Back
Poster Session A
Rheumatoid arthritis (RA)
Session: (0272–0316) RA – Treatment Poster I
0306: Maintenance of Disease Activity and Treatment Persistence in Patients with Rheumatoid Arthritis Who Switched from Combination to TNF Inhibitor Monotherapy: Results from the Rheumatology Informatics System for Effectiveness (RISE) Registry
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
- SS
Scott Stryker, MD, MPH, DrPH
Amgen, Inc
San Francisco, CA, United States
Abstract Poster Presenter(s)
Gabriela Schmajuk1, Nevin Hammam2, Jing Li3, David Collier4, Greg Kricorian5 and Scott Stryker6, 1UCSF / SFVA, San Francisco, CA, 2Rheumatology Department, Faculty of Medicine, Assiut University, Assiut, Egypt, PASADENA, CA, 3University of California, San Francisco, San Francisco, CA, 4Amgen Inc., Simi Valley, CA, 5Amgen, Inc., Thousand Oaks, CA, 6Amgen Inc., San Francisco, CA
Background/Purpose: Data regarding the maintenance of disease activity (DA) and treatment persistence in patients (pts) who switched from combination therapy to monotherapy for the management of RA in real-world settings are limited. Therefore, we examined the maintenance of remission (REM) or low DA (LDA) and treatment persistence in pts who switched from combination therapy (conventional synthetic [cs]DMARD + etanercept [ETN] or csDMARD + other TNF inhibitor [TNFi]) to monotherapy with either ETN or other TNFi.
Methods: A retrospective cohort study using Rheumatology Informatics System for Effectiveness (RISE) registry reported data for a 5-year period starting January 1, 2014. Pts (≥18 years) had a confirmed RA diagnosis by ≥2 International Classification of Diseases-9/10 diagnosis codes (≥30 days apart), with ≥1 diagnosis code before the index date (date of switch to monotherapy). They received combination of a csDMARD and a TNFi for ≥60 days and had ≥6 months (M) of follow-up on monotherapy. We assessed the proportion of pts who remained on ETN vs other TNFi monotherapy based on index date and prior exposure to non-TNFi biologic (b)DMARDs in the treatment persistence cohort. Pts who had documented DA scores before and after switching to monotherapy (≥30 days apart) and had achieved REM/LDA within 60 days prior to and up to 14 days after the index date were included in the DA maintenance cohort. Results are presented descriptively. Cumulative probability of being in REM/LDA and drug survival rates were estimated using Kaplan-Meier curves.
Results: Overall, 7399 pts were included in the treatment persistence cohort; 996 pts were included in the DA maintenance cohort, of whom 347 (34.8%) were on ETN and 649 (65.2%) were on other TNFi (adalimumab, infliximab, certolizumab pegol, or golimumab). The mean (SD) age of pts was 59.2 (14.80) years; most were female (78.1%), White (68.7%), and received MTX (75.1%) at baseline. The baseline demographics and clinical characteristics were comparable between ETN and other TNFi monotherapy groups (Table 1). During follow-up, most pts remained in REM/LDA, and the proportion who maintained REM/LDA based on CDAI was numerically higher in pts receiving ETN vs other TNFi (88.2% vs 80.5% and 78.8% vs 70.0% at 6 and 12 M, respectively; Fig 1a). Subgroup analyses stratified by baseline REM and LDA status showed that, for pts in REM at baseline, the proportion who maintained REM/LDA at follow-up was similar between groups; however, for pts with LDA at baseline, the proportion who maintained REM/LDA was numerically higher in pts receiving ETN vs other TNFi, especially at 12 M of follow-up (Fig 1b and 1c). In the treatment persistence cohort, persistence rates were similar between ETN and other TNFi groups at both timepoints (60.6% vs 61.3% and 43.8% vs 44.2% at 6 and 12 M, respectively; Fig 2). Subanalyses based on prior exposure to non-TNFi bDMARDs also showed similar persistence between groups; however, the persistence rates were lower for pts with prior exposure to non-TNFi bDMARDs (Fig 2).
Conclusion: Results from RISE showed better disease control among pts who switched from combination therapy to ETN than in those who switched to other TNFi monotherapies, despite similar persistence rates.
