Back
Poster Session A
Vasculitis
Session: (0432–0457) Vasculitis – ANCA-Associated Poster I: Epidemiology, Outcomes, and Classification
0451: Incidence and Prevalence of ANCA-associated Vasculitis in Southern Sweden – a 23-year Study
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JR
Jens Rathmann, MD
Region Skåne, Lund University
Lund, Sweden
Abstract Poster Presenter(s)
Jens Rathmann1, Mårten Segelmark2, Martin Englund3 and Aladdin Mohammad4, 1Rheumatology, Department of Clinical Sciences, Lund University, Lund, Skane Lan, Sweden, 2Nephrology, Department of Clinical Sciences, Lund University, Lund, Sweden, 3Lund University, Lund, Sweden, 4Rheumatology, Department of Clinical Sciences, Lund University, Lund, Sweden
Background/Purpose: Epidemiologic studies in ANCA associated vasculitis (AAV) have demonstrated geographical variation between different countries as well as increasing incidence and prevalence during the last 30 years. Some of these differences can be attributed to genetic and environmental factors, however different methodology for case-identification, increased physician awareness and improved survival might also influence results. We earlier described an incidence rate of 20.9/million inhabitants (1) and a point prevalence of 299/million for AAV in the same study area in 2003 (2). In this study we aim to update the epidemiology of AAV in a defined geographic area in southern Sweden using same case ascertainment and classification.
Methods: For the incidence estimation, the study area comprises 14 municipalities in southern Sweden with a total adult population (≥ 18 years) of 623 872 in 2019. All cases diagnosed with AAV from 1997 to 2019 in the study area were included in this study. Diagnosis of AAV was verified by case record review and cases were classified using EMA-algorithm. To study the point prevalence (p.p.), we included cases from 10 out of the 14 municipalities used in incidence estimates (Pop. 273135), to assure better comparability with previous p.p. results. The date of p.p. was January 1, 2020. Age and sex- specific incidence rates were estimated and the variation in incidence rate according to seasons was studied.
Results: Three hundred and seventy-four patients (47% female) were diagnosed with new onset AAV during study period. 192 patients were classified as GPA, 159 as MPA and 23 as EGPA. The median age at diagnosis was 67.5 (IQR 55—77) years. The average annual incidence rate per million adults was 30.1 (95%CI: 27.0, 33.1) for AAV, 15.4 (95%CI: 13.3, 17.6) for GPA, 12.8 (95%CI: 10.8, 14.8) for MPA and 1.8 (95%CI: 1.1, 2.6) for EGPA. Incidence rate is increasing with age. Age-specific incidence rates for MPA and MPO-positive disease are highest in patients aged 85 and older, whereas overall AAV, GPA and PR3 positive disease show peak incidence rates in patients between 70-84 years and decrease in older age. Incidence rates are highest in spring (IR 1.375, winter reference). At date of p.p. 117 patients were alive in the study area resulting in a p.p. of 428 per million adults. The prevalence was higher in men compared to women.
Conclusion: The incidence of AAV is increasing with older age reaching highest rate among people in age group 70-84 years. Annual incidence rates were stable during the study period. The prevalence of AAV has increased during the study period and is higher in men.
References:
1. Mohammad AJ, Rheumatology (Oxford). 2009;48(12):1560-5.
2. Mohammad AJ, et al. Rheumatology (Oxford) 2007;46:1329-37.
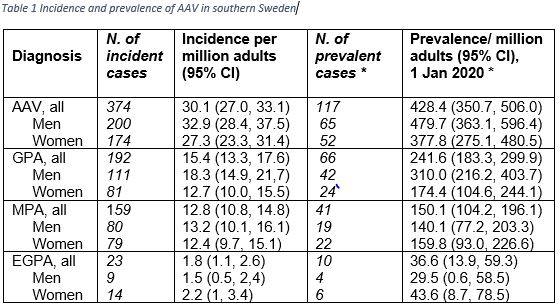 AAV: ANCA-associated vasculitis, GPA: granulomatosis with polyangiitis, MPA: microscopic polyangiitis, EGPA: eosinophilic granulomatosis with polyangiitis, PR3: proteinase-3, MPO: myeloperoxidase, 95% CI: 95% confidence-interval. *The study area for prevalence estimates comprises 10/14 (total population 2020: 273135) municipalities for better comparability to earlier studies in this cohort.
