Back
Poster Session C
Pain syndromes, fibromyalgia and regional musculoskeletal disorders
Session: (1215–1227) Fibromyalgia and Other Clinical Pain Syndromes Poster
1217: The Problem of Pain in Rheumatology: Clinical Profiles Associated with Concomitant Diagnoses with Chronic Overlapping Pain Conditions
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- TF
Titilola Falasinnu, PhD
Stanford School of Medicine
Stanford, CA, United States
Abstract Poster Presenter(s)
Titilola Falasinnu1, Yashaar Chaichian2 and Julia Simard3, 1Stanford School of Medicine, Stanford, CA, 2Stanford University, Stanford, CA, 3Stanford University School of Medicine, Palo Alto, CA
Background/Purpose: The chronification of pain is heterogeneous in rheumatology. Chronic overlapping pain conditions (COPCs) such as fibromyalgia, endometriosis, migraine, and back pain may co-occur with one another and in rheumatic diseases. We describe the sociodemographic and clinical profiles associated with concomitant COPCs among patients with rheumatic diseases.
Methods: We retrospectively identified patients visiting rheumatology clinics at a single institution from 2010 to 2020 for five common rheumatic conditions: psoriatic arthritis (PsA), rheumatoid arthritis (RA), Sjögren's syndrome (SjS), systemic lupus erythematosus (SLE), and systemic sclerosis (SSc). We compared sociodemographic, clinical and lifestyle factors by rheumatic condition and by COPC status. We also report sex-stratified diagnosis of COPCs. The primary outcome was diagnostic validation of >1 COPC.
Results: We identified 5992 rheumatology patients: n=846 PsA, n=2605 RA, n=956 SjS, n=975 SLE, and n=610 SSc. >50% of patients had concomitant COPC diagnosis. Patients with SjS had the highest prevalence: 62%. Diagnosis of ≥1 COPC was highest among Black patients, and lowest among Asian patients. Patients using public insurance had a higher prevalence of ≥1 COPC compared to those with private insurance. Patients with ≥1 COPC had more depression and anxiety and more frequent ED visits, surgeries, and hospitalizations.
