Back
Poster Session C
Pediatric autoimmune diseases: Kawasaki disease, juvenile dermatomyositis and juvenile localized scleroderma
Session: (1360–1386) Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
1362: Validation of the 2016 ACR/EULAR Myositis Response Criteria in Juvenile Dermatomyositis (JDM) Clinical Trials and Consensus Profiles
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
Hanna Kim, MD, MS
NIAMS, NIH
Bethesda, MD, United States
Abstract Poster Presenter(s)
Hanna Kim1, Didem Saygin2, Christian Douglas3, john mcgrath3, Jesse Wilkerson3, angela Pistorio4, Ann Reed5, Chester Oddis6, Frederick Miller7, Jiří Vencovský8, Nicola Ruperto9, Rohit Aggarwal10 and Lisa G Rider7, 1Division of Rheumatology, Department of Medicine, George Washington University School of Medicine and Health Sciences; Juvenile Myositis Therapeutic and Translation Studies Unit, PTRB, NIAMS, NIH, Bethesda, MD, 2University of Chicago, Chicago, IL, 3Social and Scientific Systems, Inc., Durham, NC, 4IRCCS Istituto Giannina Gaslini, Genoa, Italy, 5Duke University School of Medicine, Durham, NC, 6University of Pittsburgh, Pittsburgh, PA, 7Environmental Autoimmunity Group, Clinical Research Branch, National Institute of Environmental Health Sciences (NIEHS), National Institutes of Health, Bethesda, MD, 8Institute of Rheumatology and Department of Rheumatology, First Faculty of Medicine, Charles University, Prague, Czech Republic, 9IRCCS Istituto Giannina Gaslini; PRINTO, Clinica Pediatrica e Reumatologia, Genova, Italy, 10Division of Rheumatology and Clinical Immunology, Department of Medicine, University of Pittsburgh, Pittsburgh, PA
Background/Purpose: Juvenile dermatomyositis (JDM) ACR-EULAR myositis response criteria (MRC) were developed based on absolute % changes in 6 core set measures (CSM) differentially weighted to calculate a Total Improvement Score (TIS). Performance of MRC TIS has not been well-characterized. How changes in International Myositis Assessment & Clinical Studies (IMACS) vs. Paediatric Rheumatology INTernational Trials Organization (PRINTO) CSMs compare, and clinical significance of MRC categories are also unclear. Whether patients can achieve MRC with worsening in individual CSMs, specificity to muscle-related CSMs, and representation of patient-reported (PRO) CSMs are unknown. We aimed to assess the contribution of each CSM to TIS, frequency of muscle CSM improvement among improved patients, representation of PRO in the TIS, relationship of IMACS vs. PRINTO CSMs, frequency of worsening CSMs, and clinical significance of the TIS.
Methods: JDM patients enrolled in the Rituximab in Myositis trial (n=48), PRINTO treatment trial (n=139), and consensus profiles from natural history studies (n=273) were included. TIS and number of improving/worsening CSMs by improvement category were examined. Sign test compared observed vs. expected contribution of each CSM. Frequency of improvement with and without muscle-related CSMs and PRO CSM was calculated. We compared improvement categories by Wilcoxon tests with Bonferroni-adjusted p-values. Change in IMACS and PRINTO CSM and TIS were compared by correlation analysis. Physician rating of change category was compared to MRC improvement categories by weighted Cohen's Κ test.
