Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1186–1214) Epidemiology and Public Health Poster II
1213: Trends of Opioid Prescriptions and Impact of the COVID-19 Pandemic Among Patients with Musculoskeletal Diseases Between 2006-2021
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JH
Joyce (Yun-Ting) Huang, PhD
Institution University of Manchester
Manchester, United Kingdom
Abstract Poster Presenter(s)
Joyce (Yun-Ting) Huang1, David Jenkins2, Belay Birlie Yimer1, Jose Benitez-Aurioles2, Niels Peek2, Mark Lunt1, Will Dixon3 and Meghna Jani1, 1Centre for Epidemiology Versus Arthritis, The University of Manchester, Manchester, United Kingdom, 2Division of Informatics, The University of Manchester, Manchester, United Kingdom, 3The University of Manchester, Manchester, United Kingdom
Background/Purpose: Opioid prescribing has contributed to a North American epidemic with increasing trends in several European countries. Rheumatic and musculoskeletal diseases (RMDs) are one of the most common indications for opioids despite there being little evidence especially in the long-term use setting. The COVID-19 pandemic affected access to orthopaedic interventions & health services which may have impacted opioid prescribing. The aim was to investigate national UK opioid prescribing trends by studying the patterns of opioid prescribing in new and prevalent users with the following six RMDs: rheumatoid arthritis (RA), psoriatic arthritis (PsA), axial spondyloarthritis (AxSpA), systemic lupus erythematosus (SLE), osteoarthritis (OA) and fibromyalgia.
Methods: Patients aged 18 years and older with a diagnosis of RA, PsA, AxSpA, SLE and OA without cancer in the Clinical Practice Research Datalink (CPRD) were included between 01/01/2006 and 31/08/2021. CPRD is a database of anonymised UK primary care electronic health records representative of the national population. New and prevalent users were analysed separately. Age- and gender-standardised rates were obtained using direct standardization, and trends for the rates were tested using negative binomial regression. Significant change points were identified by assessing the points where the derivative (i.e. rate of change) of the trends for the rates crossed zero. Negative binomial regression models were fitted on the monthly measures of new and prevalent users, opioid prescriptions, and MME/day for the period Jan 2015 to Feb 2020, and used to predict the expected values between Mar 2020 and Aug 2021. The proportion of new opioid users who transitioned to long-term opioid use was calculated. Long-term opioid use was defined as ≥ 3 opioid prescriptions within a 90-day period or ≥ 1 opioid prescription lasting at least 90 days in the first year of follow up.
Results: This study included 36,932 RA, 12,649 PsA, 6,811 AxSpA, 6,423 SLE, 1,255,999 OA patients, and 66,944 fibromyalgia patients who were both new and prevalent opioid users. RA, PsA and fibromyalgia showed increasing trends of new users between 2006-2021, but trends appeared to stabilise/decrease from 2018 to 2021: RA (4.5 vs 2.4 new users/10,000 persons); PsA (1.8 vs 1.2 new users/10,000 persons); fibromyalgia (8.4 vs 5.9 new users/10,000 persons). The trends of prevalent opioid users increased for all RMDs over the 15 years, with a 4.5 fold increase in fibromyalgia (Figure). Most significant decreasing change points in the trends of new and prevalent users were detected after 2018. In patients who initiated an opioid for the first time, the proportion of long-term opioid users were: 21% RA, 20% AS, 18% PsA, 15% SLE, 23% fibromyalgia and 13% OA.
Conclusion: RA, PsA and fibromyalgia had an overall increase in new opioid users since 2006. The COVID-19 pandemic did not result in a substantial increase in opioid prescriptions. However nearly 1 in 5 new users of opioids with inflammatory arthritis and 1 in 4 fibromyalgia patients transitioned to long-term opioid use, highlighting the importance of evaluating opioid safety and effective pain interventions for patients with RMDs.
