Back
Poster Session A
Spondyloarthritis (SpA) including psoriatic arthritis (PsA)
Session: (0372–0402) Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster I
0387: Sleep Quality in Patients with Psoriatic Arthritis and Its Relationship with Activity and Comorbidity
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- MI
Marta Ibanez Martinez, MD
Hospital Salamanca
Salamanca, Spain
Abstract Poster Presenter(s)
Marta Ibañez Martinez1, Sonia Pastor Navarro2, Olga Compán Fernández2, Belén Miguel Ibáñez2, Ana Isabel Turrión Nieves2, Susana Gómez Castro1, Olga Martínez González2, Cristina Hidalgo Calleja2, Esther Toledano Martinez3 and Carlos Montilla Morales2, 1Hospital Universitario Salamanca, Salamanca, Spain, 2Hospital Universitario de Salamanca, Salamanca, Spain, 3Hospital Clínico San Carlos, Madrid, Spain
Background/Purpose: To evaluate the quality of sleep in patients with psoriatic arthritis (PsA) and its relationship with/to clinical variables, activity, functionality, the impact of the disease, and emotional factors.
Methods: It is a cross-sectional study involving 247 patients diagnosed with psoriatic arthritis. Sleep quality was measured using the PSQI questionnaire. Bivariate correlations were performed between PSQI, gender, number of affected entheses, PASI, peripheral activity (cDAPSA), axial activity (ASDAS-CRP and BASDAI), functionality (BASFI and HAQ), disease impact (PsAID), anxiety, depression (HADS) and fatigue (FACITfatigue). Significant cDAPSA variables, FACIT-F, HADS-A and HADS-D were included in a multiple linear regression model. On the other hand, the PSQI variable was categorized according to the cut-off point PSQI < 6 (good sleep quality) or PSQI ≥ 6 (poor sleep quality).Univariate analysis was performed with baseline variables, disease activity, and the different PROS included between the two groups of patients. Stepwise logistic regression, adjusted for female gender and presence of fibromyalgia, included the significant components of cDAPSA, FACIT-F, HADS-A, and HADS-D as independent variables and PSQI categorization as dependent variable.
Results: 63.15% had poor sleep quality. Of these patients, 46.5% were not taking treatment for insomnia. Female patients with a higher number of affected entheses, higher peripheral and axial activity, fatigue, anxiety, or depression had worse sleep quality. The PSQI was also related to the functionality and impact of the disease. The results are shown in the table. Multiple linear regression modelling revealed that pain [b: 0.48, p< 0.001] and fatigue [b:-0.13, p< 0.001, 95%CI] contributed 43% to the sleep quality pattern. In logistic regression, pain (OR: 1.20 [1.01-1.43)], fatigue [OR: 0.89 (0.84, 0.95)] and anxiety [OR: 1.27 (1.06-1.51)] accounted for 48% of poor sleep quality (PSQI ≥ 6).
Conclusion: Poor sleep quality was frequent in patients with PsA, despite which almost half did not perform any treatment. Emotional factors (fatigue, anxiety) were more relevant than inflammatory factors on sleep quality. The circular relationship between sleep quality, emotional disorders, and activity makes a multidisciplinary approach to the disease necessary.