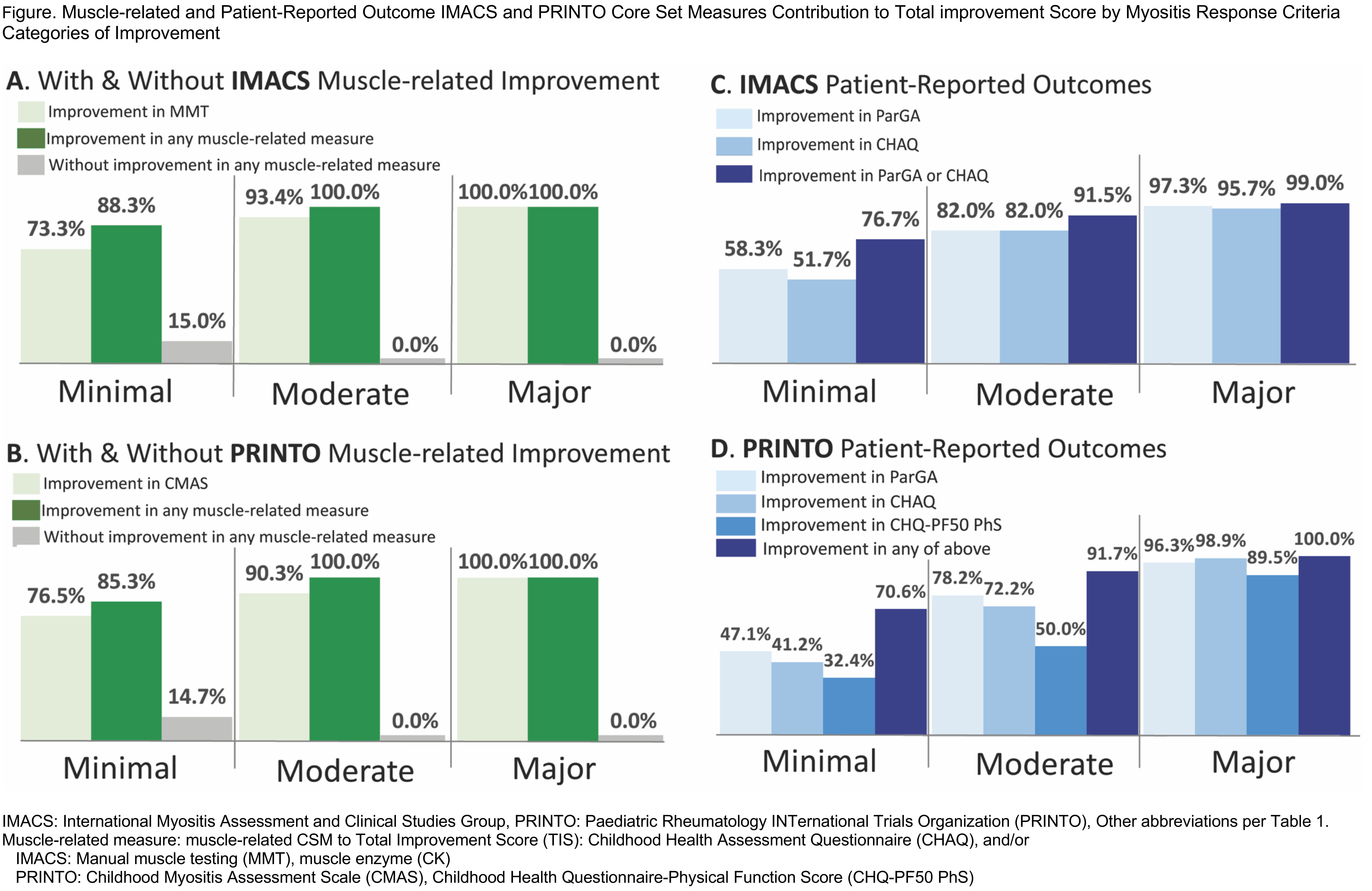
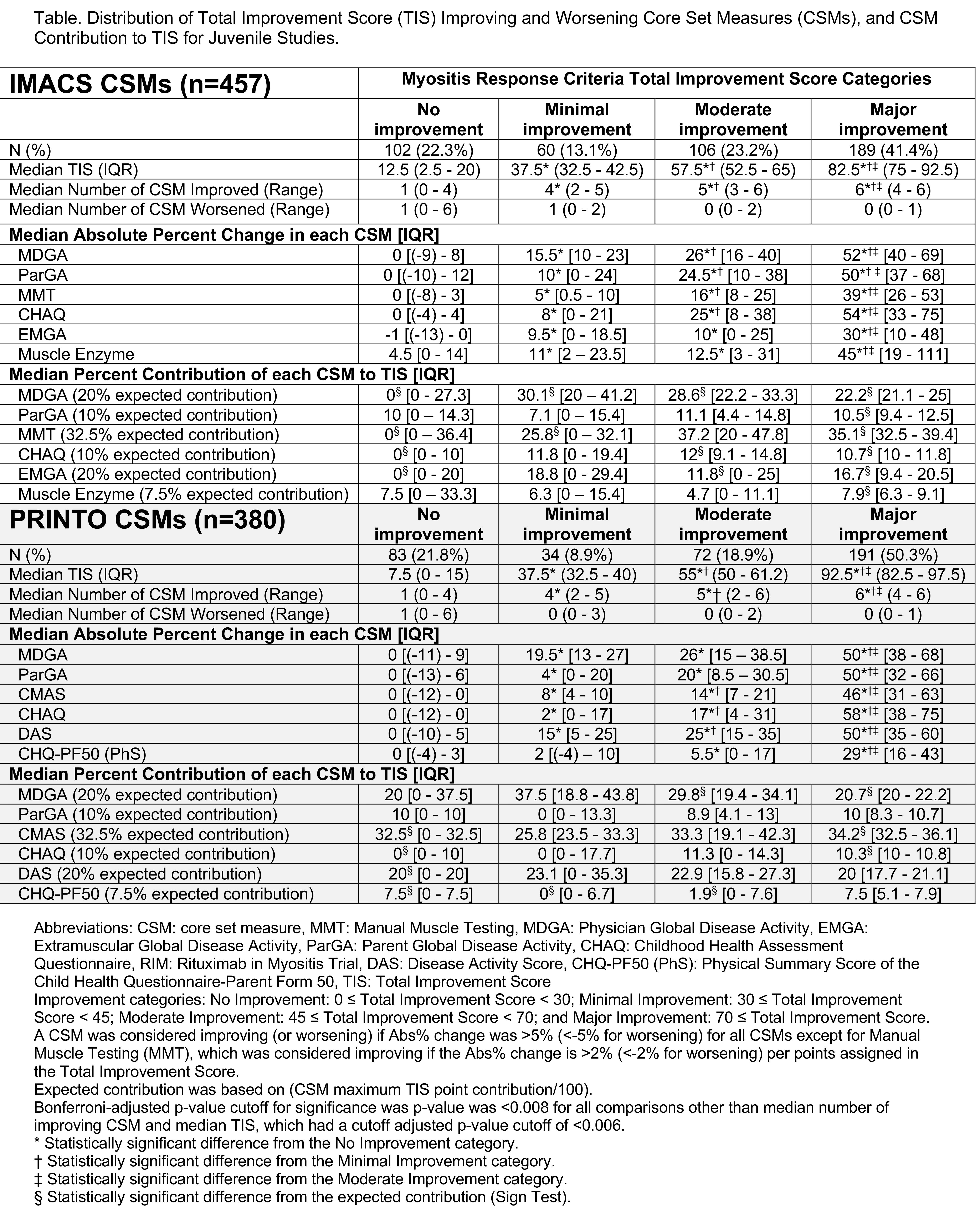
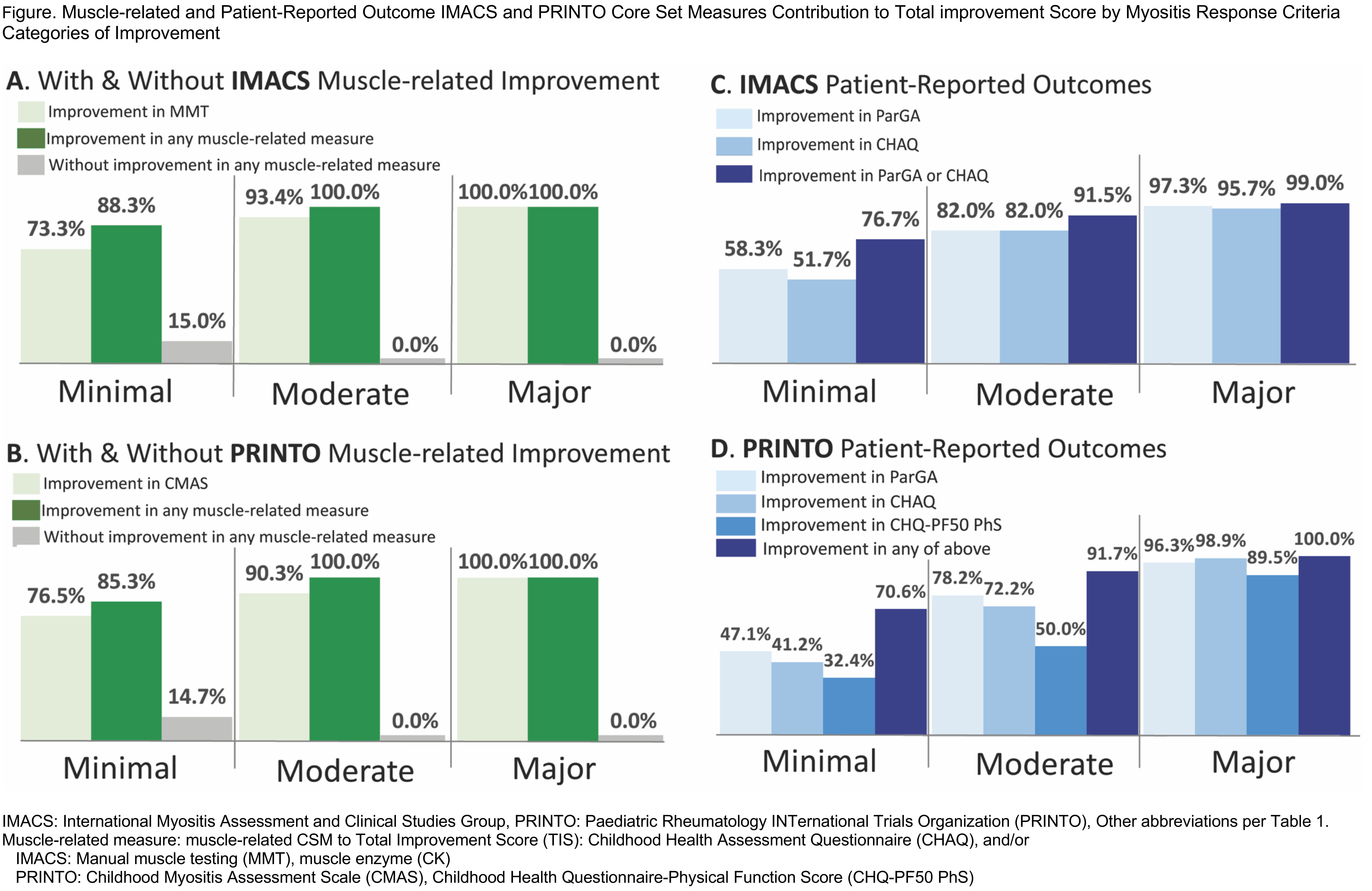
Results: Of 457 total JDM patients with IMACS CSM/ 380 with PRINTO CSM, 13%/ 9% had minimal improvement, 23%/ 19% had moderate improvement, and 41%/ 50% had major improvement using IMACS and PRINTO CSMs (Table). The number of improved CSMs increased with higher MRC improvement categories, as did the percentage change in all CSMs (Table1). Patients with no improvement had a median of 1 CSM worsening, whereas patients with moderate-major improvement had median zero CSM worsening. With minimal improvement, most CSMs contribute to TIS as expected (Table1). Of patients who had at least minimal improvement, 94%/95% had improvement in Manual Muscle Testing or Childhood Myositis Assessment Scale. Of patients with at least minimal improvement, 93%/95% had improvement in at least 1 PRO (IMACS/ PRINTO) (Figure). IMACS and PRINTO CSMs perform similarly for MRC; Changes in CSM for IMACS vs. PRINTO significantly correlated for most measures. Physician-rated categories of change significantly correlated with the TIS improvement categories (weighted Cohen's κ values 0.5-0.8).
Conclusion: Most JDM patients who improve by the MRC show improvement in muscle-related CSM. MRC improvement also reflects improvement in PRO. Among those who improve by MRC, worsening of CSM is infrequent. Most changes in CSM are significantly correlated between IMACS and PRINTO. MRC TIS categories significantly correlated with clinically meaningful changes by physician assessment. The ACR-EULAR MRC seem robust for the assessment of JDM and perform consistently across these studies.
