Back
Poster Session A
Systemic lupus erythematosus (SLE)
Session: (0317–0342) SLE – Diagnosis, Manifestations, and Outcomes Poster I: Diagnosis
0339: Corneal Confocal Microscopy: A Potential Ophthalmic Imaging Biomarker of Neurodegeneration for Systemic Lupus Erythematosus
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- MG
Miral Gharib, MD
hamad medical corporation
Doha, Qatar
Abstract Poster Presenter(s)
Miral H.Gharib1, Georgios Baloglu2, Soha Osman1, Rayaz A.Malik3 and Samar Al emadi1, 1Hamad Medical Corporation, Doha, Qatar, 2Weill Cornell Medicine-Qatar, Research division, Qatar foundation, Doha, Qatar, 3Weill Cornell Medicine-Qatar, Research division, Qatar foundation, institute of cardiovascular sciences, Cardiac center, university of Manchester and NIHR clinical research facility, Doha, Qatar
Background/Purpose: Systemic lupus erythematosus (SLE) is a chronic multi-system autoimmune disease with frequent neuropsychiatric symptoms occurring in 80% to 90% of patients with SLE divided into central and peripheral nervous system manifestations included in the neuropsychiatric systemic lupus erythematosus (NPSLE) criteria, and are associated with poor outcomes. Small fiber neuropathy (SFN) can cause intolerable pain and is an underdiagnosed neurological manifestation of SLE due to a normal or near-normal neurological examination and electrophysiological