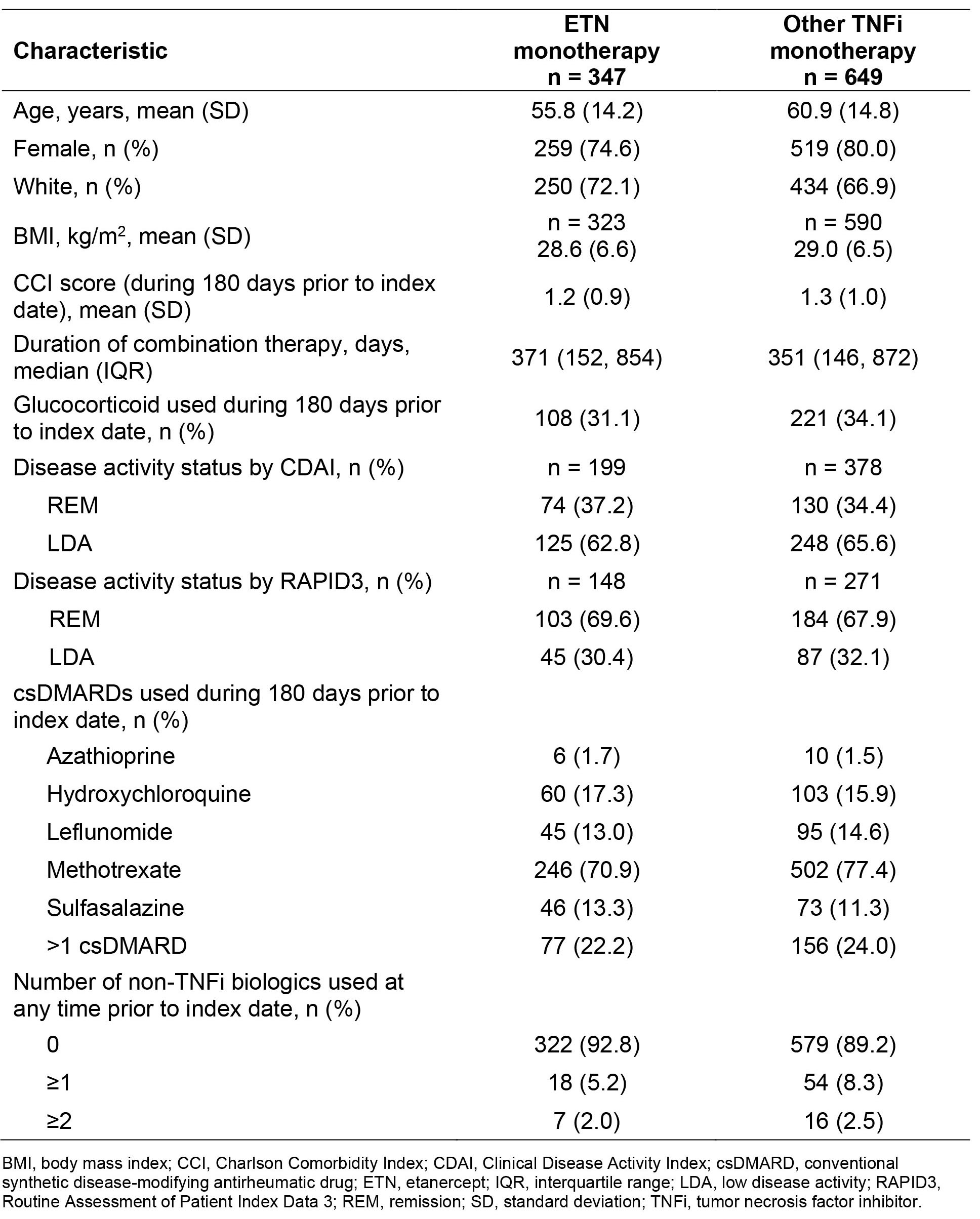 Table 1. Demographics and clinical characteristics of patients with baseline REM or LDA receiving ETN and other TNFi monotherapy after combination therapy [disease activity maintenance cohort]
Table 1. Demographics and clinical characteristics of patients with baseline REM or LDA receiving ETN and other TNFi monotherapy after combination therapy [disease activity maintenance cohort]
.jpg) Figure 1. Proportion of patients maintaining REM or LDA with ETN versus other TNFi monotherapy in the overall population (a), and in subgroup of patients with REM (b) or LDA (c) at baseline [disease activity maintenance cohort]
Figure 1. Proportion of patients maintaining REM or LDA with ETN versus other TNFi monotherapy in the overall population (a), and in subgroup of patients with REM (b) or LDA (c) at baseline [disease activity maintenance cohort]
.jpg) Figure 2. Patients who remained on ETN versus other TNFi monotherapy based on index date (a) and prior exposure to non-TNFi bDMARDs at 6 (b) and 12 months (c) [treatment persistence cohort]
Figure 2. Patients who remained on ETN versus other TNFi monotherapy based on index date (a) and prior exposure to non-TNFi bDMARDs at 6 (b) and 12 months (c) [treatment persistence cohort]
Disclosures: G. Schmajuk, None; N. Hammam, None; J. Li, None; D. Collier, Amgen; G. Kricorian, Amgen; S. Stryker, Amgen.