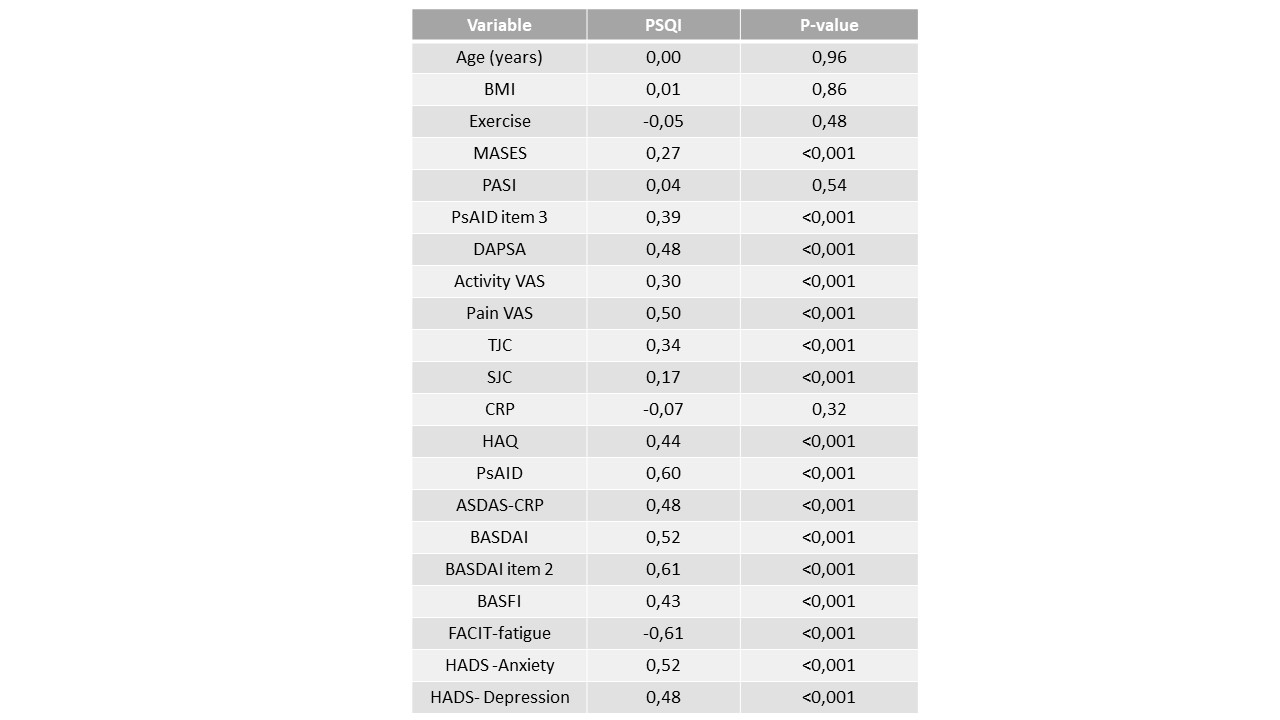 Correlation coefficients between the PSQI and demographic, clinical variables and PROs and index of disease activity, functionality, and impact.
Correlation coefficients between the PSQI and demographic, clinical variables and PROs and index of disease activity, functionality, and impact.
Disclosures: M. Ibañez Martinez, None; S. Pastor Navarro, None; O. Compán Fernández, None; B. Miguel Ibáñez, None; A. Turrión Nieves, None; S. Gómez Castro, None; O. Martínez González, None; C. Hidalgo Calleja, None; E. Toledano Martinez, None; C. Montilla Morales, None.
Background/Purpose: To evaluate the quality of sleep in patients with psoriatic arthritis (PsA) and its relationship with/to clinical variables, activity, functionality, the impact of the disease, and emotional factors.
Methods: It is a cross-sectional study involving 247 patients diagnosed with psoriatic arthritis. Sleep quality was measured using the PSQI questionnaire. Bivariate correlations were performed between PSQI, gender, number of affected entheses, PASI, peripheral activity (cDAPSA), axial activity (ASDAS-CRP and BASDAI), functionality (BASFI and HAQ), disease impact (PsAID), anxiety, depression (HADS) and fatigue (FACITfatigue). Significant cDAPSA variables, FACIT-F, HADS-A and HADS-D were included in a multiple linear regression model. On the other hand, the PSQI variable was categorized according to the cut-off point PSQI < 6 (good sleep quality) or PSQI ≥ 6 (poor sleep quality).Univariate analysis was performed with baseline variables, disease activity, and the different PROS included between the two groups of patients. Stepwise logistic regression, adjusted for female gender and presence of fibromyalgia, included the significant components of cDAPSA, FACIT-F, HADS-A, and HADS-D as independent variables and PSQI categorization as dependent variable.
Results: 63.15% had poor sleep quality. Of these patients, 46.5% were not taking treatment for insomnia. Female patients with a higher number of affected entheses, higher peripheral and axial activity, fatigue, anxiety, or depression had worse sleep quality. The PSQI was also related to the functionality and impact of the disease. The results are shown in the table. Multiple linear regression modelling revealed that pain [b: 0.48, p< 0.001] and fatigue [b:-0.13, p< 0.001, 95%CI] contributed 43% to the sleep quality pattern. In logistic regression, pain (OR: 1.20 [1.01-1.43)], fatigue [OR: 0.89 (0.84, 0.95)] and anxiety [OR: 1.27 (1.06-1.51)] accounted for 48% of poor sleep quality (PSQI ≥ 6).