testing. Indeed, it is not included in the NPSLE criteria, The purpose of this study was to evaluate the utility of corneal confocal microscopy (CCM) in identifying small nerve fiber damage in patients with systemic lupus erythematosus.
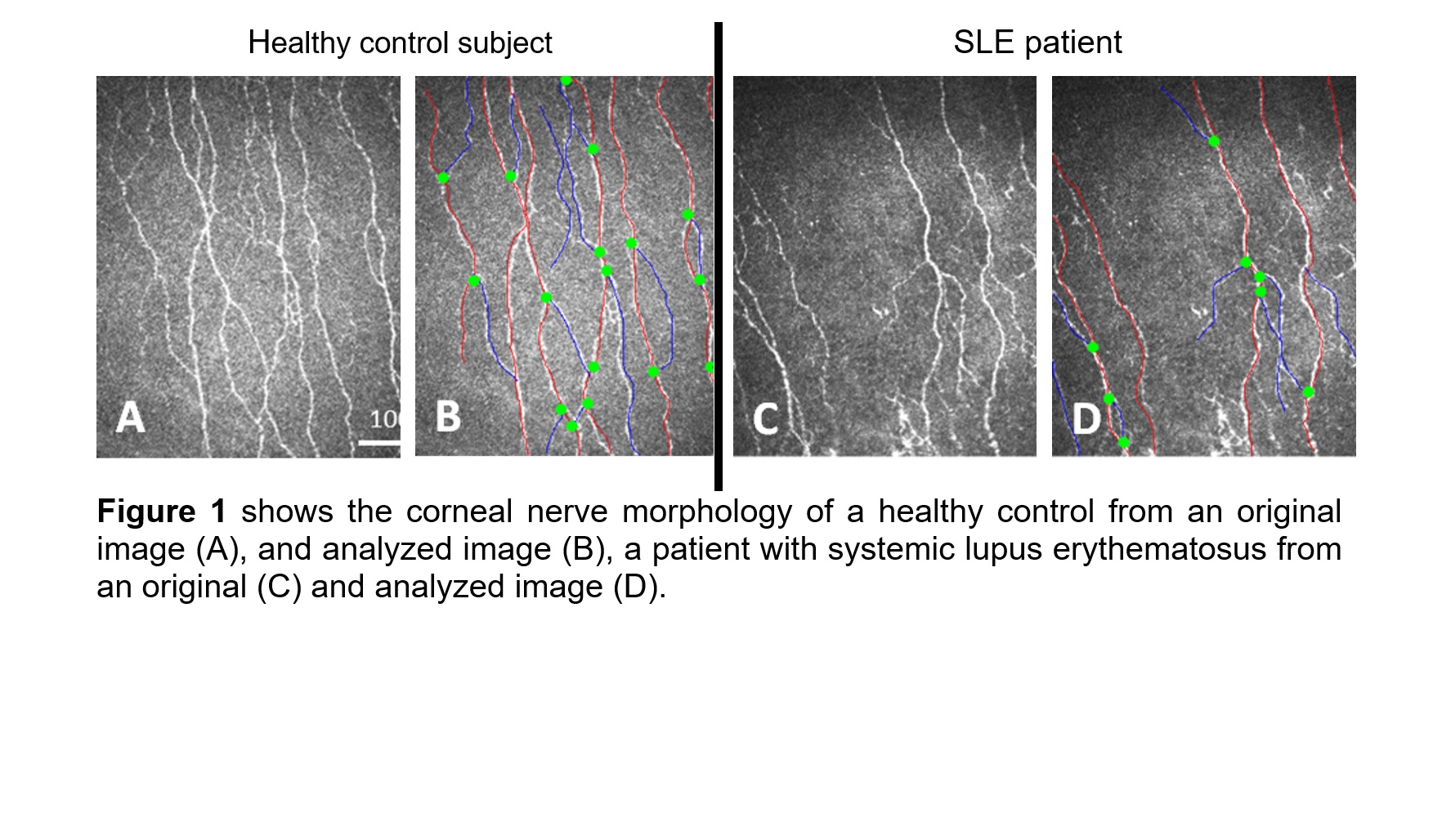
Methods: This is a pilot cross-sectional study conducted at Rheumatology clinic in Hamad Medical Hospital, Qatar. SLE was diagnosed in adult patients (≥18years old) who satisfy at least four of the American College of Rheumatology (ACR) criteria for the Classification of SLE. Exclusion criteria included causes of peripheral neuropathy: diabetes, vitamin B12, and hypothyroidism, other exclusion criteria included corneal trauma, dystrophy, surgery, severe dry eyes or allergy to local anesthetics, while the exclusion criteria for controls included SLE. Subjects underwent clinical examinations, DN4 questionnaire, CCM, sudomotor function assessment and vibration perception threshold (VPT). The CCM outcome measures were corneal nerve fiber density (CNFD, number of fibers/mm2), length (CNFL, mm/mm2), and branch density (CNBD, number of branches/mm2). The study was approved by the Hamad Medical Corporation IRB (# IRGC-07-NI-20-337) and Weill Cornell Medicine in Qatar IRB (# 21-00024) and written informed consent was obtained from all subjects complying to the Helsinki Declaration.