Background/Purpose: Data regarding the maintenance of disease activity (DA) and treatment persistence in patients (pts) who switched from combination therapy to monotherapy for the management of RA in real-world settings are limited. Therefore, we examined the maintenance of remission (REM) or low DA (LDA) and treatment persistence in pts who switched from combination therapy (conventional synthetic [cs]DMARD + etanercept [ETN] or csDMARD + other TNF inhibitor [TNFi]) to monotherapy with either ETN or other TNFi.
Methods: A retrospective cohort study using Rheumatology Informatics System for Effectiveness (RISE) registry reported data for a 5-year period starting January 1, 2014. Pts (≥18 years) had a confirmed RA diagnosis by ≥2 International Classification of Diseases-9/10 diagnosis codes (≥30 days apart), with ≥1 diagnosis code before the index date (date of switch to monotherapy). They received combination of a csDMARD and a TNFi for ≥60 days and had ≥6 months (M) of follow-up on monotherapy. We assessed the proportion of pts who remained on ETN vs other TNFi monotherapy based on index date and prior exposure to non-TNFi biologic (b)DMARDs in the treatment persistence cohort. Pts who had documented DA scores before and after switching to monotherapy (≥30 days apart) and had achieved REM/LDA within 60 days prior to and up to 14 days after the index date were included in the DA maintenance cohort. Results are presented descriptively. Cumulative probability of being in REM/LDA and drug survival rates were estimated using Kaplan-Meier curves.
Results: Overall, 7399 pts were included in the treatment persistence cohort; 996 pts were included in the DA maintenance cohort, of whom 347 (34.8%) were on ETN and 649 (65.2%) were on other TNFi (adalimumab, infliximab, certolizumab pegol, or golimumab). The mean (SD) age of pts was 59.2 (14.80) years; most were female (78.1%), White (68.7%), and received MTX (75.1%) at baseline. The baseline demographics and clinical characteristics were comparable between ETN and other TNFi monotherapy groups (Table 1). During follow-up, most pts remained in REM/LDA, and the proportion who maintained REM/LDA based on CDAI was numerically higher in pts receiving ETN vs other TNFi (88.2% vs 80.5% and 78.8% vs 70.0% at 6 and 12 M, respectively; Fig 1a). Subgroup analyses stratified by baseline REM and LDA status showed that, for pts in REM at baseline, the proportion who maintained REM/LDA at follow-up was similar between groups; however, for pts with LDA at baseline, the proportion who maintained REM/LDA was numerically higher in pts receiving ETN vs other TNFi, especially at 12 M of follow-up (Fig 1b and 1c). In the treatment persistence cohort, persistence rates were similar between ETN and other TNFi groups at both timepoints (60.6% vs 61.3% and 43.8% vs 44.2% at 6 and 12 M, respectively; Fig 2). Subanalyses based on prior exposure to non-TNFi bDMARDs also showed similar persistence between groups; however, the persistence rates were lower for pts with prior exposure to non-TNFi bDMARDs (Fig 2).
Conclusion: Results from RISE showed better disease control among pts who switched from combination therapy to ETN than in those who switched to other TNFi monotherapies, despite similar persistence rates.
