Back
Poster Session A
Vasculitis
Session: (0458–0497) Vasculitis – Non-ANCA-Associated and Related Disorders Poster I: Giant Cell Arteritis
0472: The Common Carotid Artery in the Ultrasound Evaluation of Giant Cell Arteritis
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- CO
Charles Oshinsky, MD, RhMSUS
Arthritis & Rheumatism Associates
Washington, District of Columbia, United States
Abstract Poster Presenter(s)
Charles Oshinsky1, Alison Bays1, Ingeborg Sacksen1, Elizabeth Jernberg2, R. Eugene zierler1 and Scott Pollock1, 1University of Washington, Seattle, WA, 2Virginia Mason, Seattle, WA
Background/Purpose: Giant cell arteritis (GCA), the most common large vessel vasculitis, can cause irreversible vision loss if untreated. Vascular ultrasound has been used with greater frequency to facilitate rapid, accurate diagnosis of GCA. Though the temporal arteries and its branches and the axillary arteries are commonly included in the ultrasound evaluation of GCA, the role of carotid artery ultrasonography remains unclear. Though the carotid artery may be affected in GCA and show typical changes of vasculitis, the carotid artery is a common site of atherosclerosis, a potential confounder, and the additional diagnostic value of the carotid ultrasound exam remains undefined. This study sought to determine whether ultrasound of the common carotid artery in addition to the temporal and axillary arteries improved diagnostic accuracy compared to ultrasound of the temporal and axillary arteries alone.
Methods: A fast track clinic (FTC) was formed at the University of Washington in November 2017 to rapidly evaluate patients referred for concern for GCA. All subjects received a vascular ultrasound for GCA. A positive ultrasound had either a temporal artery halo sign, or increased intima-media thickness (IMT) of a large vessel. The IMT cutoff used for the common carotid artery was 1.5 mm.
Results: 177 subjects referred to the FTC from November, 2017 – June, 2022 for concern for suspected GCA completed an ultrasound for GCA that included carotid ultrasound. 65 subjects were diagnosed with GCA by their rheumatologist. 48 subjects had positive ultrasound findings. 12 subjects diagnosed with GCA had positive common carotid artery ultrasounds, and of those 12, two subjects had isolated common carotid artery involvement without temporal or axillary involvement. One of these two subjects presented with vision loss and had a positive temporal artery biopsy. The other subject was diagnosed in the setting of elevated inflammatory markers and high clinical suspicion for GCA. Of the 112 subjects not diagnosed with GCA, 8 subjects had positive common carotid artery ultrasounds, and five of these eight subjects had isolated common carotid artery involvement without temporal or axillary involvement. These 8 subjects with positive common carotid artery ultrasounds who were not diagnosed with GCA were deemed unlikely to have GCA by their treating rheumatologist based on clinical grounds. The sensitivity of ultrasound of the temporal, axillary and common carotid arteries was 64.6% and specificity 89.2%. When evaluating just the temporal and axillary arteries without the common carotids, sensitivity was 61.5% and specificity was 93.8%. The positive predictive value of a positive carotid artery ultrasound in isolation with negative temporal and axillary findings was 28.6%.
Conclusion: Though common carotid artery ultrasound may rarely identify GCA in patients with otherwise normal temporal and axillary arteries, the positive predictive value for GCA of isolated common carotid artery changes is poor and more likely to represent a false positive in our cohort. Our data suggest that it is reasonable to exclude the common carotid artery ultrasound from the standard vascular ultrasound protocol when evaluating for GCA.