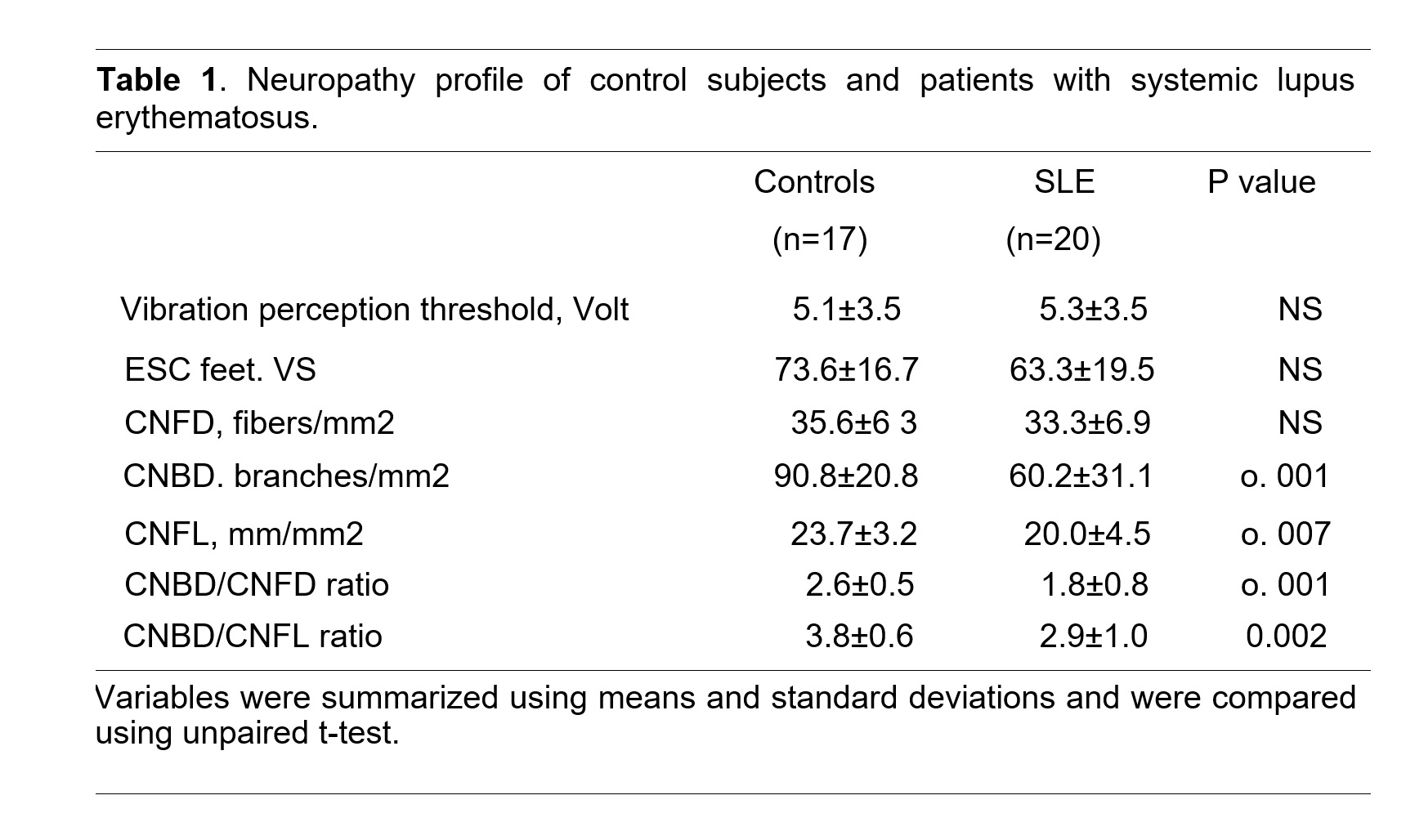
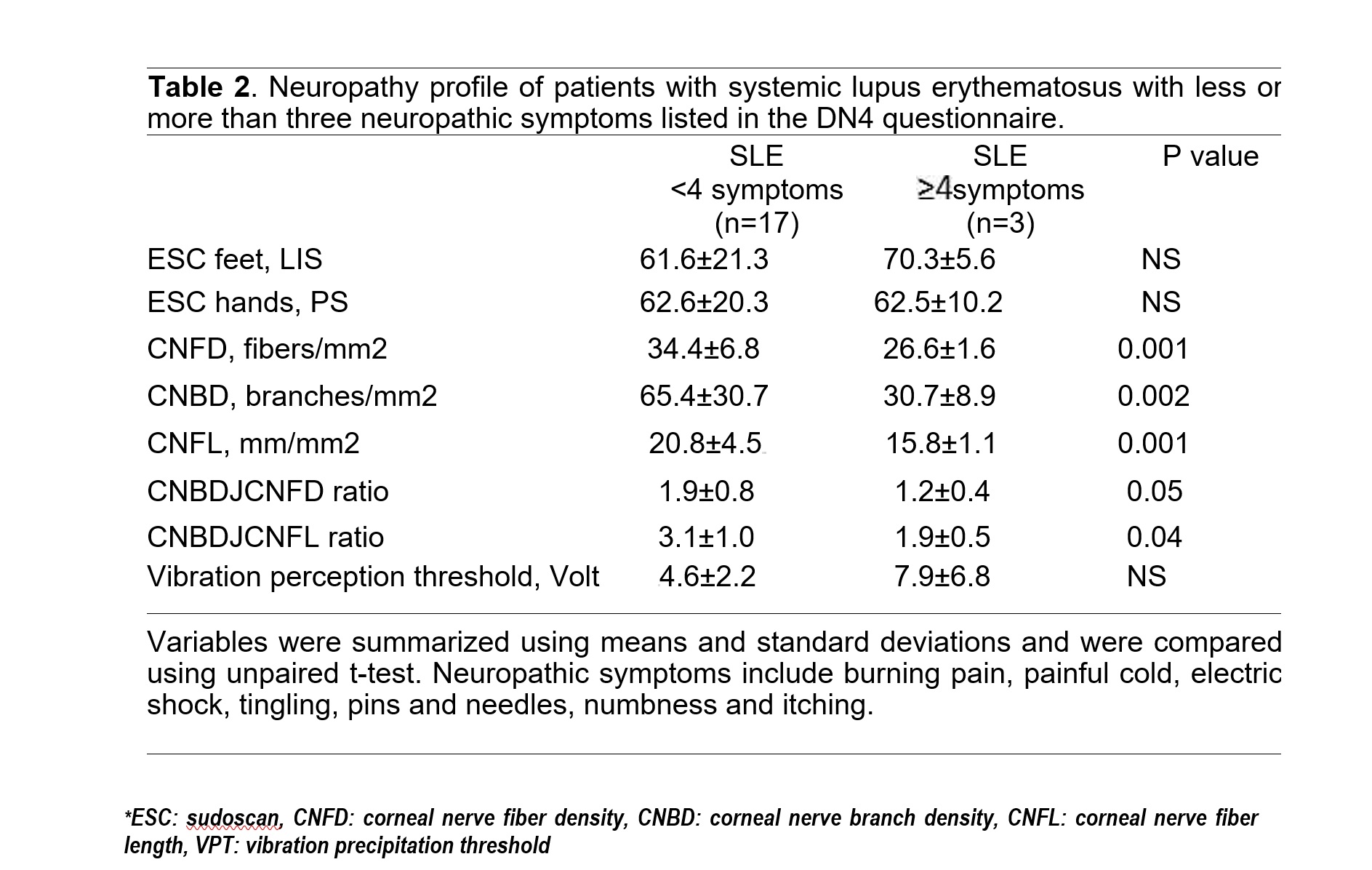
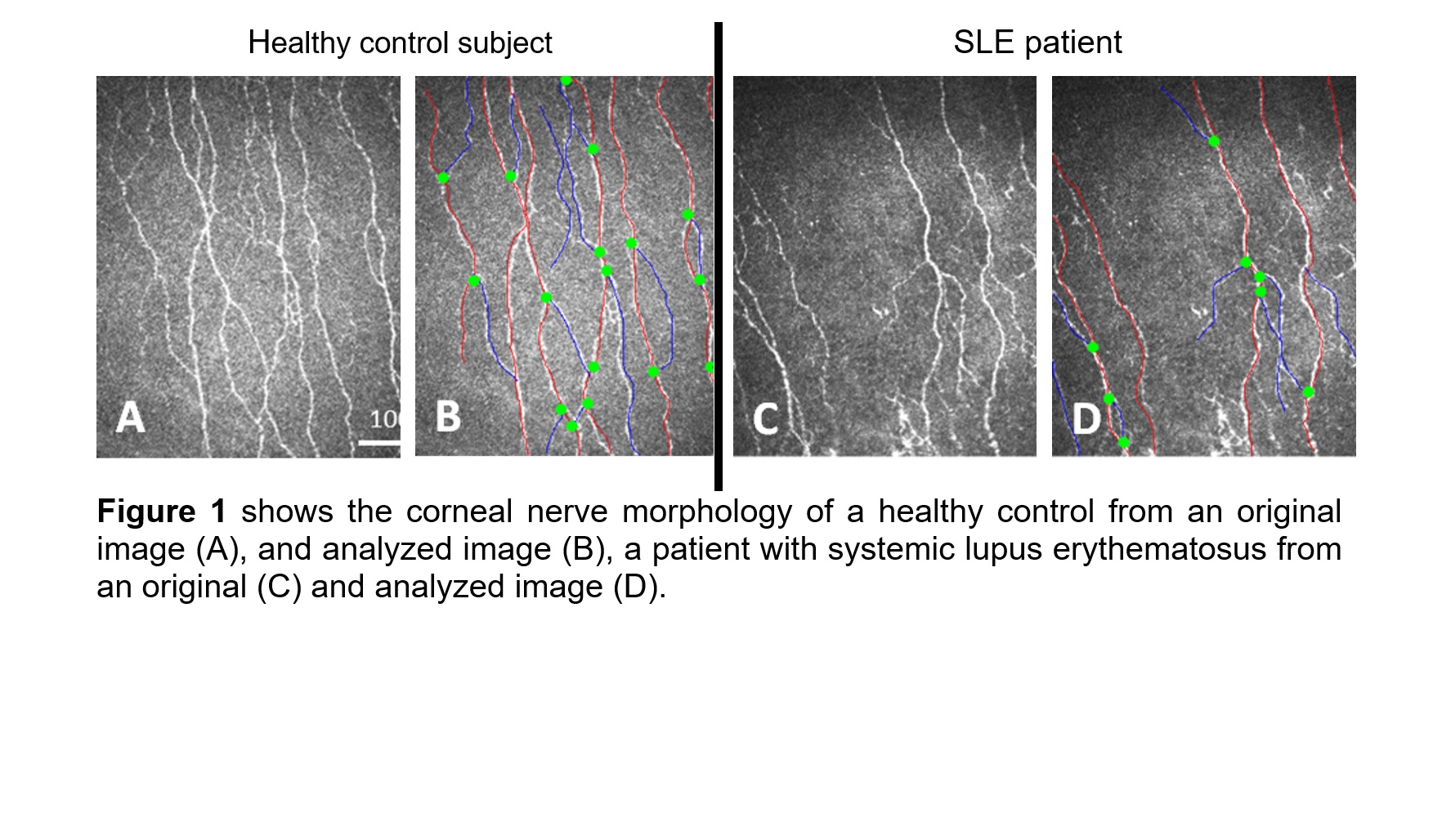
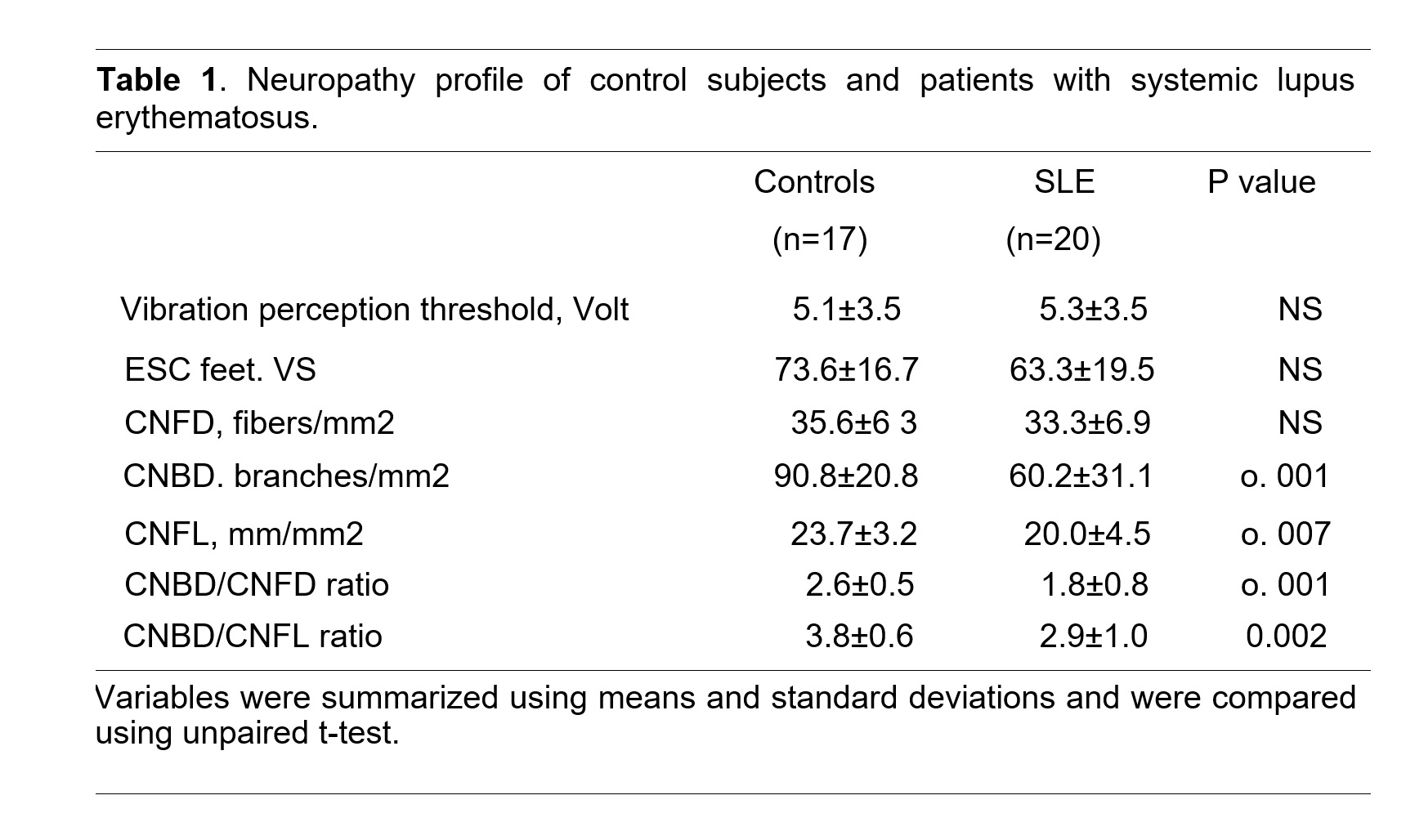
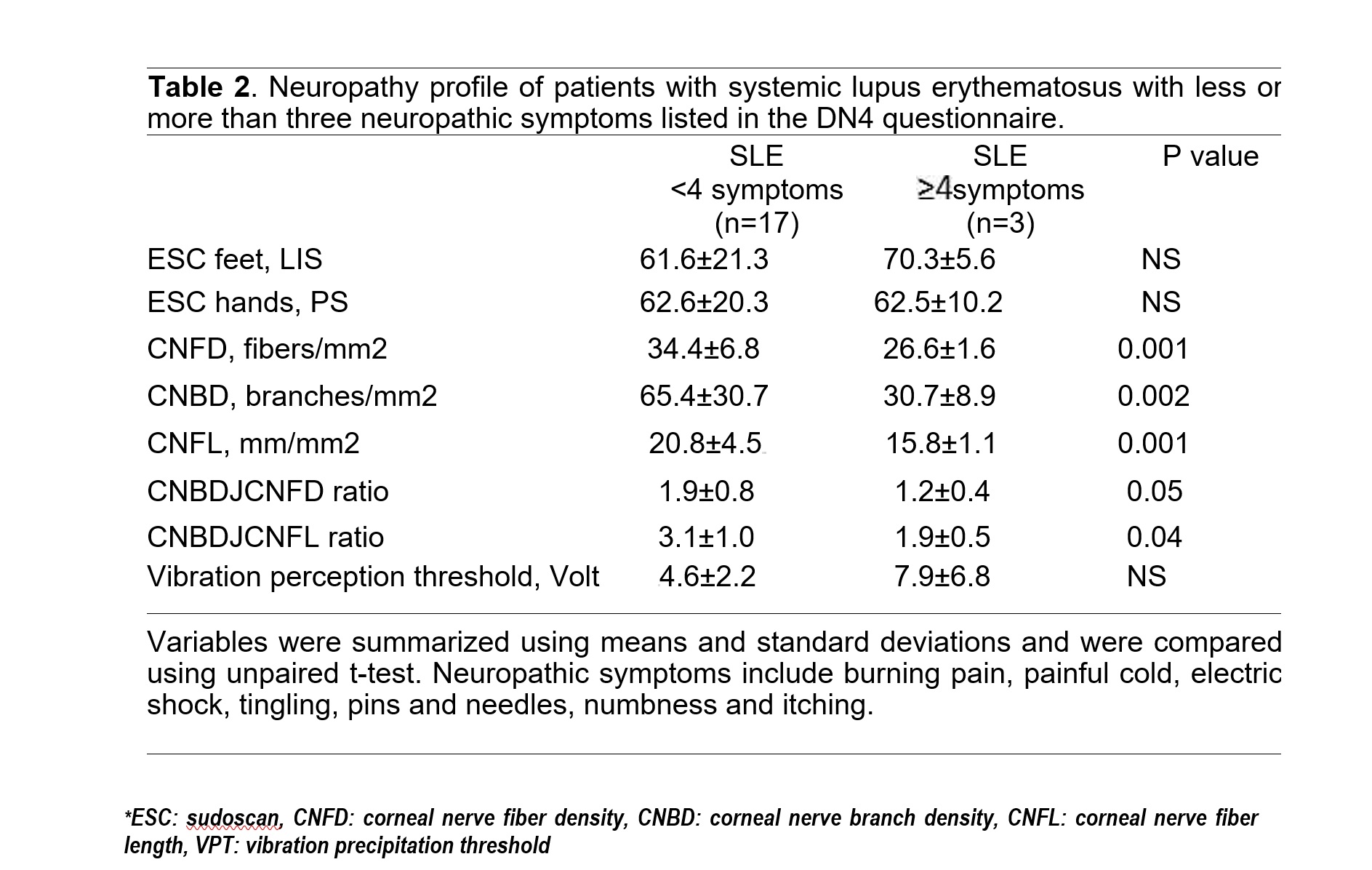
Results: Of 37 subjects recruited for the study 20 were with SLE with (n=3) and without neuropathic pain (n=17), and 17 were healthy controls. Compared to healthy controls, subjects with SLE had significantly lower CNBD (60.2+31.1 vs 90.8+20.8) branches/mm2, P= 0.001), CNFL (20.0±4.5 vs 23.7±3.2 mm/mm2, P=0.007), CNBD/CNFD ratio (1.8±0.8 vs 2.6±0.5, P=0.001), and CNBD/CNFL ratio (2.9±1.0 vs 3.8±0.6, P=0.002), but no significant differences in CNFD, VPT, and sudomotor function (Table 1). Our underpowered data suggest that patient with neuropathic pain have significantly lower CNFD (26.6±1.6 vs 34.4±6.8 fibers/mm2, P= 0.001), CNBD (30.7±8.9 vs 65.4±30.7 branches/mm2, P= 0.002), CNFL (15.8±1.1 vs 20.8±4.5 mm/mm2, P= 0.001), CNBD/CNFD ratio (1.2±0.4 vs 1.9±0.8, P=0.05), and CNBD/CNFL ratio (1.9±0.5 vs 3.1±1.0, P= 0.04), but no significant difference in VPT and sudomotor function (Table 2).