Conclusion: Our findings suggest that COPCs are strikingly common among patients with rheumatic disease and are associated with lower quality of life and greater healthcare needs. Future research may elucidate drivers of chronic pain and how to best address the unique analgesic needs of this multimorbid population.
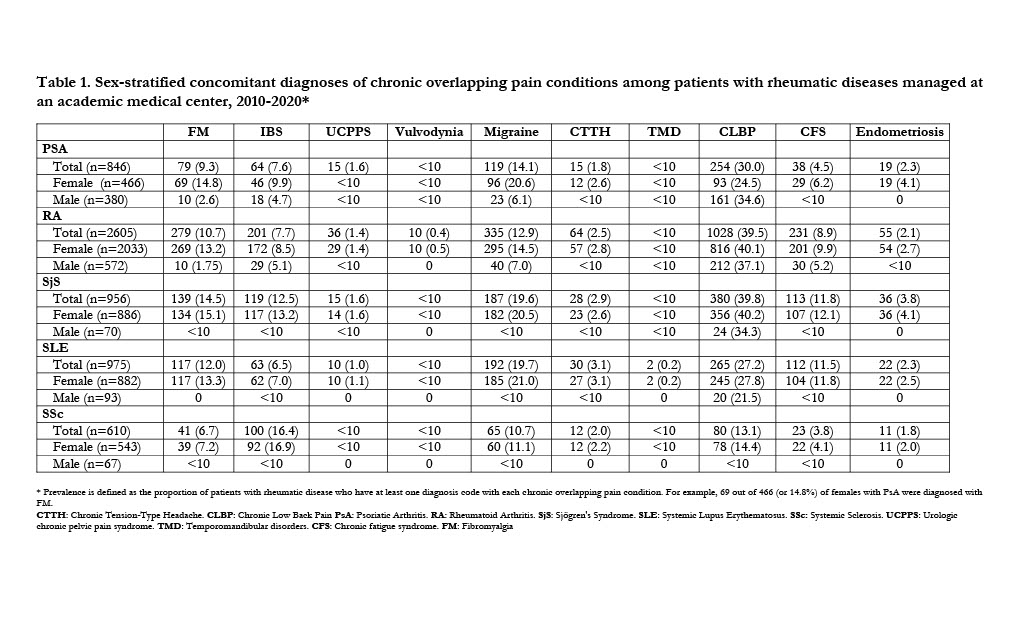 Table 1. Sex-stratified concomitant diagnoses of chronic overlapping pain conditions among patients with rheumatic diseases managed at an academic medical center, 2010-2020*
Table 1. Sex-stratified concomitant diagnoses of chronic overlapping pain conditions among patients with rheumatic diseases managed at an academic medical center, 2010-2020*
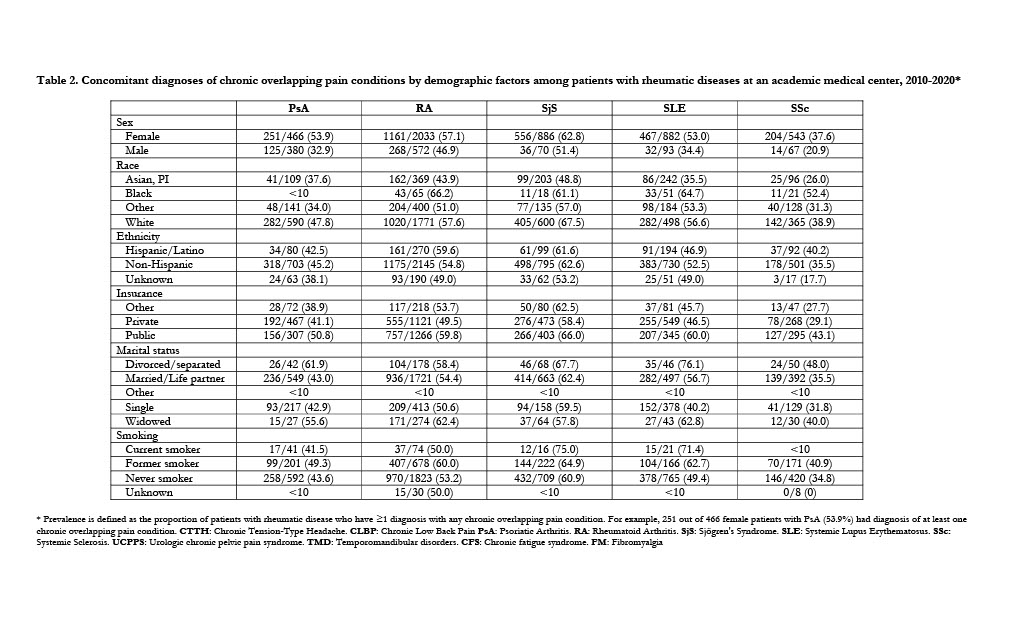 Table 2. Concomitant diagnoses of chronic overlapping pain conditions by demographic factors among patients with rheumatic diseases at an academic medical center, 2010-2020*
Table 2. Concomitant diagnoses of chronic overlapping pain conditions by demographic factors among patients with rheumatic diseases at an academic medical center, 2010-2020*
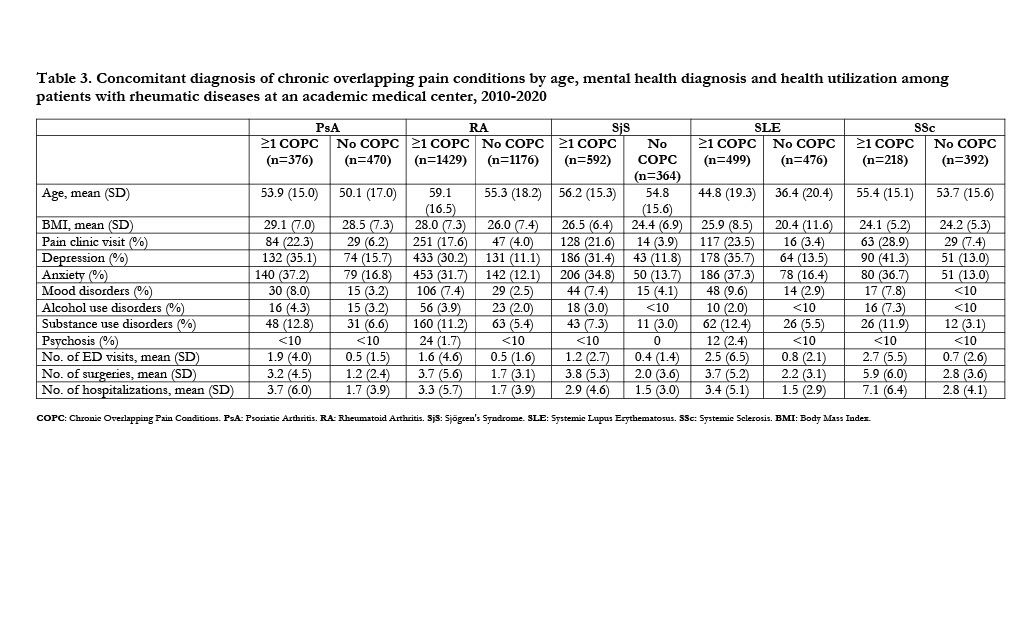 Table 3. Concomitant diagnosis of chronic overlapping pain conditions by age, mental health diagnosis and health utilization among patients with rheumatic diseases at an academic medical center, 2010-2020
Table 3. Concomitant diagnosis of chronic overlapping pain conditions by age, mental health diagnosis and health utilization among patients with rheumatic diseases at an academic medical center, 2010-2020
Disclosures: T. Falasinnu, None; Y. Chaichian, Amgen, Eli Lilly, Boehringer-Ingelheim; J. Simard, None.
