Back
Poster Session C
Vasculitis
Session: (1543–1578) Vasculitis – Non-ANCA-Associated and Related Disorders Poster II
1546: Treatment of Polymyalgia Rheumatica by Rheumatology Providers: Results from the ACR Rheumatology Informatics System for Effectiveness Registry
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall

Sebastian Sattui, MD, MS
University of Pittsburgh
Pittsburgh, PA, United States
Abstract Poster Presenter(s)
Sebastian Sattui1, Zihan Wan2, Fenglong Xie2, Cassie Clinton2, Robyn Domsic1 and Jeffrey Curtis3, 1University of Pittsburgh, Pittsburgh, PA, 2University of Alabama at Birmingham, Birmingham, AL, 3University of Alabama at Birmingham, Hoover, AL
Background/Purpose: Polymyalgia rheumatica (PMR) is one of the most common systemic rheumatic diseases in older adults. Glucocorticoids (GC) remain the main treatment, and although recommendations suggest discontinuing GC after 1-2 years, prolonged use occurs in a significant proportion of patients. Patients with PMR treated by rheumatology providers are presumably more refractory, and with emerging evidence of recent phase 2/3 studies showing efficacy of steroid-sparring agents, a better understanding of patients with PMR under rheumatologic care and associated treatment patterns are needed. The objective of this study was to describe a national cohort of PMR patients receiving care from rheumatology providers and characterize demographics, disease features, and treatment practices, including the use of steroid-sparing agents.
Methods: Using data from the ACR Rheumatology Informatics System for Effectiveness (RISE) registry from 2016-2020, patients with PMR were identified; requiring age ≥ 50 years and ≥ 2 outpatient diagnostic codes (ICD-9-CM 725/ICD-10 M35.3) separated ≥ 4 weeks apart. Exclusion criteria were other rheumatologic diagnoses including giant cell arteritis and seropositive RA (but not seronegative RA, given potential for clinical overlap). The index date was time of first PMR diagnosis code. Sociodemographic and comorbidity data (using ICD9/ICD10 codes) was collected at the index date. Cumulative comorbidity was measured using the Charlson-Deyo Comorbidity index (CCI). Use of GC and various immunomodulatory antirheumatic medications used as steroid-sparing agents during the first 24 months following the index date was characterized. A similar approach was taken to identifying patients new to rheumatology practices, based on new patient Current Procedural Terminology codes, many of which may have had new onset PMR (i.e., an inception cohort).
Results: A total of 23,125 patients with PMR were included. Patients were predominantly female (61.4%), white (76.6%), with a mean age of 73.5 (SD 9.1) years. The most frequent comorbidities were osteoporosis (17.3%), malignancy (13.2%), and hypertension (12.5%), with the majority of patients having a CCI between 0-1 (88.5%). Prior to the start of follow-up inclusion, methotrexate (8.7%) and hydroxychloroquine (6.4%) were the most frequently used anti-rheumatic medications. At 12-24 months follow-up, most patients remained on GC (61.9%). In the subgroup of 13,896 patients new to rheumatology practices, 90.8% were on GC prior to index date, while only a minority (12.5%) were on an anti-rheumatic medication. At 12-24 months, most patients with continued follow-up remained on GC (65.1%). Although there was an increase in use through follow-up, use of anti-rheumatic medications occurred only in a minority (37.7%) of patients.
Conclusion: We report data on the largest US-based study of PMR patients under rheumatology care using electronic health records data. Use of steroid-sparring agents was low during the first 24 months of follow-up, and the majority of patient remained on GC. Future analyses will focus on describing treatment patterns during follow-up, and identification of factors associated with use steroid-sparring agents for the treatment of PMR.
.jpg) Table 1. Characteristics of patients with Polymyalgia Rheumatica in the RISE registry
Table 1. Characteristics of patients with Polymyalgia Rheumatica in the RISE registry
.jpg) Table 2. Anti-rheumatic Medications used for Treatment of Polymyalgia Rheumatica During at 12-24 monts of Follow-up
Table 2. Anti-rheumatic Medications used for Treatment of Polymyalgia Rheumatica During at 12-24 monts of Follow-up
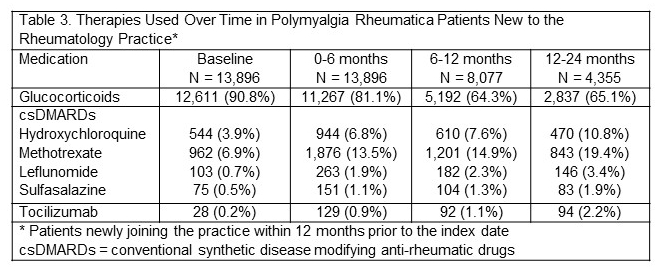 Table 3. Therapies Used Over Time in Polymyalgia Rheumatica Patients New to the Rheumatology Practice
Table 3. Therapies Used Over Time in Polymyalgia Rheumatica Patients New to the Rheumatology Practice
Disclosures: S. Sattui, AstraZeneca; Z. Wan, None; F. Xie, Bendcare; C. Clinton, None; R. Domsic, None; J. Curtis, AbbVie/Abbott, Amgen, ArthritisPower, Aqtual, Bendcare, Bristol-Myers Squibb(BMS), CorEvitas, FASTER, GlaxoSmithKlein(GSK), IlluminationHealth, Janssen, Labcorp, Eli Lilly, Myriad, Novartis, Pfizer, Sanofi, Scipher, Setpoint, UCB, United Rheumatology.
