Back
Poster Session D
Systemic lupus erythematosus (SLE)
Session: (1707–1726) SLE – Animal Models Poster
1717: Deficiency of IL-23 Receptor in Podocytes of MRL/lpr lupus-prone Mice Abrogates the Development of Lupus Nephritis Despite IgG Deposition in the Glomeruli
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- AB
Afroditi Boulougoura, MD
Beth Israel Deaconess Medical Center
Allston, MA, United States
Abstract Poster Presenter(s)
Afroditi Boulougoura1, Hao Li1, Rhea Bhargava1, Wenliang Pan1, Abhigyan Satyam1, Isaac Stillman2 and George Tsokos1, 1Division of Rheumatology and Clinical Immunology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, 2Department of Pathology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
Background/Purpose: Interleukin 23 (IL-23) is involved in the pathogenesis of systemic lupus erythematosus (SLE). IL-23 is elevated in the sera of patients with active SLE compared to those with inactive disease and it induces the expansion of pathogenic IL-17-producing cells which infiltrate inflamed tissues including the kidneys. However, there are still limited data on the role of IL-23 on nonhematopoietic kidney resident cells. We hypothesized that the expression of IL-23 receptor (R) will be increased in the podocytes of patients with active lupus nephritis (LN) and that deficiency of IL-23R only in podocytes of lupus-prone MRL/lpr mice, should ameliorate the pathology associated with LN.
Methods: Kidney biopsies of patients with LN (3 active and 3 in remission) were immunostained for IL-23R. We generated podocyte-specific IL-23R conditionally deficient mice on the lupus-prone MRL/lpr mouse using the Cre-loxP system. Mice harboring loxP sites of IL-23R gene (IL23R flox/flox) were crossed with Cre transgenic mice driven by the human podocin (NPHS2) promoter/enhancer region. Mice were sacrificed at 21 weeks of age. Serum, urine, kidneys and spleens were collected. Kidneys were stained with hematoxylin and eosin, examined microscopically in a blinded manner by using the renal activity index score (scores range from 0 to 16). Levels of double-stranded DNA antibodies were measured by ELISA. Proteinuria was assessed by albumin to creatinine ratio. Frozen kidney sections were fixed in acetone, stained for IL-23R, IgG, and Calcium/calmodulin kinase IV (CaMK4) and analyzed using a confocal microscope. Fluorescence intensities were measured by ImageJ software. T- test was used for statistical analysis and data are expressed as mean±SD.
Results: IL-23R expression was increased in the glomeruli of patients with active LN compared to those in remission (29.0± 8.1 vs. 5.2 ± 6.1, p= 0.029). MRL/lpr.Podo-Cre + IL-23R f/f mice had significantly decreased glomerular crescent formation, lymphocytic infiltration, tubular changes and perivascular infiltrates in the kidney parenchyma compared to MRL/lpr.Podo-Cre - IL23R f/f mice (score 4 vs. 20.5 respectively). MRL/lpr.Podo-Cre + IL-23R f/f mice had less ptoteinuria compered to their controls (82± 4 vs. 335± 32 μg/mg). The level of dsDNA antibodies and the spleen size were similar in the two groups. As expected, confocal immunofluorescence studies in the kidney biopsies of MRL/lpr.Podo-Cre - IL23R f/f mice had increased IgG deposition and expression of CaMK4, that has been linked previously to podocyte injury. Unexpectedly, MRL/lpr.Podo-Cre + IL-23R f/f, had significant IgG deposition in the glomeruli but decreased CaMK4 expression (Fig.1). Electron microscopy showed less subendothelial electron dense deposits, normal foot processes, reduced mesangial cell proliferation and membrane thickening (Fig.1).
Conclusion: IL-23R is significantly increased in the kidneys of patients with active LN compared to those with inactive disease. Deficiency of IL-23R specifically in podocytes of the lupus-prone MRL/lpr mouse, although it did not affect the peripheral autoimmunity, it abrogates the development of LN, despite the fact that IgG was deposited in the glomeruli.
