Back
Poster Session C
Vasculitis
Session: (1543–1578) Vasculitis – Non-ANCA-Associated and Related Disorders Poster II
1562: Validation of Behçet's Disease Overall Damage Index (BODI) for Retrospective Studies and a Proposal for Modification
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- YY
Yeliz Yagiz Ozogul, MD
Istanbul University-Cerrahpasa
Istanbul, Turkey
Abstract Poster Presenter(s)
Yeliz Yagiz Ozogul1, Yesim Ozguler2, Didar Ucar3, Ugur Uygunoglu4, Zekayi Kutlubay5, Vedat Hamuryudan6 and gulen Hatemi7, 1Istanbul University-Cerrahpaşa, Cerrahpaşa Medical School, Department of Internal Medicine, Istanbul, Turkey, 2Istanbul University-Cerrahpasa, Cerrahpasa Medical Faculty, Department of Internal Medicine, Division of Rheumatology, New York, NY, 3Istanbul University-Cerrahpaşa, Cerrahpaşa Medical School, Department of Ophthalmology, Istanbul, Turkey, 4Istanbul University-Cerrahpaşa, Cerrahpaşa Medical School, Department of Neurology, Istanbul, Turkey, 5Istanbul University-Cerrahpaşa, Cerrahpaşa Medical School, Department of Dermatology, Istanbul, Turkey, 6Istanbul University-Cerrahpaşa, Cerrahpaşa Medical School, Department of Internal Medicine, Division of Rheumatology, Istanbul, Turkey, 7Istanbul University-Cerrahpaşa, Cerrahpasa Medical Faculty, Department of Internal Medicine, Division of Rheumatology, Istanbul, Turkey
Background/Purpose: Damage accrual in Behçet syndrome (BS) may progress over the years and an index that can be scored using retrospective data may be useful in measuring damage accrual over a long time and comparing different treatment strategies or patient populations. We aimed to assess the construct validity, reproducibility, sensitivity to change and feasibility of Behçet's Disease Overall Damage Index (BODI) for use in retrospective studies, and to identify items that may be missing in BODI.
Methods: BODI was translated into Turkish with the principles of scale adaptation and translated backwards by 2 people. The study included 300 patients with at least 2 visits at 1-year intervals out of 712 consecutive BS patients admitted between 2015-2017. Correlation between BODI score of the same patient that was assessed during a face-to-face visit and that was calculated retrospectively using patient charts was evaluated using intraclass correlation coefficient (ICC). Interobserver and intraobserver correlation, correlation with disease activity and feasibility were also evaluated.
Results: The mean BODI score was 1.56 ± 1.44 SD. There was good correlation between face-to-face and retrospective evaluation (ICC 0.998; [%95CI 0.997-0.999]), good interobserver agreement (ICC 0.96 [95%CI 0.94-0.98]) and intraobserver agreement (ICC 1). No correlation with disease activity was detected (r=-0.01, p=0.5). We observed an increase in BODI score in 113 (37.6%) patients during follow-up. The main reasons for increasing BODI scores were eye, vascular and neurological involvement (Table). Items not captured by BODI were hypertension, lymphedema, liver failure, glaucoma, damage due to venous interventions and lung parenchymal involvement. The mean time to complete the form was 1.5 (1-4) minutes.
Conclusion: The validated Turkish version of BODI is convenient and applicable in terms of construct validity and can be used reliably in retrospective studies. Whether modification of BODI by adding damage items identified in this study would make it an even better scale warrants further studies.