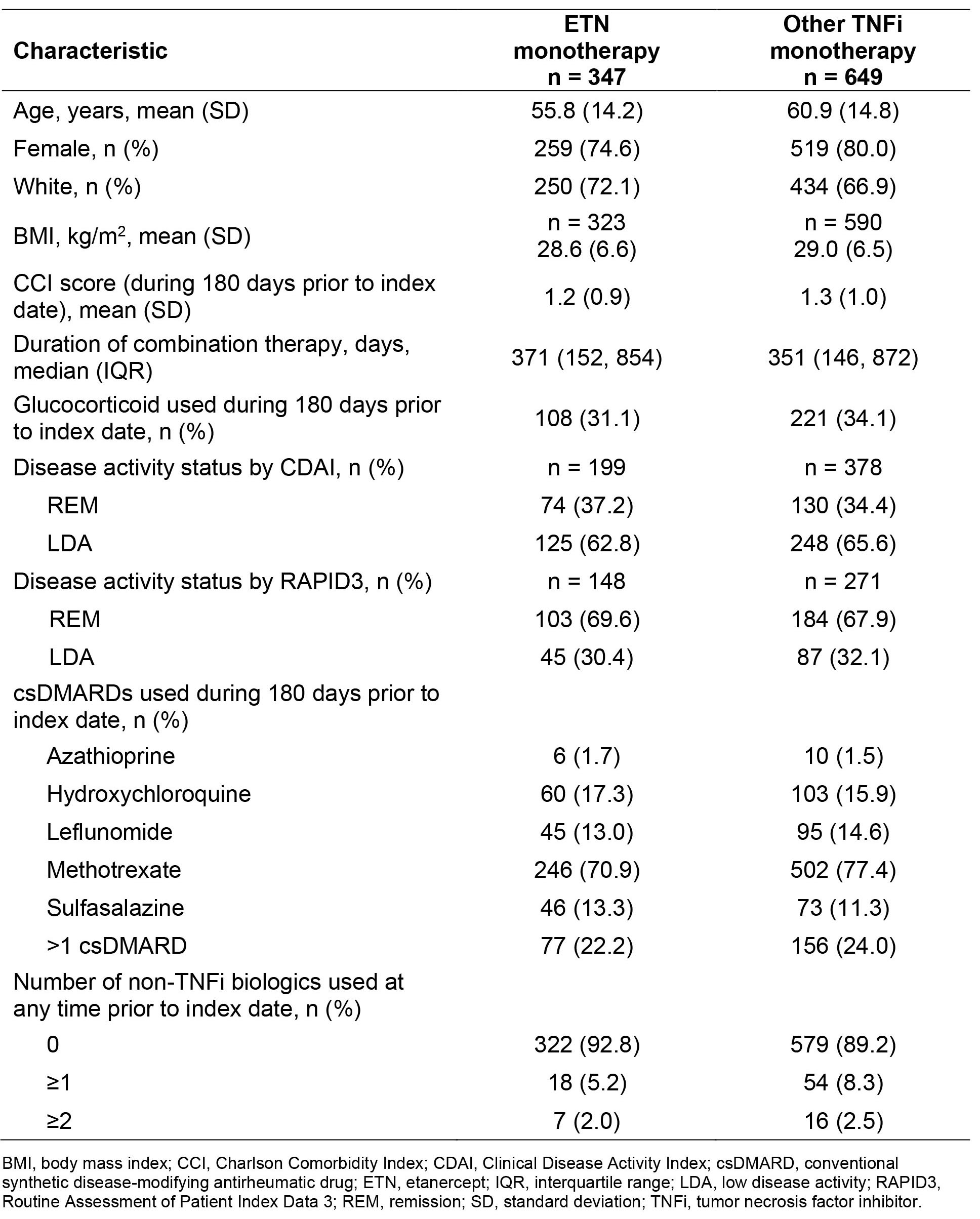 Table 1. Demographics and clinical characteristics of patients with baseline REM or LDA receiving ETN and other TNFi monotherapy after combination therapy [disease activity maintenance cohort]
Table 1. Demographics and clinical characteristics of patients with baseline REM or LDA receiving ETN and other TNFi monotherapy after combination therapy [disease activity maintenance cohort].jpg) Figure 1. Proportion of patients maintaining REM or LDA with ETN versus other TNFi monotherapy in the overall population (a), and in subgroup of patients with REM (b) or LDA (c) at baseline [disease activity maintenance cohort]
Figure 1. Proportion of patients maintaining REM or LDA with ETN versus other TNFi monotherapy in the overall population (a), and in subgroup of patients with REM (b) or LDA (c) at baseline [disease activity maintenance cohort].jpg) Figure 2. Patients who remained on ETN versus other TNFi monotherapy based on index date (a) and prior exposure to non-TNFi bDMARDs at 6 (b) and 12 months (c) [treatment persistence cohort]
Figure 2. Patients who remained on ETN versus other TNFi monotherapy based on index date (a) and prior exposure to non-TNFi bDMARDs at 6 (b) and 12 months (c) [treatment persistence cohort]Disclosures: G. Schmajuk, None; N. Hammam, None; J. Li, None; D. Collier, Amgen; G. Kricorian, Amgen; S. Stryker, Amgen.

