Back
Poster Session C
Rheumatoid arthritis (RA)
Session: (1417–1439) RA – Treatment Poster III
1438: The Ratio Between Biological and Glucocorticoid Use in Different Countries Worldwide: Results from the METEOR Registry
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- IN
Isabell Nevins, PhD
LUMC
Wassenaar, Netherlands
Abstract Poster Presenter(s)
Isabell Nevins1, CF Allaart1, David Vega Morales2, Lai Ling Winchow3, Arvind Chopra4, Ana Maria Rodrigues5, Tom Huizinga1, Maarten Boers6 and Sytske Anne Bergstra7, 1Leiden University Medical Center, Leiden, Netherlands, 2Autonomous University of Nuevo León, Monterrey, Mexico, 3Chris hani baragwanath academic hospital, Johannesburg, South Africa, 4Center for Rheumatic Diseases, Pune, Maharashtra, India, 5Reuma.pt, Sociedade Portuguesa de Reumatologia, Lisbon, Portugal, 6Amsterdam UMC, Vrije Universiteit, Amsterdam, Netherlands, 7LUMC, Leiden, Netherlands
Background/Purpose: Previous studies have demonstrated differing bDMARD prescription rates between countries, which seems to be amongst others related to a country's socioeconomic status. In contrast, the costs of glucocorticoids (GC) are significantly lower and it may be hypothesized that when less bDMARDs are used, GC use increases. Therefore, the objective of this study was to investigate globally the ratio between bDMARD and GC use, and to assess whether this relates to a country's socioeconomic status (SES).
Methods: Data on bDMARD and GC use were extracted from the METEOR database: an international database capturing daily clinical practice data from patients with a clinical diagnosis of rheumatoid arthritis (RA). Countries were included that had contributed at least 60 newly diagnosed patients, as of 1-1-2007. The ratio between the proportion of patients who had ever used a bDMARD and the proportion of patients who had ever used a GC (with no concomitant bDMARD use) during a total