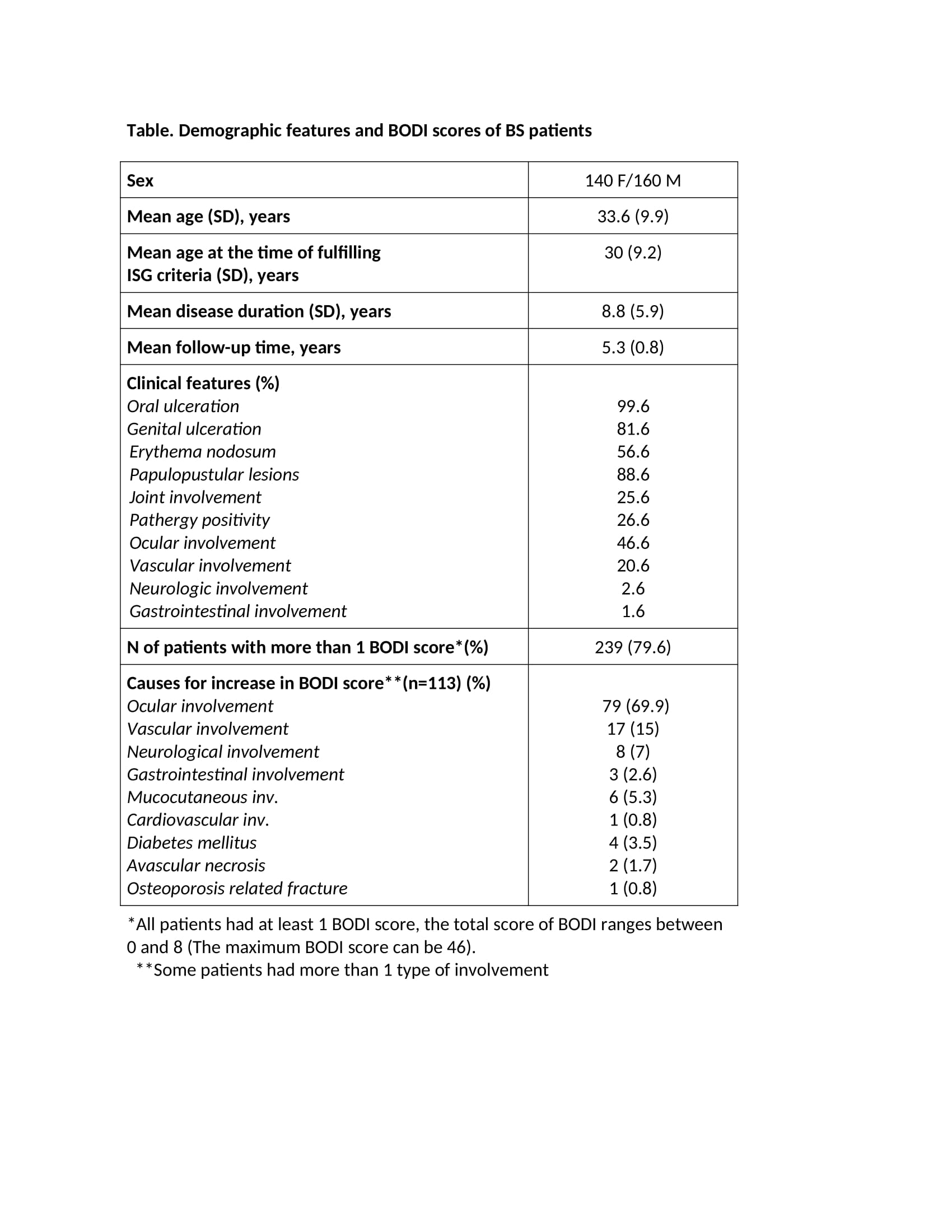 Table. Demographic features and BODI scores of BS patients
Table. Demographic features and BODI scores of BS patients
Disclosures: Y. Yagiz Ozogul, None; Y. Ozguler, UCB, Novartis, Pfizer; D. Ucar, None; U. Uygunoglu, None; Z. Kutlubay, None; V. Hamuryudan, Celgene, AbbVie/Abbott, Novartis, UCB; g. Hatemi, Celgene, UCB, Novartis, AbbVie/Abbott.
Background/Purpose: Damage accrual in Behçet syndrome (BS) may progress over the years and an index that can be scored using retrospective data may be useful in measuring damage accrual over a long time and comparing different treatment strategies or patient populations. We aimed to assess the construct validity, reproducibility, sensitivity to change and feasibility of Behçet's Disease Overall Damage Index (BODI) for use in retrospective studies, and to identify items that may be missing in BODI.
Methods: BODI was translated into Turkish with the principles of scale adaptation and translated backwards by 2 people. The study included 300 patients with at least 2 visits at 1-year intervals out of 712 consecutive BS patients admitted between 2015-2017. Correlation between BODI score of the same patient that was assessed during a face-to-face visit and that was calculated retrospectively using patient charts was evaluated using intraclass correlation coefficient (ICC). Interobserver and intraobserver correlation, correlation with disease activity and feasibility were also evaluated.
Results: The mean BODI score was 1.56 ± 1.44 SD. There was good correlation between face-to-face and retrospective evaluation (ICC 0.998; [%95CI 0.997-0.999]), good interobserver agreement (ICC 0.96 [95%CI 0.94-0.98]) and intraobserver agreement (ICC 1). No correlation with disease activity was detected (r=-0.01, p=0.5). We observed an increase in BODI score in 113 (37.6%) patients during follow-up. The main reasons for increasing BODI scores were eye, vascular and neurological involvement (Table). Items not captured by BODI were hypertension, lymphedema, liver failure, glaucoma, damage due to venous interventions and lung parenchymal involvement. The mean time to complete the form was 1.5 (1-4) minutes.
