Back
Poster Session A
Professional development and education
Session: (0214–0240) Professional Education Poster
0236: What Ultrasound Skills Can Be Learned Before Laying Hands on a Probe? Results of a Pilot Study of a Hybrid Online and in Person Curriculum to Teach Rheumatology Focused Knee Ultrasonography Skills to Internal Medicine Residents
Saturday, November 12, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- AL
Andrew Long, MD
University of Rochester Medical Center
Rochester, NY, United States
Abstract Poster Presenter(s)
Andrew Long1, Norman Madsen2, William Novak1, Homaira Rahimi3 and Bethany Marston3, 1University of Rochester Medical Center, Rochester, NY, 2University of Rochester, NY, Rochester, NY, 3University of Rochester, Rochester, NY
Background/Purpose: Developing competence in musculoskeletal point of care ultrasound (MSK POCUS) involves mastery of 3 key domains: image acquisition, image interpretation, and incorporation of findings into clinical decision making. Hands-on experiential learning is essential for the development of competence, but other teaching methodologies including interactive self-teaching tools have gained popularity in recent years in the context of the COVID-19 pandemic. Little is known regarding the extent of mastery that can be obtained through the use of such tools in each key competence domain or whether mastery of each domain is interdependent on mastery of the others. We have previously shown that a self-directed web-based module may improve skills in interpreting knee US pathology. Here, we present results from a pilot cohort of internal medicine residents who completed a hybrid online and in person knee US curriculum.
Methods: 5 primary care track internal medicine residents were assigned a web-based module we designed to teach 3 US views of the knee, including transducer placement, normal anatomy, and common pathology in each view. US physics, pertinent artifacts, and indications for MSK POCUS are also featured. Residents then participated in a single hands-on scanning session with an MSK ultrasound trained instructor. Residents were assessed with an online pre and post-test after module completion followed by an observed structured clinical examination (OSCE) during which they were asked to reproduce the 3 protocol views on a standardized patient model and take a written test with items assessing each of the 3 key competency domains for mastery of MSK POCUS. A survey gauging prior US exposure, confidence in performing the protocol following each component of the curriculum, and satisfaction with the course was also administered.
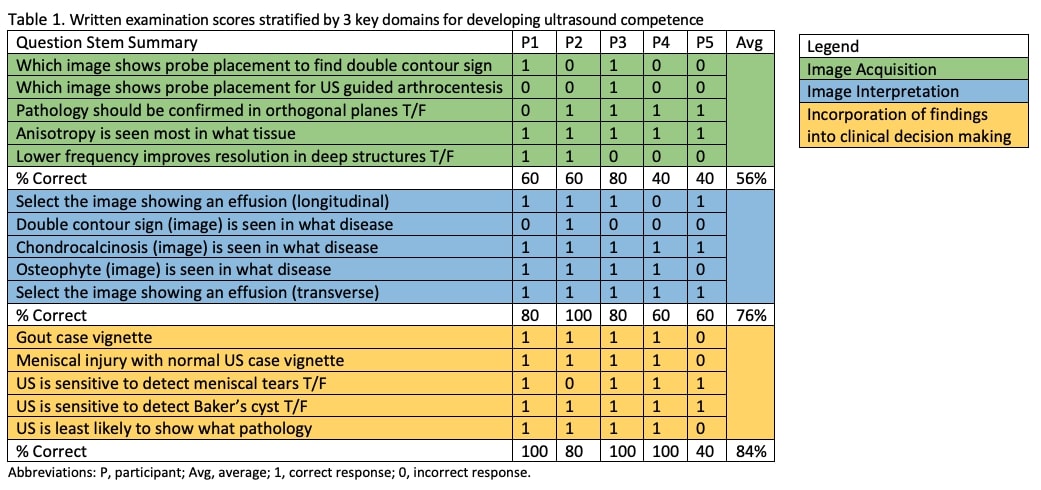
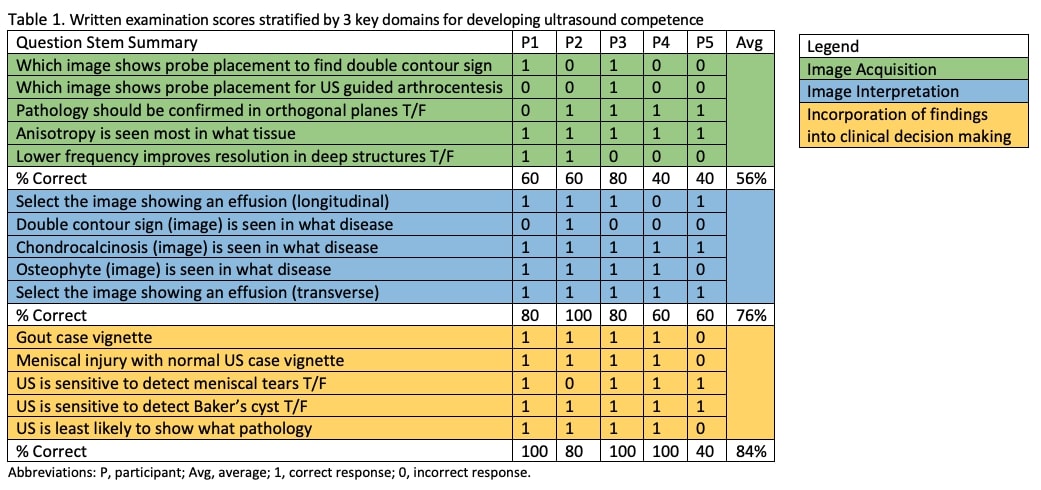
Results: Module post-test data show that 4/5 residents were able to accurately identify images showing effusion, OA, the double contour sign of gout, and chondrocalcinosis while none could identify pathology prior to completing the module. None of the residents were able to produce interpretable images in all 3 protocol views. Written exam scores ranged from 46.7% to 86.7% with an average score of 72%. Analysis of results in each of the 3 key competency domains showed average scores of 56% for image acquisition, 76% for image interpretation, and 84% for incorporation of findings into clinical decision making (Table 1). 4/5 residents indicated they found the curriculum useful for clinical practice and all indicated they would like to take additional web-based instructional modules for MSK POCUS training in future.
