Back
Poster Session C
Epidemiology, health policy and outcomes
Session: (1332–1359) Patient Outcomes, Preferences, and Attitudes Poster II
1348: We Asked Patients and Families: What Is the Job of a Pediatric Rheumatologist?
Sunday, November 13, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- EH
Emily Hause, MD, MPH
University of Minnesota
Minneapolis, MN, United States
Abstract Poster Presenter(s)
Emily Hause1, Nathan Rubin2, Bryce Binstadt1, Colleen Correll1, Patricia Hobday1, Alison Lerman1, Shawn Mahmud1, Mona Riskalla1, Meghan Ryan3, Zachary Shaheen1 and Danielle Bullock1, 1University of Minnesota, Minneapolis, MN, 2University of Minnesota Masonic Cancer Center, Minneapolis, MN, 3University of Minnesota, Vadnais Heights, MN
Background/Purpose: Pediatric rheumatology is a highly specialized field, with approximately 300 practicing pediatric rheumatologists in the United States. Prior research into patient understanding of medical specialties demonstrated that most patients were unable to correctly describe the roles of an oncologist and radiologist, with 43% and 28% correctly identifying these roles respectively. We hypothesized that, given the specialized nature of the field, patients and their families might have difficulty defining the job of a pediatric rheumatologist. In order to ultimately target improvement efforts, we studied factors impacting concordance of patients' and their guardians' definitions of the job of a pediatric rheumatologist with the definition provided by the pediatric rheumatologists in our practice.
Methods: We surveyed patients or their guardian being seen at the University of Minnesota pediatric rheumatology clinic on twelve half-days of clinic. We asked, "What is the job