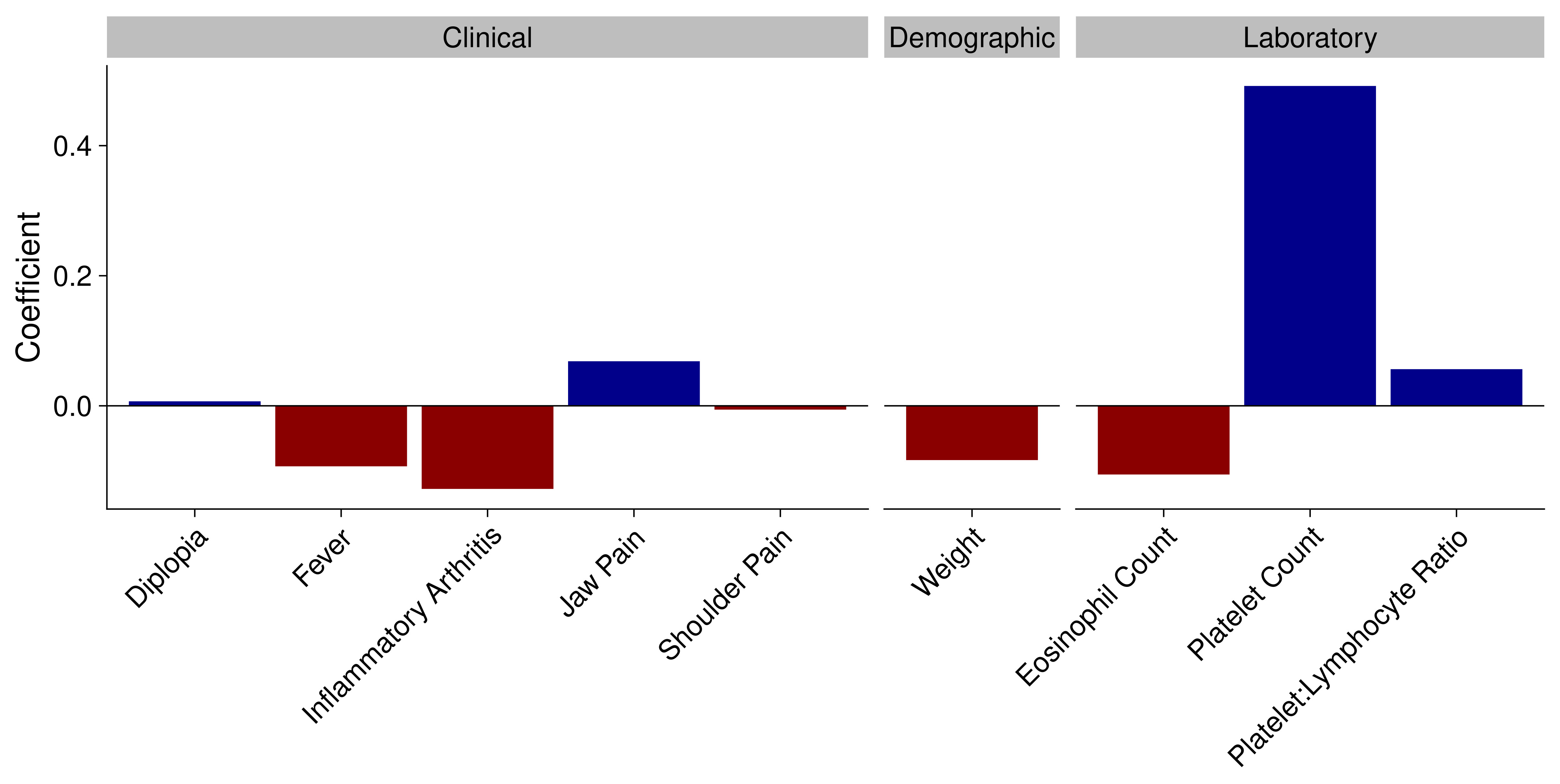 Clinical characteristics and their association with giant cell arteritis. Model co-efficient listed only for variables independently predictive on a multivariable model using LASSO regression. All variables have been centred and scaled, enabling direct comparison of coefficients.