Conclusion: Our study shows that Corneal confocal microscopy (CCM) a non-invasive modality detects small nerve fiber damage in patients with SLE, particularly in those with neuropathic pain encouraging larger studies to determine the utility of CCM as a surrogate marker of neurodegeneration for SLE.
Disclosures: M. H.Gharib, None; G. Baloglu, None; S. Osman, None; R. A.Malik, None; S. Al emadi, None.
Background/Purpose: Systemic lupus erythematosus (SLE) is a chronic multi-system autoimmune disease with frequent neuropsychiatric symptoms occurring in 80% to 90% of patients with SLE divided into central and peripheral nervous system manifestations included in the neuropsychiatric systemic lupus erythematosus (NPSLE) criteria, and are associated with poor outcomes. Small fiber neuropathy (SFN) can cause intolerable pain and is an underdiagnosed neurological manifestation of SLE due to a normal or near-normal neurological examination and electrophysiological testing. Indeed, it is not included in the NPSLE criteria, The purpose of this study was to evaluate the utility of corneal confocal microscopy (CCM) in identifying small nerve fiber damage in patients with systemic lupus erythematosus.
Methods: This is a pilot cross-sectional study conducted at Rheumatology clinic in Hamad Medical Hospital, Qatar. SLE was diagnosed in adult patients (≥18years old) who satisfy at least four of the American College of Rheumatology (ACR) criteria for the Classification of SLE. Exclusion criteria included causes of peripheral neuropathy: diabetes, vitamin B12, and hypothyroidism, other exclusion criteria included corneal trauma, dystrophy, surgery, severe dry eyes or allergy to local anesthetics, while the exclusion criteria for controls included SLE. Subjects underwent clinical examinations, DN4 questionnaire, CCM, sudomotor function assessment and vibration perception threshold (VPT). The CCM outcome measures were corneal nerve fiber density (CNFD, number of fibers/mm2), length (CNFL, mm/mm2), and branch density (CNBD, number of branches/mm2). The study was approved by the Hamad Medical Corporation IRB (# IRGC-07-NI-20-337) and Weill Cornell Medicine in Qatar IRB (# 21-00024) and written informed consent was obtained from all subjects complying to the Helsinki Declaration.
Results: Of 37 subjects recruited for the study 20 were with SLE with (n=3) and without neuropathic pain (n=17), and 17 were healthy controls. Compared to healthy controls, subjects with SLE had significantly lower CNBD (60.2+31.1 vs 90.8+20.8) branches/mm2, P= 0.001), CNFL (20.0±4.5 vs 23.7±3.2 mm/mm2, P=0.007), CNBD/CNFD ratio (1.8±0.8 vs 2.6±0.5, P=0.001), and CNBD/CNFL ratio (2.9±1.0 vs 3.8±0.6, P=0.002), but no significant differences in CNFD, VPT, and sudomotor function (Table 1). Our underpowered data suggest that patient with neuropathic pain have significantly lower CNFD (26.6±1.6 vs 34.4±6.8 fibers/mm2, P= 0.001), CNBD (30.7±8.9 vs 65.4±30.7 branches/mm2, P= 0.002), CNFL (15.8±1.1 vs 20.8±4.5 mm/mm2, P= 0.001), CNBD/CNFD ratio (1.2±0.4 vs 1.9±0.8, P=0.05), and CNBD/CNFL ratio (1.9±0.5 vs 3.1±1.0, P= 0.04), but no significant difference in VPT and sudomotor function (Table 2).
Conclusion: Our study shows that Corneal confocal microscopy (CCM) a non-invasive modality detects small nerve fiber damage in patients with SLE, particularly in those with neuropathic pain encouraging larger studies to determine the utility of CCM as a surrogate marker of neurodegeneration for SLE.
Disclosures: M. H.Gharib, None; G. Baloglu, None; S. Osman, None; R. A.Malik, None; S. Al emadi, None.