of a pediatric rheumatologist?". Respondents answered with free text on paper. We collected data on number of visits to the pediatric rheumatology clinic, whether the respondent was a patient or guardian, and age of the respondent. Free responses were analyzed and coded according to the presence of three key response elements, which were determined via analysis of answers to the same question posed to our pediatric rheumatology attending physicians and fellows: 1) inclusion of child/teen/adolescent, 2) inclusion of a verb indicating diagnosis/treatment/management, and 3) specialty specific knowledge with words like autoimmune/arthritis/lupus. We then utilized a quasi-Poisson regression model to determine if the number of visits (2+ vs 1) was associated with answers that included more of the key response elements after adjusting for (1) age (continuous) or (2) patient vs guardian response (binary age with a cutoff of 22 years).
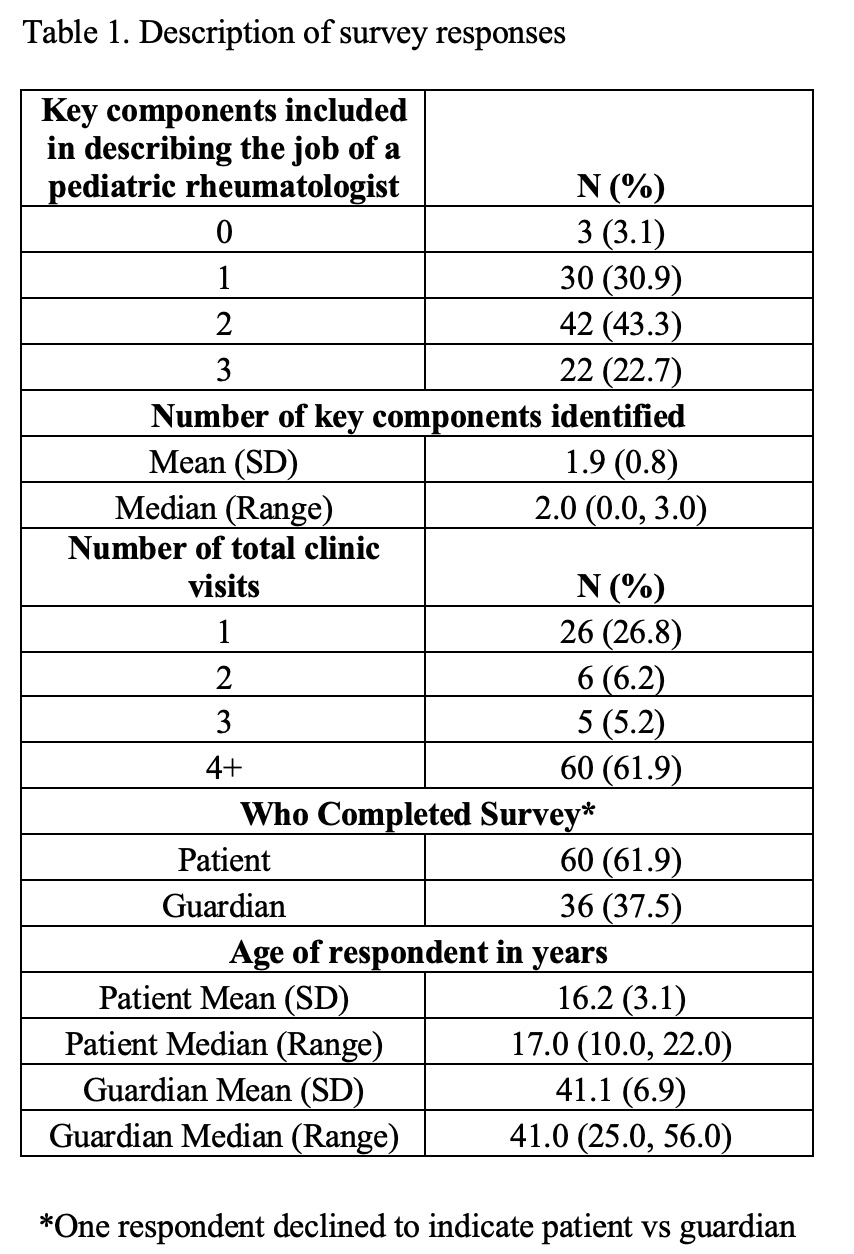
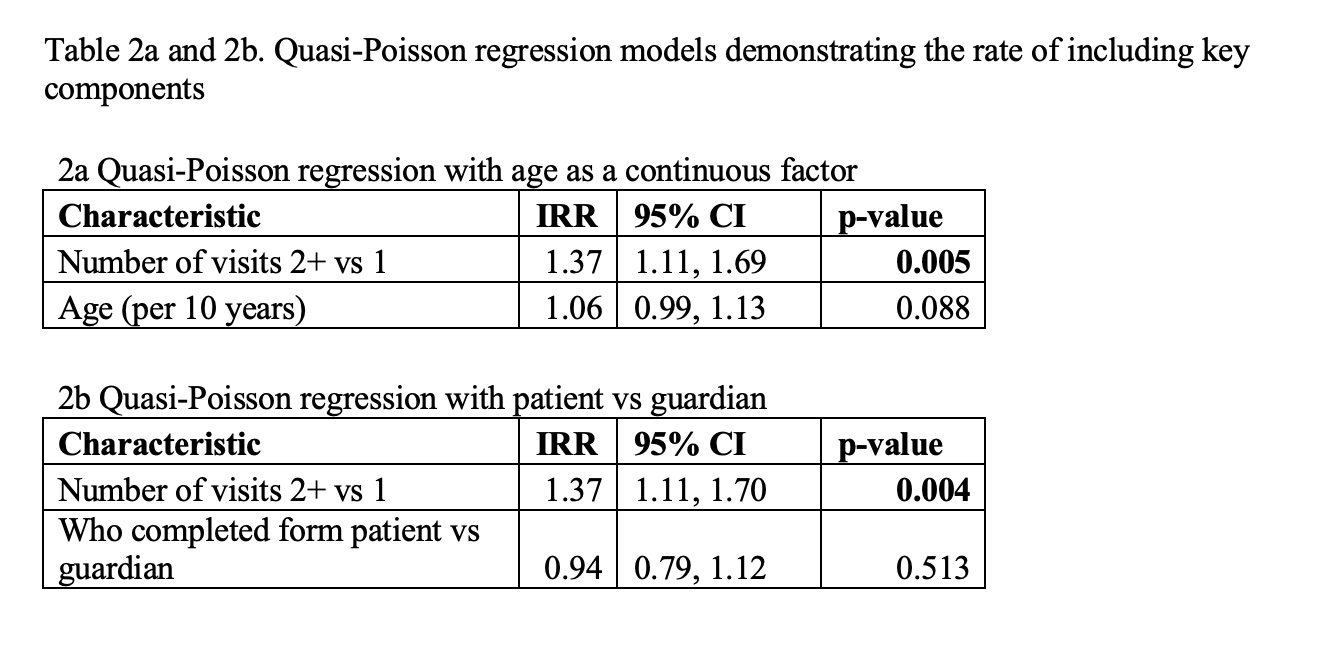
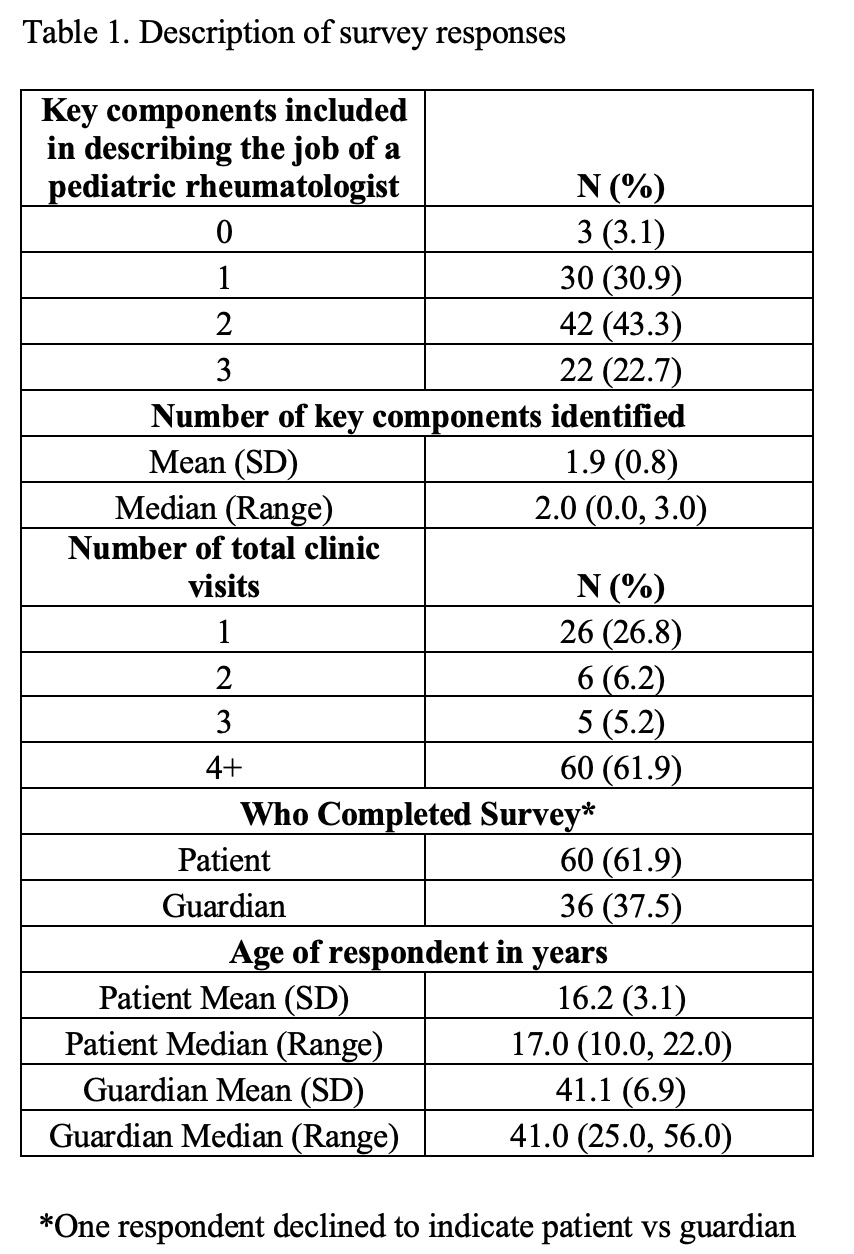
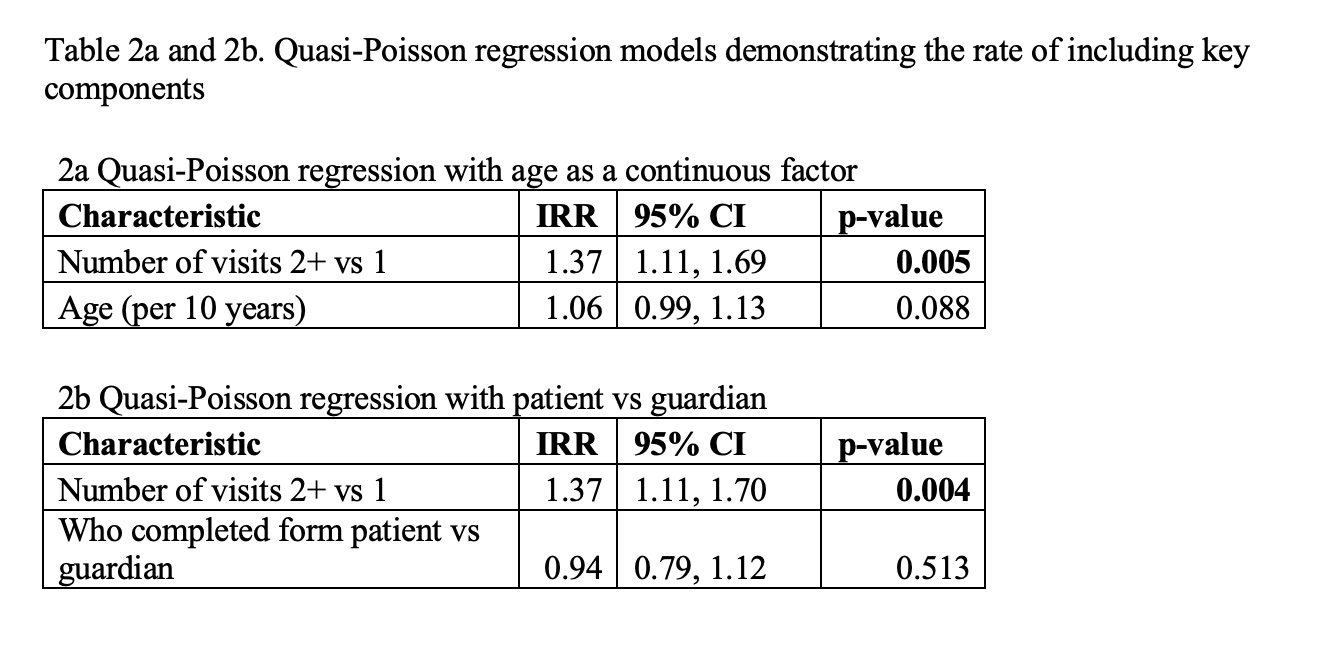
Results: Our survey completion rate was 95% (97/102), with 37.5% of surveys completed by a guardian. The majority, 61.9%, were completed by participants who had 4+ visits. Twenty-two respondents (22.7%) included all three key response elements, 42 (43.3%) included two, 30 (30.9%) included one, and 3 (3.1%) included zero (Table 1). Number of visits was a significant predictor of inclusion of more key response elements (2+ vs 1 visits) regardless of age or patient vs guardian form completion (Tables 2a and 2b). Neither age nor completion of the form by the patient or guardian was associated with number of key response elements.