AAV: ANCA-associated vasculitis, GPA: granulomatosis with polyangiitis, MPA: microscopic polyangiitis, EGPA: eosinophilic granulomatosis with polyangiitis, PR3: proteinase-3, MPO: myeloperoxidase, 95% CI: 95% confidence-interval. *The study area for prevalence estimates comprises 10/14 (total population 2020: 273135) municipalities for better comparability to earlier studies in this cohort.
Disclosures: J. Rathmann, None; M. Segelmark, None; M. Englund, None; A. Mohammad, None.
Background/Purpose: Epidemiologic studies in ANCA associated vasculitis (AAV) have demonstrated geographical variation between different countries as well as increasing incidence and prevalence during the last 30 years. Some of these differences can be attributed to genetic and environmental factors, however different methodology for case-identification, increased physician awareness and improved survival might also influence results. We earlier described an incidence rate of 20.9/million inhabitants (1) and a point prevalence of 299/million for AAV in the same study area in 2003 (2). In this study we aim to update the epidemiology of AAV in a defined geographic area in southern Sweden using same case ascertainment and classification.
Methods: For the incidence estimation, the study area comprises 14 municipalities in southern Sweden with a total adult population (≥ 18 years) of 623 872 in 2019. All cases diagnosed with AAV from 1997 to 2019 in the study area were included in this study. Diagnosis of AAV was verified by case record review and cases were classified using EMA-algorithm. To study the point prevalence (p.p.), we included cases from 10 out of the 14 municipalities used in incidence estimates (Pop. 273135), to assure better comparability with previous p.p. results. The date of p.p. was January 1, 2020. Age and sex- specific incidence rates were estimated and the variation in incidence rate according to seasons was studied.
Results: Three hundred and seventy-four patients (47% female) were diagnosed with new onset AAV during study period. 192 patients were classified as GPA, 159 as MPA and 23 as EGPA. The median age at diagnosis was 67.5 (IQR 55—77) years. The average annual incidence rate per million adults was 30.1 (95%CI: 27.0, 33.1) for AAV, 15.4 (95%CI: 13.3, 17.6) for GPA, 12.8 (95%CI: 10.8, 14.8) for MPA and 1.8 (95%CI: 1.1, 2.6) for EGPA. Incidence rate is increasing with age. Age-specific incidence rates for MPA and MPO-positive disease are highest in patients aged 85 and older, whereas overall AAV, GPA and PR3 positive disease show peak incidence rates in patients between 70-84 years and decrease in older age. Incidence rates are highest in spring (IR 1.375, winter reference). At date of p.p. 117 patients were alive in the study area resulting in a p.p. of 428 per million adults. The prevalence was higher in men compared to women.
Conclusion: The incidence of AAV is increasing with older age reaching highest rate among people in age group 70-84 years. Annual incidence rates were stable during the study period. The prevalence of AAV has increased during the study period and is higher in men.
References:
1. Mohammad AJ, Rheumatology (Oxford). 2009;48(12):1560-5.
2. Mohammad AJ, et al. Rheumatology (Oxford) 2007;46:1329-37.
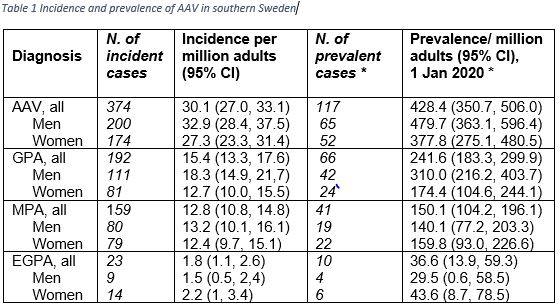 AAV: ANCA-associated vasculitis, GPA: granulomatosis with polyangiitis, MPA: microscopic polyangiitis, EGPA: eosinophilic granulomatosis with polyangiitis, PR3: proteinase-3, MPO: myeloperoxidase, 95% CI: 95% confidence-interval. *The study area for prevalence estimates comprises 10/14 (total population 2020: 273135) municipalities for better comparability to earlier studies in this cohort.
AAV: ANCA-associated vasculitis, GPA: granulomatosis with polyangiitis, MPA: microscopic polyangiitis, EGPA: eosinophilic granulomatosis with polyangiitis, PR3: proteinase-3, MPO: myeloperoxidase, 95% CI: 95% confidence-interval. *The study area for prevalence estimates comprises 10/14 (total population 2020: 273135) municipalities for better comparability to earlier studies in this cohort.Disclosures: J. Rathmann, None; M. Segelmark, None; M. Englund, None; A. Mohammad, None.