Clinical characteristics and their association with giant cell arteritis. Model co-efficient listed only for variables independently predictive on a multivariable model using LASSO regression. All variables have been centred and scaled, enabling direct comparison of coefficients.
Disclosures: V. Yang, None; C. McMaster, None; C. Owen, None; J. Leung, Novartis, Fresenius Kabi, Eli Lilly, AbbVie; B. Liu, Eli Lilly; R. Buchanan, None; D. Liew, None.
Background/Purpose: The 2022 ACR/EULAR GCA classification criteria are a major advance which will underpin future scientific advancement by classifying patients already diagnosed with primary systemic vasculitis, which is the purpose they are designed for. Unfortunately, they will inevitably be inappropriately employed for diagnosis by some, despite clear communication to the contrary. Given that temporal artery biopsy and imaging techniques insufficiently delineate many patients, the clinical diagnosis of GCA is frequently reliant on likelihood ratio calculation. Pre-test probability stratification tools integrate much of this calculation, but are currently underutilized. We sought to examine the performance of classification criteria and existing stratification tools in the diagnosis of GCA.
Methods: We examined the performance of the 2022 and 1990 ACR/EULAR classification criteria, and the Southend GCA pre-test probability score. We included all patients at our center between 2011 to 2020 who were considered sufficiently likely to have had GCA as to have had a temporal artery biopsy, and on retrospective chart review compared clinical characteristics based on the eventual diagnosis after at least six months. Diagnostic GCA imaging was only rarely used at our center during this time period, but any patients who had undergone this were excluded. We determined independently predictive variables based on regularization via LASSO regression.
Results: In this current set of 268 patients, 66 patients were eventually diagnosed with GCA, including 46 with a positive TAB. The remaining 128 patients (i.e. mimics) had a broad array of other diagnoses, and in 74 patients, no final diagnosis was attributed. Notably, the only non-laboratory disease manifestations positively predicting GCA were jaw pain and diplopia (Figure), although fever and inflammatory arthritis predicted mimics. The strongest predictor was a higher serum platelet count, similar to findings elsewhere, although most patients had normal reporting range values. The 2022 ACR/EULAR criteria achieved a receiver operating characteristic area under the curve (AUC) of 0.72 (95% CI 0.64-0.79), similar to the 1990 criteria achieving an AUC of 0.75 (95% CI 0.68-0.82); performance dropped further when temporal artery biopsy was excluded. The Southend GCAPS achieved an AUC of 0.63 (95% CI 0.55-0.71), with the GCAPS high-risk cut-off (GCAPS≥13) had a sensitivity of 17% and a specificity of 90%. The optimal cut-off by Youden's index was GCAPS≥8, with a sensitivity of 89% but only specificity of 35%.
Conclusion: While this is just one center's experience, in this study the ACR/EULAR classification criteria appear inappropriate for diagnostic purposes. Other conventional factors, such as single clinical or laboratory characteristics and existing stratification tools, are also insufficient in isolation to make a diagnosis. Appropriate compound diagnostic tools need to be developed for GCA diagnosis. While machine learning using collaborative data sets will likely lead to advances in supporting the diagnosis of biopsy-negative GCA, explainability, rigorous validation, and regulation are likely to engender clinical confidence.