Conclusion: These data serve as a baseline to target future quality improvement interventions to expand patient/guardian understanding of the job of pediatric rheumatologists. Two-thirds of our surveyed population included 2 or more of the 3 key response elements. Participants who had visited the pediatric rheumatology clinic more often had responses that were more closely aligned with the physicians' definitions of the job of a pediatric rheumatologist. Not surprisingly, this suggests that understanding of the profession increases with exposure. Therefore, targeting patients/guardians at their initial visit may improve understanding of our specialty.
Disclosures: E. Hause, None; N. Rubin, None; B. Binstadt, Pfizer, Pfizer; C. Correll, None; P. Hobday, None; A. Lerman, None; S. Mahmud, None; M. Riskalla, None; M. Ryan, None; Z. Shaheen, None; D. Bullock, None.
Background/Purpose: Pediatric rheumatology is a highly specialized field, with approximately 300 practicing pediatric rheumatologists in the United States. Prior research into patient understanding of medical specialties demonstrated that most patients were unable to correctly describe the roles of an oncologist and radiologist, with 43% and 28% correctly identifying these roles respectively. We hypothesized that, given the specialized nature of the field, patients and their families might have difficulty defining the job of a pediatric rheumatologist. In order to ultimately target improvement efforts, we studied factors impacting concordance of patients' and their guardians' definitions of the job of a pediatric rheumatologist with the definition provided by the pediatric rheumatologists in our practice.
Methods: We surveyed patients or their guardian being seen at the University of Minnesota pediatric rheumatology clinic on twelve half-days of clinic. We asked, "What is the job of a pediatric rheumatologist?". Respondents answered with free text on paper. We collected data on number of visits to the pediatric rheumatology clinic, whether the respondent was a patient or guardian, and age of the respondent. Free responses were analyzed and coded according to the presence of three key response elements, which were determined via analysis of answers to the same question posed to our pediatric rheumatology attending physicians and fellows: 1) inclusion of child/teen/adolescent, 2) inclusion of a verb indicating diagnosis/treatment/management, and 3) specialty specific knowledge with words like autoimmune/arthritis/lupus. We then utilized a quasi-Poisson regression model to determine if the number of visits (2+ vs 1) was associated with answers that included more of the key response elements after adjusting for (1) age (continuous) or (2) patient vs guardian response (binary age with a cutoff of 22 years).
Results: Our survey completion rate was 95% (97/102), with 37.5% of surveys completed by a guardian. The majority, 61.9%, were completed by participants who had 4+ visits. Twenty-two respondents (22.7%) included all three key response elements, 42 (43.3%) included two, 30 (30.9%) included one, and 3 (3.1%) included zero (Table 1). Number of visits was a significant predictor of inclusion of more key response elements (2+ vs 1 visits) regardless of age or patient vs guardian form completion (Tables 2a and 2b). Neither age nor completion of the form by the patient or guardian was associated with number of key response elements.
Conclusion: These data serve as a baseline to target future quality improvement interventions to expand patient/guardian understanding of the job of pediatric rheumatologists. Two-thirds of our surveyed population included 2 or more of the 3 key response elements. Participants who had visited the pediatric rheumatology clinic more often had responses that were more closely aligned with the physicians' definitions of the job of a pediatric rheumatologist. Not surprisingly, this suggests that understanding of the profession increases with exposure. Therefore, targeting patients/guardians at their initial visit may improve understanding of our specialty.
Disclosures: E. Hause, None; N. Rubin, None; B. Binstadt, Pfizer, Pfizer; C. Correll, None; P. Hobday, None; A. Lerman, None; S. Mahmud, None; M. Riskalla, None; M. Ryan, None; Z. Shaheen, None; D. Bullock, None.

