Back
Poster Session C
Imaging
Session: (1228–1266) Imaging of Rheumatic Diseases Poster
1243: The Impact of MRI Slice Thickness on the Detection of Spinal Syndesmophytes in Axial Spondyloarthritis
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- XB
Xenofon Baraliakos, MD
Rheumazentrum Ruhrgebiet Herne
Herne, Germany
Abstract Poster Presenter(s)
Kalliopi Klavdianou1, Alexaner Dieter Mewes2, Styliani Tsiami3, Philipp Sewerin4 and Xenofon Baraliakos5, 1'Asklepieion' General Hospital, Department of Rheumatology, Voula, Athens, Greece, 2University Dusseldorf, Medical Faculty, Department of Diagnostic and Interventional Radiology, Dusseldorf, Germany, 3Rheumazentrum Ruhrgebiet, Herne, Ruhr-University Bochum, Herne, Germany, 4Rheumazentrum Ruhrgebiet, Ruhr-Universität-Bochum, Herne, Germany, 5Rheumazentrum Ruhrgebiet Herne, Herne, Germany
Background/Purpose: Conventional radiographs (CR) are the gold standard for detecting syndesmophytes in axial Spondyloarthritis (axSpA), mainly because magnetic resonance imaging (MRI) is not able to detect thin bony structures due to its slicing technique. We aimed to assess the ability and performance of detection of syndesmophytes using different slice thicknesses on MRI and compare them with findings on CR.
Methods: MRI with T1W and STIR images with slice thicknesses of 1-6mm and CR of the lower thoracic and lumbar spine performed on the same day were prospectively performed in 43 axSpA patients. Clinical and laboratory characteristics of the patients from the same timepoint were