Background/Purpose: The chronification of pain is heterogeneous in rheumatology. Chronic overlapping pain conditions (COPCs) such as fibromyalgia, endometriosis, migraine, and back pain may co-occur with one another and in rheumatic diseases. We describe the sociodemographic and clinical profiles associated with concomitant COPCs among patients with rheumatic diseases.
Methods: We retrospectively identified patients visiting rheumatology clinics at a single institution from 2010 to 2020 for five common rheumatic conditions: psoriatic arthritis (PsA), rheumatoid arthritis (RA), Sjögren's syndrome (SjS), systemic lupus erythematosus (SLE), and systemic sclerosis (SSc). We compared sociodemographic, clinical and lifestyle factors by rheumatic condition and by COPC status. We also report sex-stratified diagnosis of COPCs. The primary outcome was diagnostic validation of >1 COPC.
Results: We identified 5992 rheumatology patients: n=846 PsA, n=2605 RA, n=956 SjS, n=975 SLE, and n=610 SSc. >50% of patients had concomitant COPC diagnosis. Patients with SjS had the highest prevalence: 62%. Diagnosis of ≥1 COPC was highest among Black patients, and lowest among Asian patients. Patients using public insurance had a higher prevalence of ≥1 COPC compared to those with private insurance. Patients with ≥1 COPC had more depression and anxiety and more frequent ED visits, surgeries, and hospitalizations.