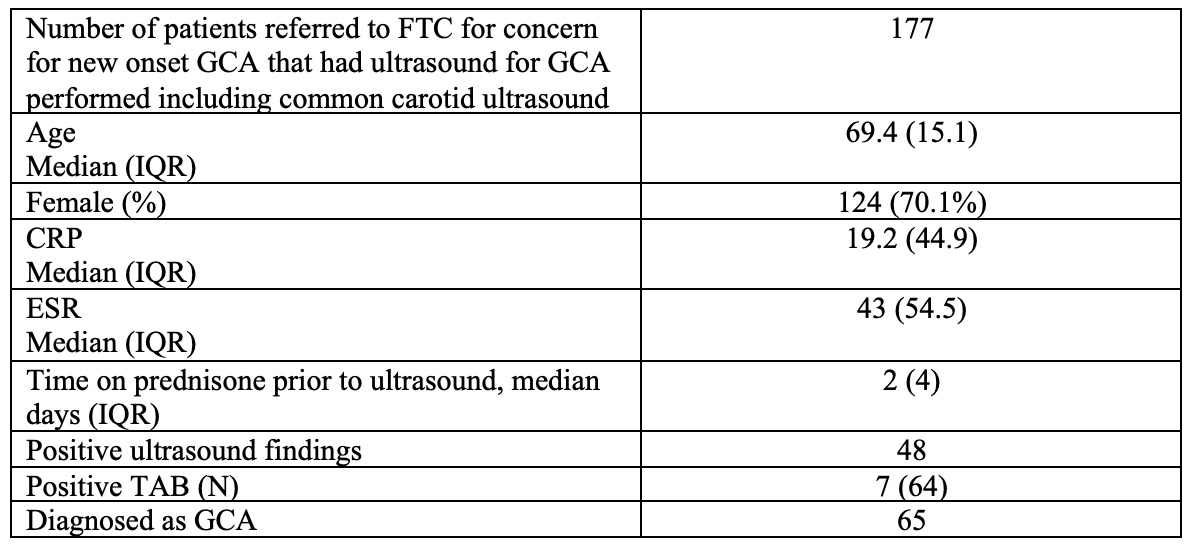 Demographic features of patients referred to the FTC for concern for new onset GCA between 11/2017 and 6/2022 that had ultrasound for GCA performed including common carotid ultrasound
Demographic features of patients referred to the FTC for concern for new onset GCA between 11/2017 and 6/2022 that had ultrasound for GCA performed including common carotid ultrasound
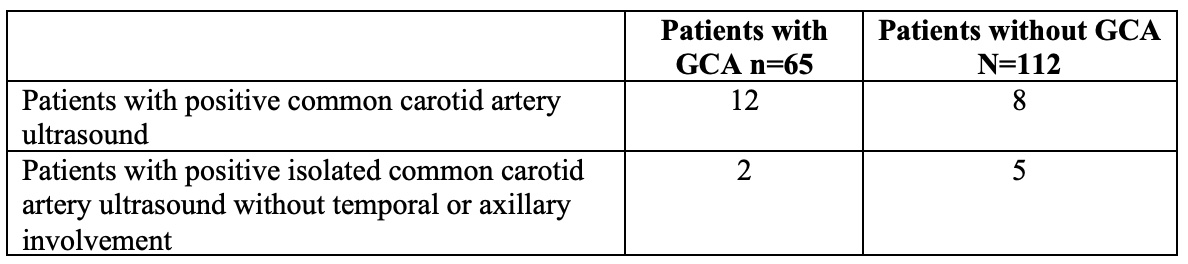 Vascular ultrasound features of patients referred to the FTC for new onset GCA between 11/2017 and 6/2022
Vascular ultrasound features of patients referred to the FTC for new onset GCA between 11/2017 and 6/2022
Disclosures: C. Oshinsky, None; A. Bays, None; I. Sacksen, None; E. Jernberg, None; R. zierler, None; S. Pollock, None.
Background/Purpose: Giant cell arteritis (GCA), the most common large vessel vasculitis, can cause irreversible vision loss if untreated. Vascular ultrasound has been used with greater frequency to facilitate rapid, accurate diagnosis of GCA. Though the temporal arteries and its branches and the axillary arteries are commonly included in the ultrasound evaluation of GCA, the role of carotid artery ultrasonography remains unclear. Though the carotid artery may be affected in GCA and show typical changes of vasculitis, the carotid artery is a common site of atherosclerosis, a potential confounder, and the additional diagnostic value of the carotid ultrasound exam remains undefined. This study sought to determine whether ultrasound of the common carotid artery in addition to the temporal and axillary arteries improved diagnostic accuracy compared to ultrasound of the temporal and axillary arteries alone.
Methods: A fast track clinic (FTC) was formed at the University of Washington in November 2017 to rapidly evaluate patients referred for concern for GCA. All subjects received a vascular ultrasound for GCA. A positive ultrasound had either a temporal artery halo sign, or increased intima-media thickness (IMT) of a large vessel. The IMT cutoff used for the common carotid artery was 1.5 mm.
Results: 177 subjects referred to the FTC from November, 2017 – June, 2022 for concern for suspected GCA completed an ultrasound for GCA that included carotid ultrasound. 65 subjects were diagnosed with GCA by their rheumatologist. 48 subjects had positive ultrasound findings. 12 subjects diagnosed with GCA had positive common carotid artery ultrasounds, and of those 12, two subjects had isolated common carotid artery involvement without temporal or axillary involvement. One of these two subjects presented with vision loss and had a positive temporal artery biopsy. The other subject was diagnosed in the setting of elevated inflammatory markers and high clinical suspicion for GCA. Of the 112 subjects not diagnosed with GCA, 8 subjects had positive common carotid artery ultrasounds, and five of these eight subjects had isolated common carotid artery involvement without temporal or axillary involvement. These 8 subjects with positive common carotid artery ultrasounds who were not diagnosed with GCA were deemed unlikely to have GCA by their treating rheumatologist based on clinical grounds. The sensitivity of ultrasound of the temporal, axillary and common carotid arteries was 64.6% and specificity 89.2%. When evaluating just the temporal and axillary arteries without the common carotids, sensitivity was 61.5% and specificity was 93.8%. The positive predictive value of a positive carotid artery ultrasound in isolation with negative temporal and axillary findings was 28.6%.