follow up duration of five years (bDMARD/GC ratio) was calculated per country. Univariable linear regression was used to analyze the bDMARD/GC ratios according to publicly available country-level indicators of SES (measured in GDP per capita, household net disposable income and health expenditure per capita, expressed in International dollar (IntI$) to account for the differences in purchasing power)
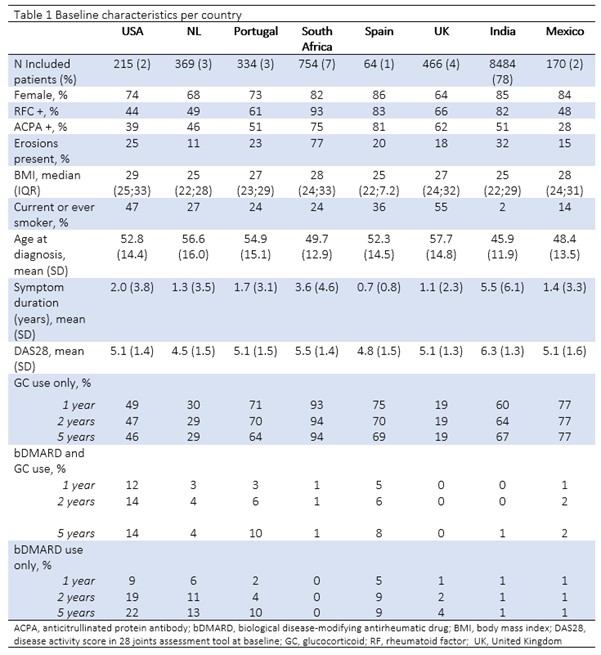
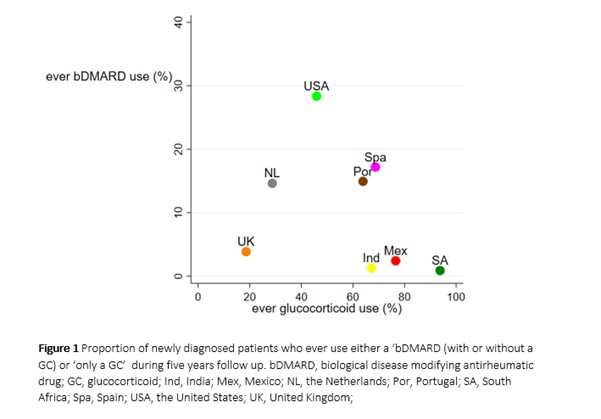
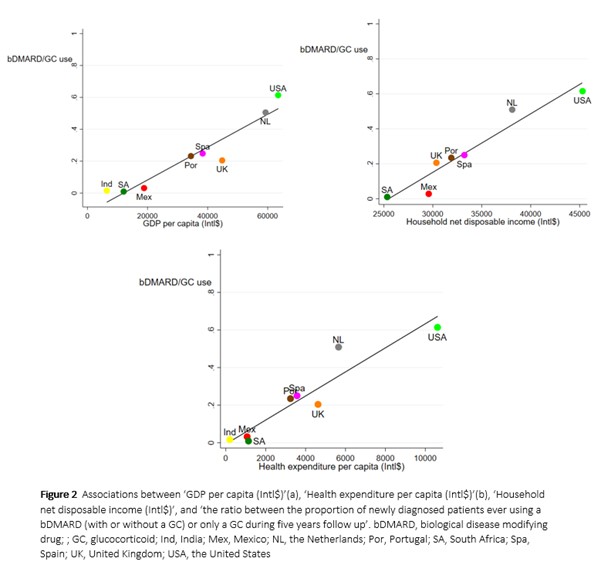
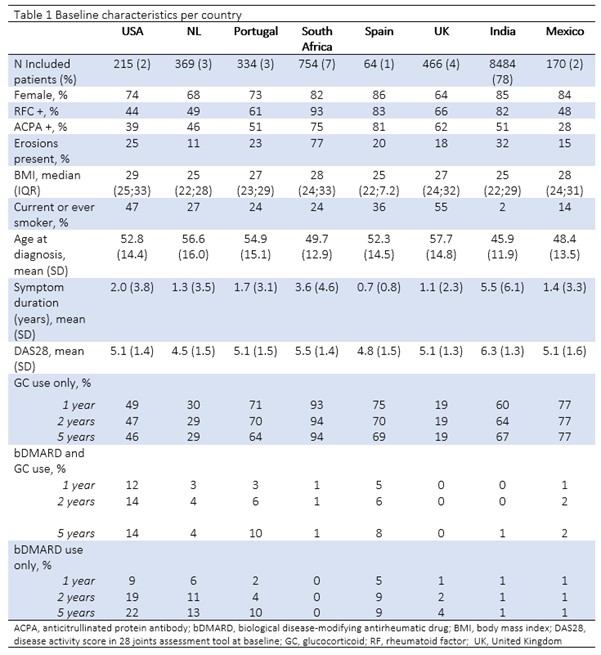
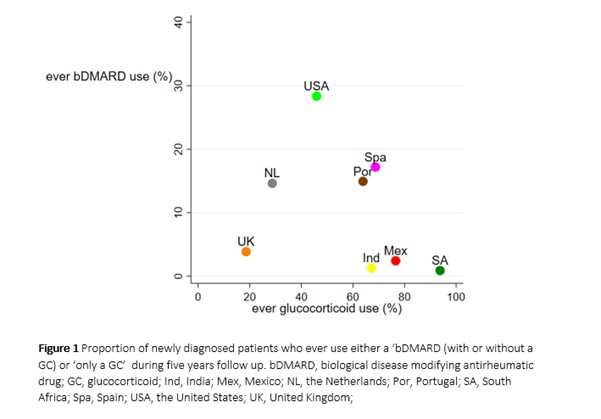
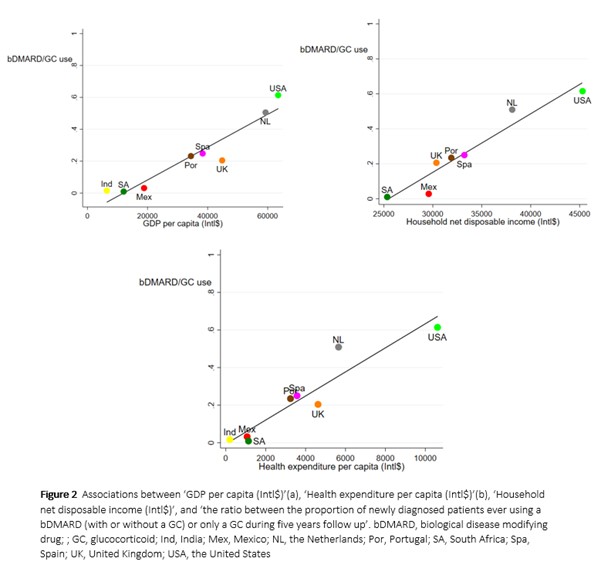
Results: Data from 10,856 patients covering eight different countries showed varying baseline characteristics (table 1) and proportions of bDMARD use. The number of included patients ranged from 64 (Spain) to 8484 (India). The percentage of females and patients with ACPA positive antibodies ranged from 64% (GB) to 86% (Spain) and from 28% (Mexico) to 81% (Spain), respectively. Mean baseline disease activity score (DAS28) varied between 4.8 (Spain) and 6.3 (India). The percentage of patients who used a bDMARD during five years follow up, ranged from 1% (South Africa and India) to 28% (United States, state of Massachusetts) and who used a GC at some time (with no concomitant bDMARD use) during five years follow up, ranged from 19% (Great Britain) to 94% (South Africa) (figure 1). Higher country-level wealth measured in GDP per capita, health expenditure per capita and household net disposable income were related to a higher bDMARD/GC ratio. For every 10,000 IntI$ increase in GDP per capita, household net disposable income and health expenditure per capita, the bDMARD/GC ratio (range 0 to 1) was observed to increase by a value of β 0.1 (95% CI 0.07;0.2, p< 0.001), β 0.3 (95% CI 0.2;0.5, p< 0.05) and β 0.6 (95% CI 0.4;0.9, p< 0.001), respectively (figure 2).