Acknowledgements: IRP of NIH, NIEHS, NIAMS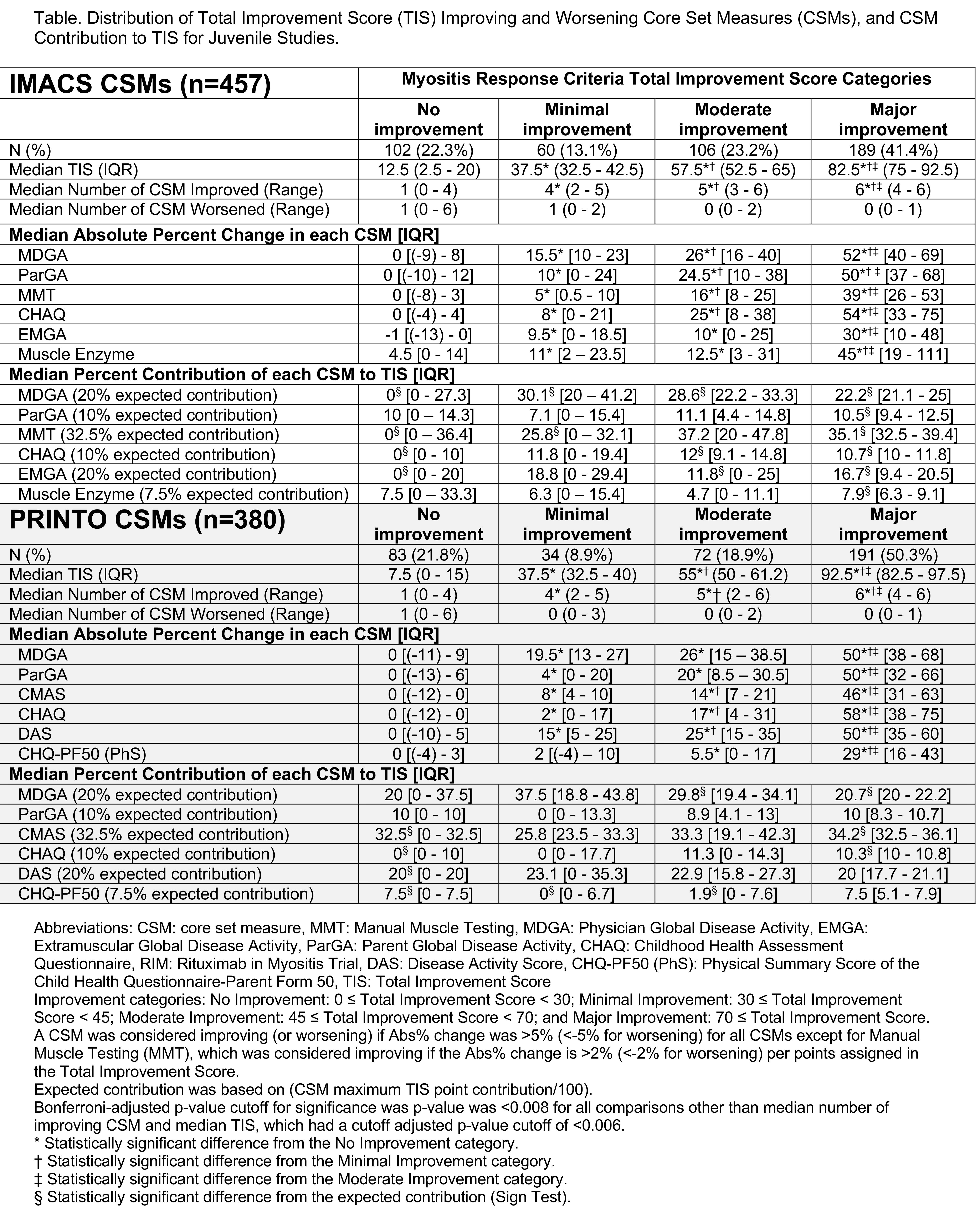
Disclosures: H. Kim, Eli Lilly and Company; D. Saygin, None; C. Douglas, None; j. mcgrath, None; J. Wilkerson, None; a. Pistorio, None; A. Reed, None; C. Oddis, None; F. Miller, None; J. Vencovský, Abbvie, Biogen, Boehringer, Eli Lilly, Gilead, Kezar, Merck, Novartis, Octapharma, Pfizer, Takeda, UCB, Werfen, Argenx; N. Ruperto, 2 Bridge, Amgen, AstraZeneca, Aurinia, Bayer, Brystol Myers and Squibb, Celgene, inMed, Cambridge Healthcare Research, Domain Therapeutic,, EMD Serono, Glaxo Smith Kline, Idorsia, Janssen, Eli Lilly, Novartis, Pfizer, Sobi, UCB; R. Aggarwal, Mallinckrodt, Bristol Myers Squibb, EMD Serono, Pfizer, Octapharma, CSL Behring, Q32, Kezar, AstraZeneca, Alexion, Argenx, Boehringer Ingelheim, Corbus, Janssen, Kyverna, Roivant, AbbVie, Jubilant, Orphazyme, Genentech; L. Rider, Hope Pharmaceuticals, Pfizer, Bristol-Myers Squibb(BMS).