Conclusion: Our findings suggest that COPCs are strikingly common among patients with rheumatic disease and are associated with lower quality of life and greater healthcare needs. Future research may elucidate drivers of chronic pain and how to best address the unique analgesic needs of this multimorbid population.
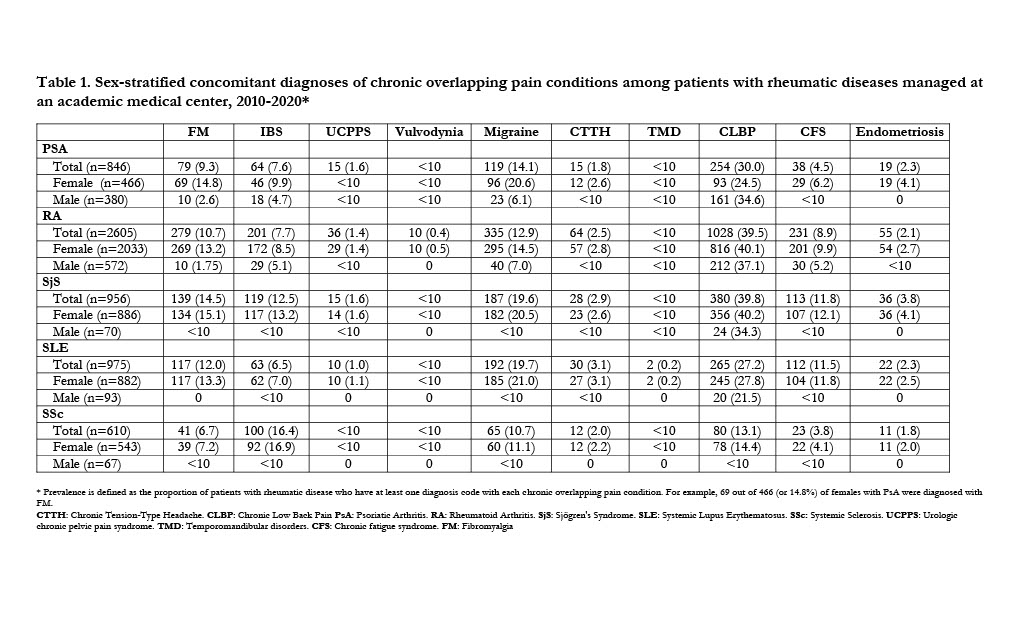 Table 1. Sex-stratified concomitant diagnoses of chronic overlapping pain conditions among patients with rheumatic diseases managed at an academic medical center, 2010-2020*
Table 1. Sex-stratified concomitant diagnoses of chronic overlapping pain conditions among patients with rheumatic diseases managed at an academic medical center, 2010-2020*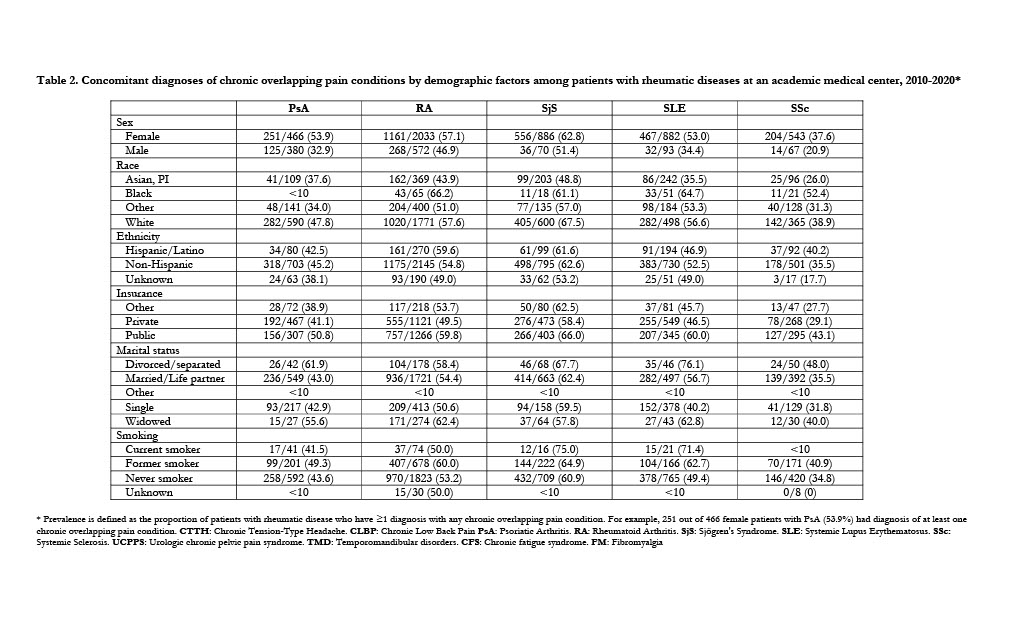 Table 2. Concomitant diagnoses of chronic overlapping pain conditions by demographic factors among patients with rheumatic diseases at an academic medical center, 2010-2020*
Table 2. Concomitant diagnoses of chronic overlapping pain conditions by demographic factors among patients with rheumatic diseases at an academic medical center, 2010-2020*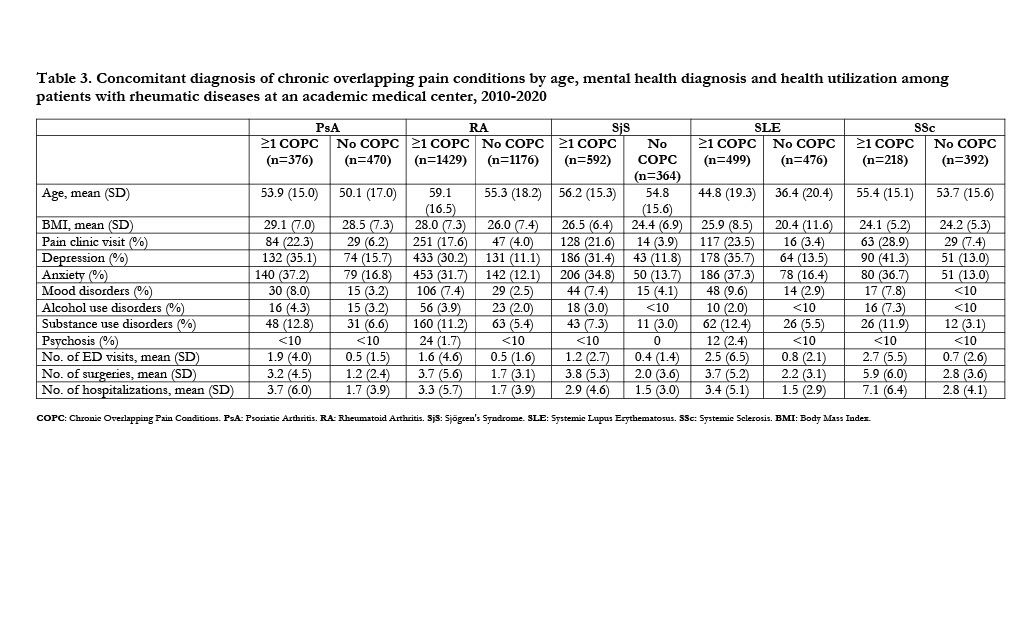 Table 3. Concomitant diagnosis of chronic overlapping pain conditions by age, mental health diagnosis and health utilization among patients with rheumatic diseases at an academic medical center, 2010-2020
Table 3. Concomitant diagnosis of chronic overlapping pain conditions by age, mental health diagnosis and health utilization among patients with rheumatic diseases at an academic medical center, 2010-2020Disclosures: T. Falasinnu, None; Y. Chaichian, Amgen, Eli Lilly, Boehringer-Ingelheim; J. Simard, None.