Conclusion: The inability of residents to produce interpretable images from our 3 view US protocol of the knee following this brief curriculum suggests there is a minimum threshold of hands-on experience needed to obtain images that was not reached by this cohort. Results of the web-based module and written exam provide further evidence that image interpretation skills may be learned independent of image acquisition skills.
Disclosures: A. Long, None; N. Madsen, None; W. Novak, None; H. Rahimi, None; B. Marston, None.
Background/Purpose: Developing competence in musculoskeletal point of care ultrasound (MSK POCUS) involves mastery of 3 key domains: image acquisition, image interpretation, and incorporation of findings into clinical decision making. Hands-on experiential learning is essential for the development of competence, but other teaching methodologies including interactive self-teaching tools have gained popularity in recent years in the context of the COVID-19 pandemic. Little is known regarding the extent of mastery that can be obtained through the use of such tools in each key competence domain or whether mastery of each domain is interdependent on mastery of the others. We have previously shown that a self-directed web-based module may improve skills in interpreting knee US pathology. Here, we present results from a pilot cohort of internal medicine residents who completed a hybrid online and in person knee US curriculum.
Methods: 5 primary care track internal medicine residents were assigned a web-based module we designed to teach 3 US views of the knee, including transducer placement, normal anatomy, and common pathology in each view. US physics, pertinent artifacts, and indications for MSK POCUS are also featured. Residents then participated in a single hands-on scanning session with an MSK ultrasound trained instructor. Residents were assessed with an online pre and post-test after module completion followed by an observed structured clinical examination (OSCE) during which they were asked to reproduce the 3 protocol views on a standardized patient model and take a written test with items assessing each of the 3 key competency domains for mastery of MSK POCUS. A survey gauging prior US exposure, confidence in performing the protocol following each component of the curriculum, and satisfaction with the course was also administered.
Results: Module post-test data show that 4/5 residents were able to accurately identify images showing effusion, OA, the double contour sign of gout, and chondrocalcinosis while none could identify pathology prior to completing the module. None of the residents were able to produce interpretable images in all 3 protocol views. Written exam scores ranged from 46.7% to 86.7% with an average score of 72%. Analysis of results in each of the 3 key competency domains showed average scores of 56% for image acquisition, 76% for image interpretation, and 84% for incorporation of findings into clinical decision making (Table 1). 4/5 residents indicated they found the curriculum useful for clinical practice and all indicated they would like to take additional web-based instructional modules for MSK POCUS training in future.
Conclusion: The inability of residents to produce interpretable images from our 3 view US protocol of the knee following this brief curriculum suggests there is a minimum threshold of hands-on experience needed to obtain images that was not reached by this cohort. Results of the web-based module and written exam provide further evidence that image interpretation skills may be learned independent of image acquisition skills.
Disclosures: A. Long, None; N. Madsen, None; W. Novak, None; H. Rahimi, None; B. Marston, None.