Background/Purpose: Polymyalgia rheumatica (PMR) is one of the most common systemic rheumatic diseases in older adults. Glucocorticoids (GC) remain the main treatment, and although recommendations suggest discontinuing GC after 1-2 years, prolonged use occurs in a significant proportion of patients. Patients with PMR treated by rheumatology providers are presumably more refractory, and with emerging evidence of recent phase 2/3 studies showing efficacy of steroid-sparring agents, a better understanding of patients with PMR under rheumatologic care and associated treatment patterns are needed. The objective of this study was to describe a national cohort of PMR patients receiving care from rheumatology providers and characterize demographics, disease features, and treatment practices, including the use of steroid-sparing agents.
Methods: Using data from the ACR Rheumatology Informatics System for Effectiveness (RISE) registry from 2016-2020, patients with PMR were identified; requiring age ≥ 50 years and ≥ 2 outpatient diagnostic codes (ICD-9-CM 725/ICD-10 M35.3) separated ≥ 4 weeks apart. Exclusion criteria were other rheumatologic diagnoses including giant cell arteritis and seropositive RA (but not seronegative RA, given potential for clinical overlap). The index date was time of first PMR diagnosis code. Sociodemographic and comorbidity data (using ICD9/ICD10 codes) was collected at the index date. Cumulative comorbidity was measured using the Charlson-Deyo Comorbidity index (CCI). Use of GC and various immunomodulatory antirheumatic medications used as steroid-sparing agents during the first 24 months following the index date was characterized. A similar approach was taken to identifying patients new to rheumatology practices, based on new patient Current Procedural Terminology codes, many of which may have had new onset PMR (i.e., an inception cohort).
Results: A total of 23,125 patients with PMR were included. Patients were predominantly female (61.4%), white (76.6%), with a mean age of 73.5 (SD 9.1) years. The most frequent comorbidities were osteoporosis (17.3%), malignancy (13.2%), and hypertension (12.5%), with the majority of patients having a CCI between 0-1 (88.5%). Prior to the start of follow-up inclusion, methotrexate (8.7%) and hydroxychloroquine (6.4%) were the most frequently used anti-rheumatic medications. At 12-24 months follow-up, most patients remained on GC (61.9%). In the subgroup of 13,896 patients new to rheumatology practices, 90.8% were on GC prior to index date, while only a minority (12.5%) were on an anti-rheumatic medication. At 12-24 months, most patients with continued follow-up remained on GC (65.1%). Although there was an increase in use through follow-up, use of anti-rheumatic medications occurred only in a minority (37.7%) of patients.
Conclusion: We report data on the largest US-based study of PMR patients under rheumatology care using electronic health records data. Use of steroid-sparring agents was low during the first 24 months of follow-up, and the majority of patient remained on GC. Future analyses will focus on describing treatment patterns during follow-up, and identification of factors associated with use steroid-sparring agents for the treatment of PMR.
.jpg) Table 1. Characteristics of patients with Polymyalgia Rheumatica in the RISE registry
Table 1. Characteristics of patients with Polymyalgia Rheumatica in the RISE registry.jpg) Table 2. Anti-rheumatic Medications used for Treatment of Polymyalgia Rheumatica During at 12-24 monts of Follow-up
Table 2. Anti-rheumatic Medications used for Treatment of Polymyalgia Rheumatica During at 12-24 monts of Follow-up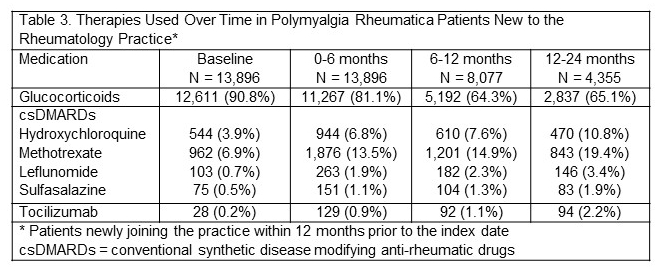 Table 3. Therapies Used Over Time in Polymyalgia Rheumatica Patients New to the Rheumatology Practice
Table 3. Therapies Used Over Time in Polymyalgia Rheumatica Patients New to the Rheumatology PracticeDisclosures: S. Sattui, AstraZeneca; Z. Wan, None; F. Xie, Bendcare; C. Clinton, None; R. Domsic, None; J. Curtis, AbbVie/Abbott, Amgen, ArthritisPower, Aqtual, Bendcare, Bristol-Myers Squibb(BMS), CorEvitas, FASTER, GlaxoSmithKlein(GSK), IlluminationHealth, Janssen, Labcorp, Eli Lilly, Myriad, Novartis, Pfizer, Sanofi, Scipher, Setpoint, UCB, United Rheumatology.