available. Each vertebral corner (VC) (anterior superior and posterior, inferior anterior and posterior) from the thoracic (Th11) to the lumbar (L5) vertebral body were assessed for the presence/absence of syndesmophytes but also fat lesion (FL) on MRI by two experienced readers (one radiologist and one rheumatologist) independently. Disagreements were solved in consensus.
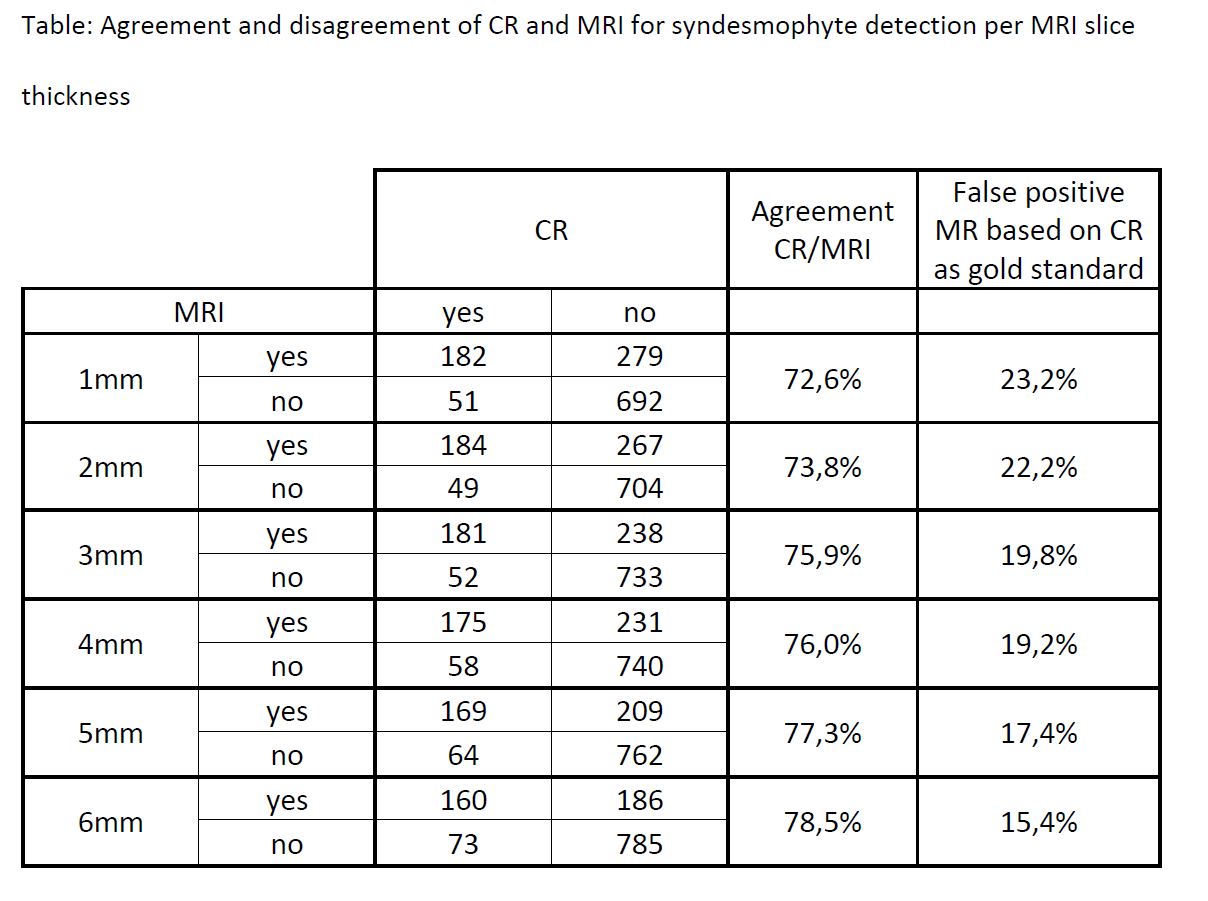
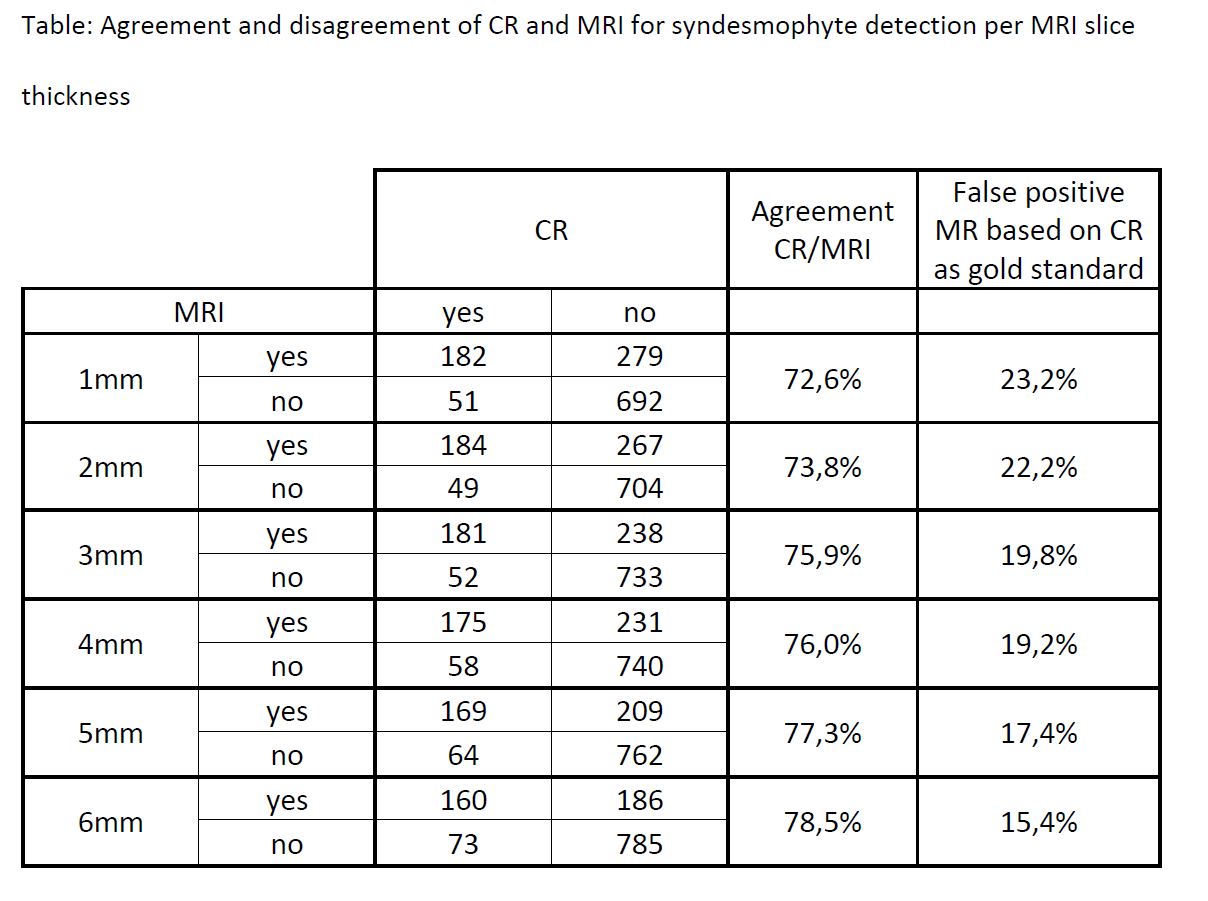
Results: A total of 1.204 VCs was assessed from all patients. The mean time needed for scoring the MRIs varied between 2:27 and 4:12min for the MRI thicknesses of 1-6mm, respectively. Syndesmophytes were detected in 19.3% VCs on CR and in 38.3%, 37.5%, 34.8%, 33.7%, 31.4%, 28.7% VCs on MRI slice thicknesses of 1-6mm, respectively (p≤0.001 for all MRI vs. CR evaluations and within MRI slice thicknesses). The anterior superior VC of L1 was the most affected site among all vertebral corners in all MRI slice thicknesses and CRs. In thoracic spine , the anterior superior corner of T12 was the most frequently affected site in both MRI (all slice thicknesses) and CR. Although MRI could detect more syndesmophytes in both lumbar and thoracic vertebrae than CR, MRI at any slice thickness could not detect 15.4%-23.2% of syndesmophytes detected in CR (Table). Fat lesions were detected in 38.3%, 37.5%, 34.8%, 33.7%, 31.4%, 28.7% of VC with MRI slice thicknesses of 1-6mm, respectively. MRI slice thickness had no role in detecting fat lesions (p >0.05 within MRI slice thicknesses).