Conclusion: In this analysis based on a worldwide cohort capturing eight countries, we show that the bDMARD/GC ratio indeed differs across countries. These differences are significantly related to general country-level indicators of level of wealth, a higher proportion of patients using bDMARDs and/or a smaller proportion of patients using GCs.
Disclosures: I. Nevins, None; C. Allaart, None; D. Vega Morales, None; L. Winchow, None; A. Chopra, None; A. Rodrigues, None; T. Huizinga, None; M. Boers, Novartis; S. Bergstra, None.
Background/Purpose: Previous studies have demonstrated differing bDMARD prescription rates between countries, which seems to be amongst others related to a country's socioeconomic status. In contrast, the costs of glucocorticoids (GC) are significantly lower and it may be hypothesized that when less bDMARDs are used, GC use increases. Therefore, the objective of this study was to investigate globally the ratio between bDMARD and GC use, and to assess whether this relates to a country's socioeconomic status (SES).
Methods: Data on bDMARD and GC use were extracted from the METEOR database: an international database capturing daily clinical practice data from patients with a clinical diagnosis of rheumatoid arthritis (RA). Countries were included that had contributed at least 60 newly diagnosed patients, as of 1-1-2007. The ratio between the proportion of patients who had ever used a bDMARD and the proportion of patients who had ever used a GC (with no concomitant bDMARD use) during a total follow up duration of five years (bDMARD/GC ratio) was calculated per country. Univariable linear regression was used to analyze the bDMARD/GC ratios according to publicly available country-level indicators of SES (measured in GDP per capita, household net disposable income and health expenditure per capita, expressed in International dollar (IntI$) to account for the differences in purchasing power)
Results: Data from 10,856 patients covering eight different countries showed varying baseline characteristics (table 1) and proportions of bDMARD use. The number of included patients ranged from 64 (Spain) to 8484 (India). The percentage of females and patients with ACPA positive antibodies ranged from 64% (GB) to 86% (Spain) and from 28% (Mexico) to 81% (Spain), respectively. Mean baseline disease activity score (DAS28) varied between 4.8 (Spain) and 6.3 (India). The percentage of patients who used a bDMARD during five years follow up, ranged from 1% (South Africa and India) to 28% (United States, state of Massachusetts) and who used a GC at some time (with no concomitant bDMARD use) during five years follow up, ranged from 19% (Great Britain) to 94% (South Africa) (figure 1). Higher country-level wealth measured in GDP per capita, health expenditure per capita and household net disposable income were related to a higher bDMARD/GC ratio. For every 10,000 IntI$ increase in GDP per capita, household net disposable income and health expenditure per capita, the bDMARD/GC ratio (range 0 to 1) was observed to increase by a value of β 0.1 (95% CI 0.07;0.2, p< 0.001), β 0.3 (95% CI 0.2;0.5, p< 0.05) and β 0.6 (95% CI 0.4;0.9, p< 0.001), respectively (figure 2).
Conclusion: In this analysis based on a worldwide cohort capturing eight countries, we show that the bDMARD/GC ratio indeed differs across countries. These differences are significantly related to general country-level indicators of level of wealth, a higher proportion of patients using bDMARDs and/or a smaller proportion of patients using GCs.
Disclosures: I. Nevins, None; C. Allaart, None; D. Vega Morales, None; L. Winchow, None; A. Chopra, None; A. Rodrigues, None; T. Huizinga, None; M. Boers, Novartis; S. Bergstra, None.