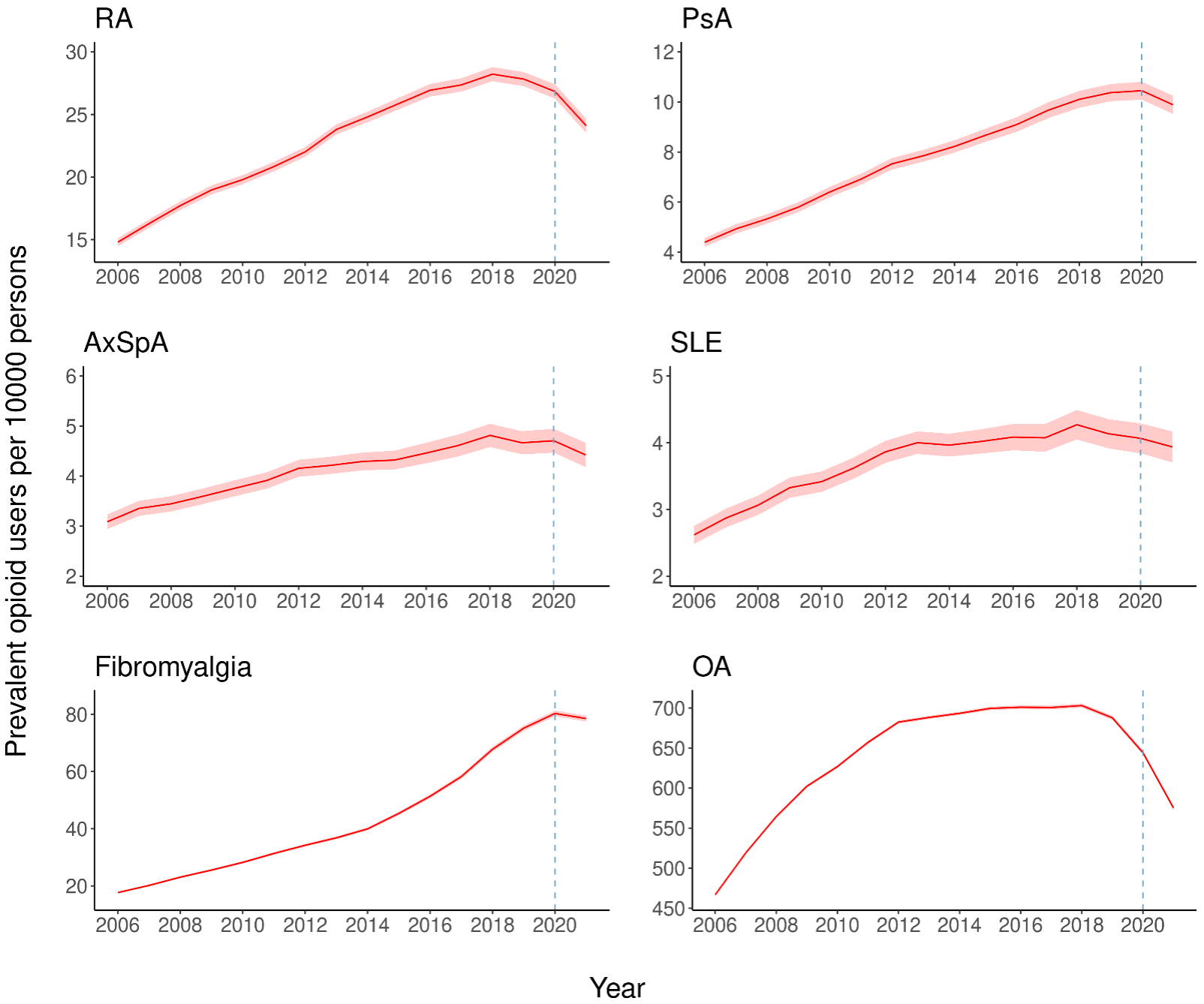 Prevalent opioid users per 10,000 persons
Prevalent opioid users per 10,000 persons
Disclosures: J. Huang, None; D. Jenkins, None; B. Yimer, None; J. Benitez-Aurioles, None; N. Peek, None; M. Lunt, None; W. Dixon, Google; M. Jani, None.
Background/Purpose: Opioid prescribing has contributed to a North American epidemic with increasing trends in several European countries. Rheumatic and musculoskeletal diseases (RMDs) are one of the most common indications for opioids despite there being little evidence especially in the long-term use setting. The COVID-19 pandemic affected access to orthopaedic interventions & health services which may have impacted opioid prescribing. The aim was to investigate national UK opioid prescribing trends by studying the patterns of opioid prescribing in new and prevalent users with the following six RMDs: rheumatoid arthritis (RA), psoriatic arthritis (PsA), axial spondyloarthritis (AxSpA), systemic lupus erythematosus (SLE), osteoarthritis (OA) and fibromyalgia.
Methods: Patients aged 18 years and older with a diagnosis of RA, PsA, AxSpA, SLE and OA without cancer in the Clinical Practice Research Datalink (CPRD) were included between 01/01/2006 and 31/08/2021. CPRD is a database of anonymised UK primary care electronic health records representative of the national population. New and prevalent users were analysed separately. Age- and gender-standardised rates were obtained using direct standardization, and trends for the rates were tested using negative binomial regression. Significant change points were identified by assessing the points where the derivative (i.e. rate of change) of the trends for the rates crossed zero. Negative binomial regression models were fitted on the monthly measures of new and prevalent users, opioid prescriptions, and MME/day for the period Jan 2015 to Feb 2020, and used to predict the expected values between Mar 2020 and Aug 2021. The proportion of new opioid users who transitioned to long-term opioid use was calculated. Long-term opioid use was defined as ≥ 3 opioid prescriptions within a 90-day period or ≥ 1 opioid prescription lasting at least 90 days in the first year of follow up.