Conclusion: Though common carotid artery ultrasound may rarely identify GCA in patients with otherwise normal temporal and axillary arteries, the positive predictive value for GCA of isolated common carotid artery changes is poor and more likely to represent a false positive in our cohort. Our data suggest that it is reasonable to exclude the common carotid artery ultrasound from the standard vascular ultrasound protocol when evaluating for GCA.
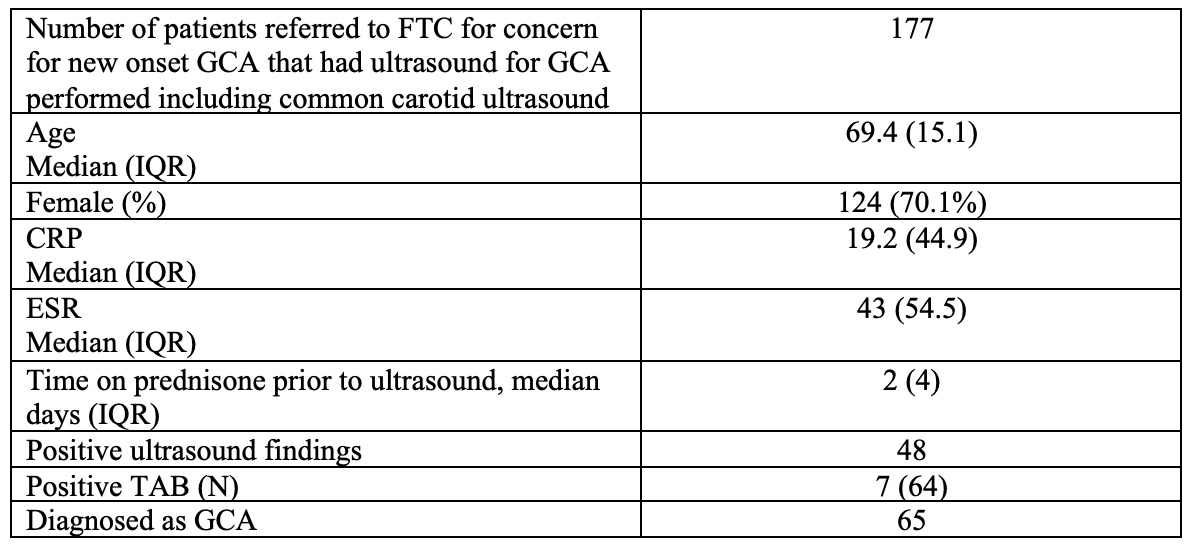 Demographic features of patients referred to the FTC for concern for new onset GCA between 11/2017 and 6/2022 that had ultrasound for GCA performed including common carotid ultrasound
Demographic features of patients referred to the FTC for concern for new onset GCA between 11/2017 and 6/2022 that had ultrasound for GCA performed including common carotid ultrasound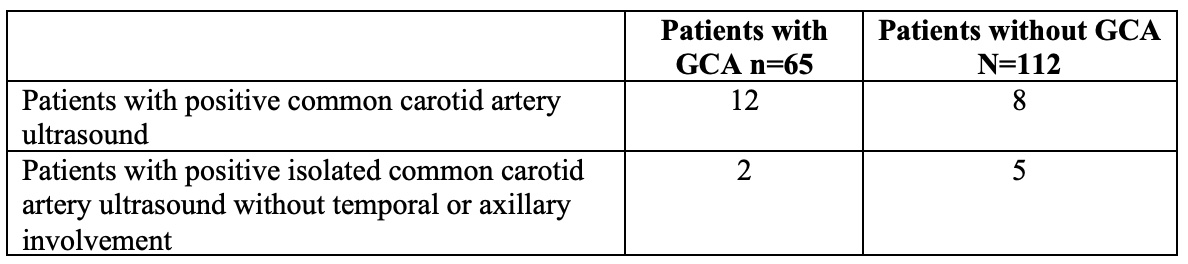 Vascular ultrasound features of patients referred to the FTC for new onset GCA between 11/2017 and 6/2022
Vascular ultrasound features of patients referred to the FTC for new onset GCA between 11/2017 and 6/2022Disclosures: C. Oshinsky, None; A. Bays, None; I. Sacksen, None; E. Jernberg, None; R. zierler, None; S. Pollock, None.