Background/Purpose: Juvenile dermatomyositis (JDM) ACR-EULAR myositis response criteria (MRC) were developed based on absolute % changes in 6 core set measures (CSM) differentially weighted to calculate a Total Improvement Score (TIS). Performance of MRC TIS has not been well-characterized. How changes in International Myositis Assessment & Clinical Studies (IMACS) vs. Paediatric Rheumatology INTernational Trials Organization (PRINTO) CSMs compare, and clinical significance of MRC categories are also unclear. Whether patients can achieve MRC with worsening in individual CSMs, specificity to muscle-related CSMs, and representation of patient-reported (PRO) CSMs are unknown. We aimed to assess the contribution of each CSM to TIS, frequency of muscle CSM improvement among improved patients, representation of PRO in the TIS, relationship of IMACS vs. PRINTO CSMs, frequency of worsening CSMs, and clinical significance of the TIS.
Methods: JDM patients enrolled in the Rituximab in Myositis trial (n=48), PRINTO treatment trial (n=139), and consensus profiles from natural history studies (n=273) were included. TIS and number of improving/worsening CSMs by improvement category were examined. Sign test compared observed vs. expected contribution of each CSM. Frequency of improvement with and without muscle-related CSMs and PRO CSM was calculated. We compared improvement categories by Wilcoxon tests with Bonferroni-adjusted p-values. Change in IMACS and PRINTO CSM and TIS were compared by correlation analysis. Physician rating of change category was compared to MRC improvement categories by weighted Cohen's Κ test.
Results: Of 457 total JDM patients with IMACS CSM/ 380 with PRINTO CSM, 13%/ 9% had minimal improvement, 23%/ 19% had moderate improvement, and 41%/ 50% had major improvement using IMACS and PRINTO CSMs (Table). The number of improved CSMs increased with higher MRC improvement categories, as did the percentage change in all CSMs (Table1). Patients with no improvement had a median of 1 CSM worsening, whereas patients with moderate-major improvement had median zero CSM worsening. With minimal improvement, most CSMs contribute to TIS as expected (Table1). Of patients who had at least minimal improvement, 94%/95% had improvement in Manual Muscle Testing or Childhood Myositis Assessment Scale. Of patients with at least minimal improvement, 93%/95% had improvement in at least 1 PRO (IMACS/ PRINTO) (Figure). IMACS and PRINTO CSMs perform similarly for MRC; Changes in CSM for IMACS vs. PRINTO significantly correlated for most measures. Physician-rated categories of change significantly correlated with the TIS improvement categories (weighted Cohen's κ values 0.5-0.8).
Conclusion: Most JDM patients who improve by the MRC show improvement in muscle-related CSM. MRC improvement also reflects improvement in PRO. Among those who improve by MRC, worsening of CSM is infrequent. Most changes in CSM are significantly correlated between IMACS and PRINTO. MRC TIS categories significantly correlated with clinically meaningful changes by physician assessment. The ACR-EULAR MRC seem robust for the assessment of JDM and perform consistently across these studies.
Acknowledgements: IRP of NIH, NIEHS, NIAMS
Disclosures: H. Kim, Eli Lilly and Company; D. Saygin, None; C. Douglas, None; j. mcgrath, None; J. Wilkerson, None; a. Pistorio, None; A. Reed, None; C. Oddis, None; F. Miller, None; J. Vencovský, Abbvie, Biogen, Boehringer, Eli Lilly, Gilead, Kezar, Merck, Novartis, Octapharma, Pfizer, Takeda, UCB, Werfen, Argenx; N. Ruperto, 2 Bridge, Amgen, AstraZeneca, Aurinia, Bayer, Brystol Myers and Squibb, Celgene, inMed, Cambridge Healthcare Research, Domain Therapeutic,, EMD Serono, Glaxo Smith Kline, Idorsia, Janssen, Eli Lilly, Novartis, Pfizer, Sobi, UCB; R. Aggarwal, Mallinckrodt, Bristol Myers Squibb, EMD Serono, Pfizer, Octapharma, CSL Behring, Q32, Kezar, AstraZeneca, Alexion, Argenx, Boehringer Ingelheim, Corbus, Janssen, Kyverna, Roivant, AbbVie, Jubilant, Orphazyme, Genentech; L. Rider, Hope Pharmaceuticals, Pfizer, Bristol-Myers Squibb(BMS).