Conclusion: MRI of the lower thoracic and the lumbar spine at any slice thickness detected more syndesmophytes than CR, but the best agreement and least false-positive findings on MRI based on CR as gold standard was found in the thicker slice thicknesses. The presence of fat lesions did not influence syndesmophyte detection on MRI. These results may influence the performance of spinal MRI in identification of SpAspecific spinal lesions in daily practice.
Disclosures: K. Klavdianou, None; A. Mewes, None; S. Tsiami, None; P. Sewerin, AXIOM Health, Amgen, AbbVie, Biogen, Bristol-Myers Squibb (BMS), Celgene, Chugai Pharma Marketing Ltd. / Chugai Europe, Deutscher Psoriasis-Bund,, Gilead Sciences, Hexal Pharma, Janssen-Cilag, Johnson & Johnson, Lilly / Lilly Europe / Lilly Global, medi-login, Mediri GmbH, Novartis Pharma, Onkowissen GmbH, Pfizer, Roche Pharma, Rheumazentrum Rhein- Ruhr, Sanofi-Genzyme, Spirit Medical Communication, Swedish Orphan Biovitrum, UCB Pharma; X. Baraliakos, AbbVie, Lilly, Galapagos, MSD, Novartis, Pfizer, UCB, Bristol-Myers Squibb, Janssen, Roche, Sandoz, Sanofi.
Background/Purpose: Conventional radiographs (CR) are the gold standard for detecting syndesmophytes in axial Spondyloarthritis (axSpA), mainly because magnetic resonance imaging (MRI) is not able to detect thin bony structures due to its slicing technique. We aimed to assess the ability and performance of detection of syndesmophytes using different slice thicknesses on MRI and compare them with findings on CR.
Methods: MRI with T1W and STIR images with slice thicknesses of 1-6mm and CR of the lower thoracic and lumbar spine performed on the same day were prospectively performed in 43 axSpA patients. Clinical and laboratory characteristics of the patients from the same timepoint were available. Each vertebral corner (VC) (anterior superior and posterior, inferior anterior and posterior) from the thoracic (Th11) to the lumbar (L5) vertebral body were assessed for the presence/absence of syndesmophytes but also fat lesion (FL) on MRI by two experienced readers (one radiologist and one rheumatologist) independently. Disagreements were solved in consensus.
Results: A total of 1.204 VCs was assessed from all patients. The mean time needed for scoring the MRIs varied between 2:27 and 4:12min for the MRI thicknesses of 1-6mm, respectively. Syndesmophytes were detected in 19.3% VCs on CR and in 38.3%, 37.5%, 34.8%, 33.7%, 31.4%, 28.7% VCs on MRI slice thicknesses of 1-6mm, respectively (p≤0.001 for all MRI vs. CR evaluations and within MRI slice thicknesses). The anterior superior VC of L1 was the most affected site among all vertebral corners in all MRI slice thicknesses and CRs. In thoracic spine , the anterior superior corner of T12 was the most frequently affected site in both MRI (all slice thicknesses) and CR. Although MRI could detect more syndesmophytes in both lumbar and thoracic vertebrae than CR, MRI at any slice thickness could not detect 15.4%-23.2% of syndesmophytes detected in CR (Table). Fat lesions were detected in 38.3%, 37.5%, 34.8%, 33.7%, 31.4%, 28.7% of VC with MRI slice thicknesses of 1-6mm, respectively. MRI slice thickness had no role in detecting fat lesions (p >0.05 within MRI slice thicknesses).
Conclusion: MRI of the lower thoracic and the lumbar spine at any slice thickness detected more syndesmophytes than CR, but the best agreement and least false-positive findings on MRI based on CR as gold standard was found in the thicker slice thicknesses. The presence of fat lesions did not influence syndesmophyte detection on MRI. These results may influence the performance of spinal MRI in identification of SpAspecific spinal lesions in daily practice.
Disclosures: K. Klavdianou, None; A. Mewes, None; S. Tsiami, None; P. Sewerin, AXIOM Health, Amgen, AbbVie, Biogen, Bristol-Myers Squibb (BMS), Celgene, Chugai Pharma Marketing Ltd. / Chugai Europe, Deutscher Psoriasis-Bund,, Gilead Sciences, Hexal Pharma, Janssen-Cilag, Johnson & Johnson, Lilly / Lilly Europe / Lilly Global, medi-login, Mediri GmbH, Novartis Pharma, Onkowissen GmbH, Pfizer, Roche Pharma, Rheumazentrum Rhein- Ruhr, Sanofi-Genzyme, Spirit Medical Communication, Swedish Orphan Biovitrum, UCB Pharma; X. Baraliakos, AbbVie, Lilly, Galapagos, MSD, Novartis, Pfizer, UCB, Bristol-Myers Squibb, Janssen, Roche, Sandoz, Sanofi.