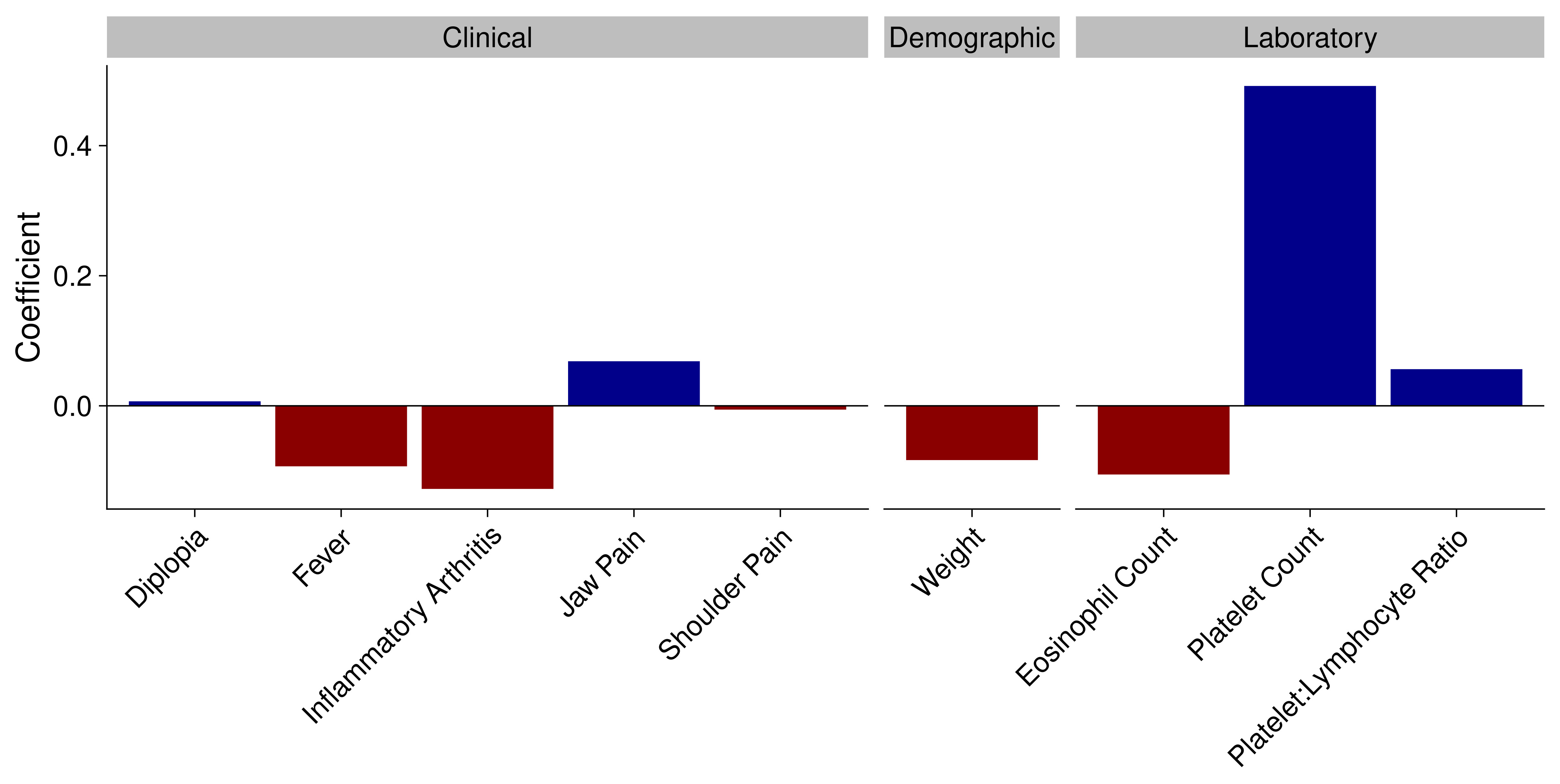 Clinical characteristics and their association with giant cell arteritis. Model co-efficient listed only for variables independently predictive on a multivariable model using LASSO regression. All variables have been centred and scaled, enabling direct comparison of coefficients.
Clinical characteristics and their association with giant cell arteritis. Model co-efficient listed only for variables independently predictive on a multivariable model using LASSO regression. All variables have been centred and scaled, enabling direct comparison of coefficients.Disclosures: V. Yang, None; C. McMaster, None; C. Owen, None; J. Leung, Novartis, Fresenius Kabi, Eli Lilly, AbbVie; B. Liu, Eli Lilly; R. Buchanan, None; D. Liew, None.