Conclusion: Poor sleep quality was frequent in patients with PsA, despite which almost half did not perform any treatment. Emotional factors (fatigue, anxiety) were more relevant than inflammatory factors on sleep quality. The circular relationship between sleep quality, emotional disorders, and activity makes a multidisciplinary approach to the disease necessary.
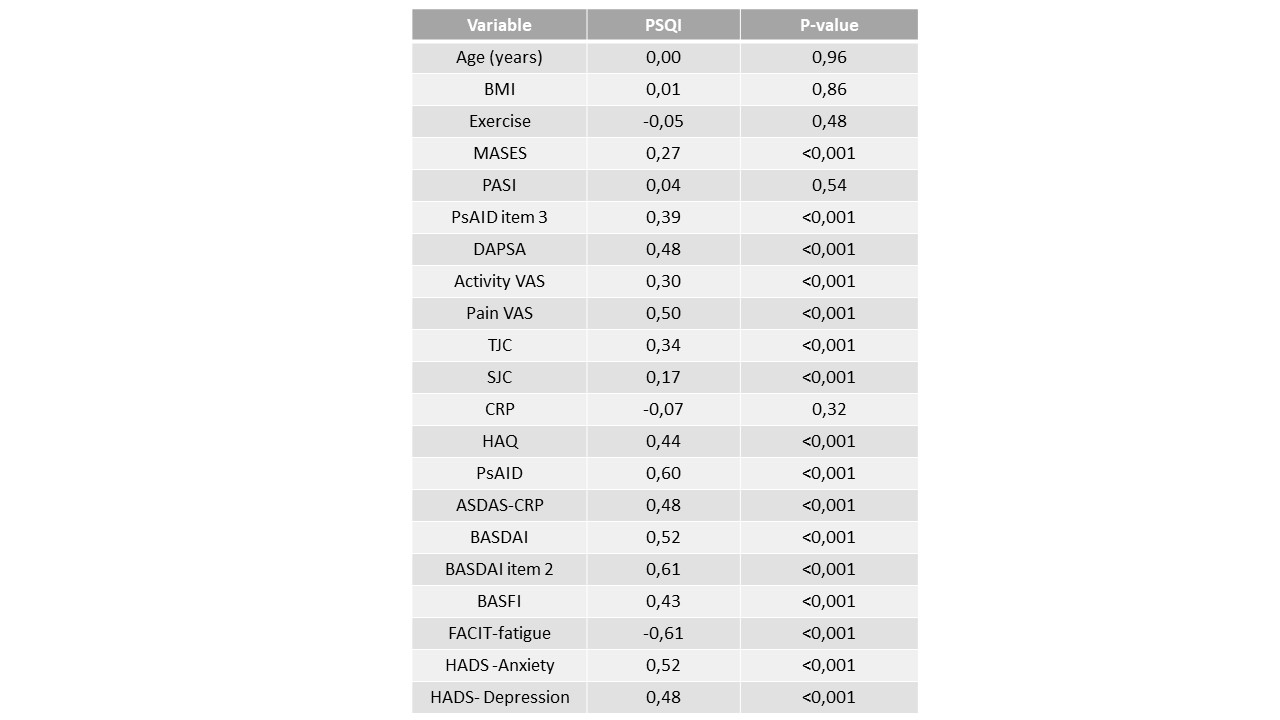 Correlation coefficients between the PSQI and demographic, clinical variables and PROs and index of disease activity, functionality, and impact.
Correlation coefficients between the PSQI and demographic, clinical variables and PROs and index of disease activity, functionality, and impact.Disclosures: M. Ibañez Martinez, None; S. Pastor Navarro, None; O. Compán Fernández, None; B. Miguel Ibáñez, None; A. Turrión Nieves, None; S. Gómez Castro, None; O. Martínez González, None; C. Hidalgo Calleja, None; E. Toledano Martinez, None; C. Montilla Morales, None.