Conclusion: The validated Turkish version of BODI is convenient and applicable in terms of construct validity and can be used reliably in retrospective studies. Whether modification of BODI by adding damage items identified in this study would make it an even better scale warrants further studies.
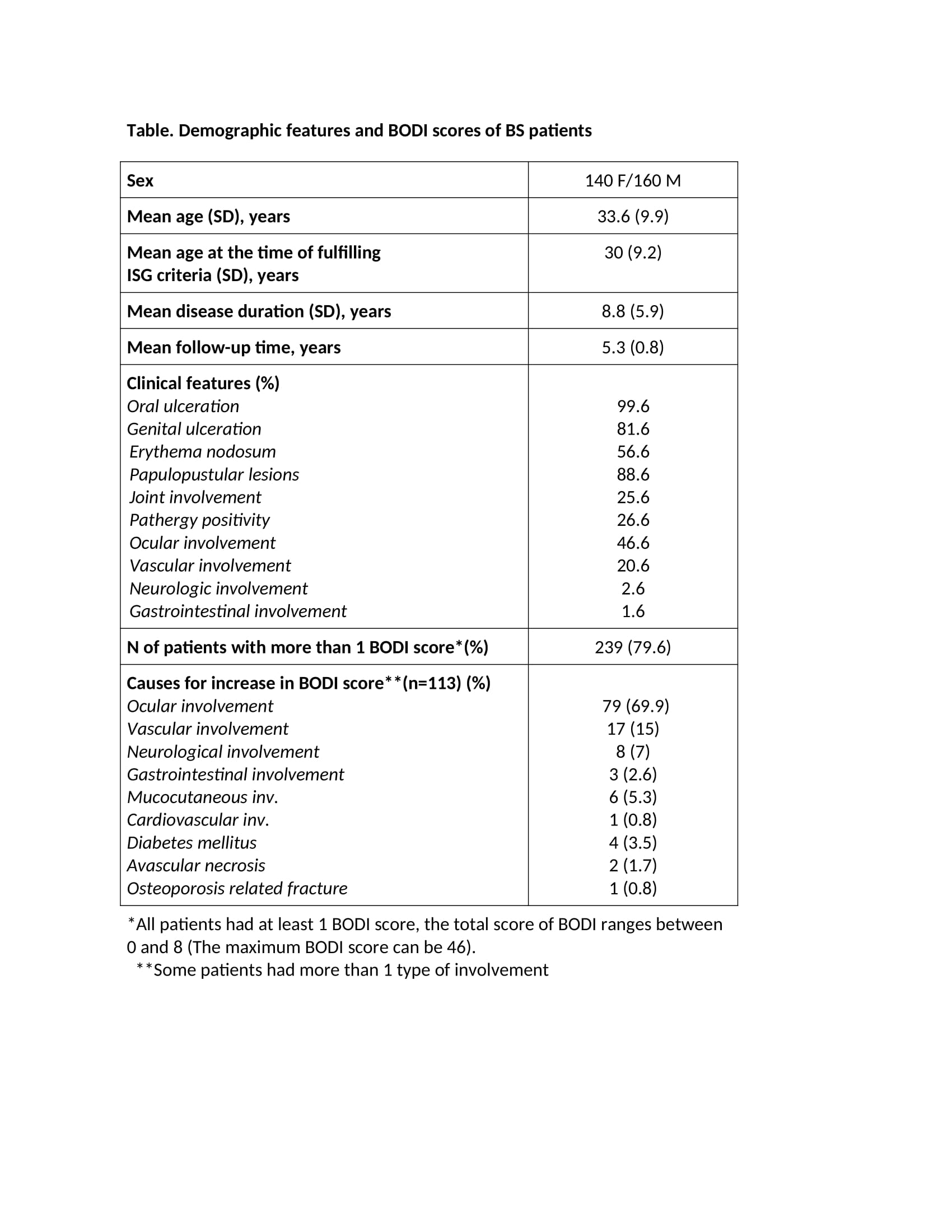 Table. Demographic features and BODI scores of BS patients
Table. Demographic features and BODI scores of BS patientsDisclosures: Y. Yagiz Ozogul, None; Y. Ozguler, UCB, Novartis, Pfizer; D. Ucar, None; U. Uygunoglu, None; Z. Kutlubay, None; V. Hamuryudan, Celgene, AbbVie/Abbott, Novartis, UCB; g. Hatemi, Celgene, UCB, Novartis, AbbVie/Abbott.