Results: This study included 36,932 RA, 12,649 PsA, 6,811 AxSpA, 6,423 SLE, 1,255,999 OA patients, and 66,944 fibromyalgia patients who were both new and prevalent opioid users. RA, PsA and fibromyalgia showed increasing trends of new users between 2006-2021, but trends appeared to stabilise/decrease from 2018 to 2021: RA (4.5 vs 2.4 new users/10,000 persons); PsA (1.8 vs 1.2 new users/10,000 persons); fibromyalgia (8.4 vs 5.9 new users/10,000 persons). The trends of prevalent opioid users increased for all RMDs over the 15 years, with a 4.5 fold increase in fibromyalgia (Figure). Most significant decreasing change points in the trends of new and prevalent users were detected after 2018. In patients who initiated an opioid for the first time, the proportion of long-term opioid users were: 21% RA, 20% AS, 18% PsA, 15% SLE, 23% fibromyalgia and 13% OA.
Conclusion: RA, PsA and fibromyalgia had an overall increase in new opioid users since 2006. The COVID-19 pandemic did not result in a substantial increase in opioid prescriptions. However nearly 1 in 5 new users of opioids with inflammatory arthritis and 1 in 4 fibromyalgia patients transitioned to long-term opioid use, highlighting the importance of evaluating opioid safety and effective pain interventions for patients with RMDs.
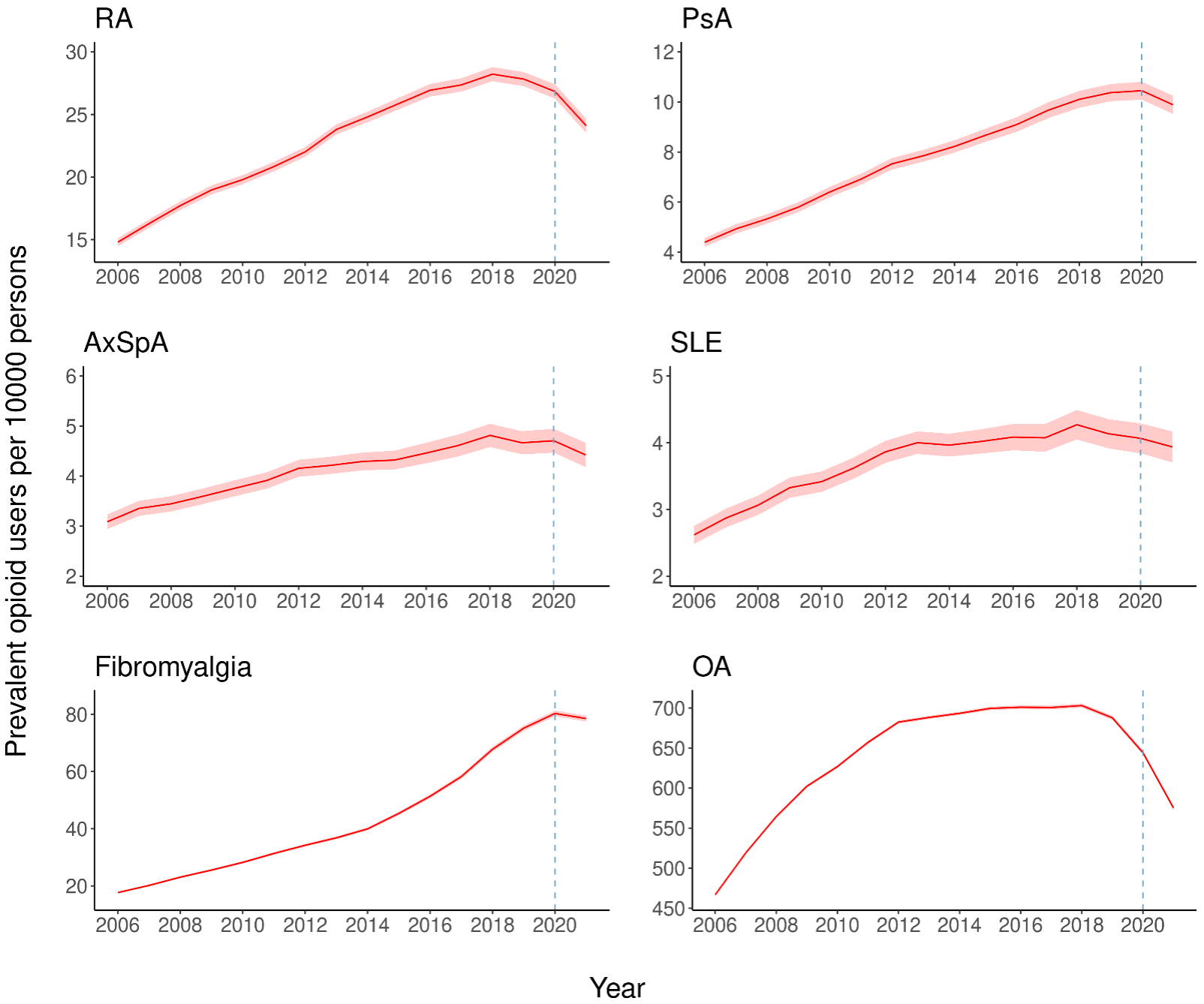 Prevalent opioid users per 10,000 persons
Prevalent opioid users per 10,000 personsDisclosures: J. Huang, None; D. Jenkins, None; B. Yimer, None; J. Benitez-Aurioles, None; N. Peek, None; M. Lunt, None; W. Dixon, Google; M. Jani, None.