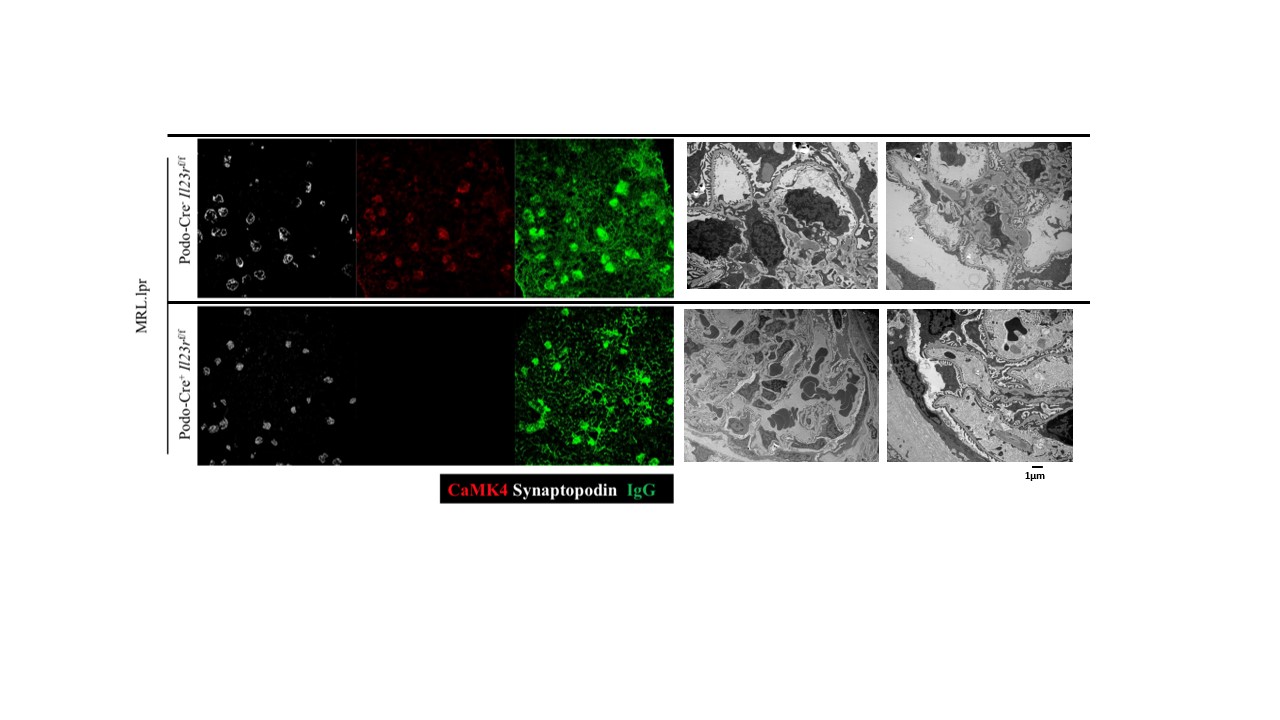 Fig. 1. Immunofluorescent staining (left) and electron microscopy study (right) of glomeruli of MRL/lpr.Podo-Cre negative IL23R f/f mice (top row) and MRL/lpr. Podo-Cre positive IL-23R f/f mice (bottom row).
Fig. 1. Immunofluorescent staining (left) and electron microscopy study (right) of glomeruli of MRL/lpr.Podo-Cre negative IL23R f/f mice (top row) and MRL/lpr. Podo-Cre positive IL-23R f/f mice (bottom row).
Disclosures: A. Boulougoura, None; H. Li, None; R. Bhargava, None; W. Pan, None; A. Satyam, None; I. Stillman, None; G. Tsokos, None.
Background/Purpose: Interleukin 23 (IL-23) is involved in the pathogenesis of systemic lupus erythematosus (SLE). IL-23 is elevated in the sera of patients with active SLE compared to those with inactive disease and it induces the expansion of pathogenic IL-17-producing cells which infiltrate inflamed tissues including the kidneys. However, there are still limited data on the role of IL-23 on nonhematopoietic kidney resident cells. We hypothesized that the expression of IL-23 receptor (R) will be increased in the podocytes of patients with active lupus nephritis (LN) and that deficiency of IL-23R only in podocytes of lupus-prone MRL/lpr mice, should ameliorate the pathology associated with LN.
Methods: Kidney biopsies of patients with LN (3 active and 3 in remission) were immunostained for IL-23R. We generated podocyte-specific IL-23R conditionally deficient mice on the lupus-prone MRL/lpr mouse using the Cre-loxP system. Mice harboring loxP sites of IL-23R gene (IL23R flox/flox) were crossed with Cre transgenic mice driven by the human podocin (NPHS2) promoter/enhancer region. Mice were sacrificed at 21 weeks of age. Serum, urine, kidneys and spleens were collected. Kidneys were stained with hematoxylin and eosin, examined microscopically in a blinded manner by using the renal activity index score (scores range from 0 to 16). Levels of double-stranded DNA antibodies were measured by ELISA. Proteinuria was assessed by albumin to creatinine ratio. Frozen kidney sections were fixed in acetone, stained for IL-23R, IgG, and Calcium/calmodulin kinase IV (CaMK4) and analyzed using a confocal microscope. Fluorescence intensities were measured by ImageJ software. T- test was used for statistical analysis and data are expressed as mean±SD.
Results: IL-23R expression was increased in the glomeruli of patients with active LN compared to those in remission (29.0± 8.1 vs. 5.2 ± 6.1, p= 0.029). MRL/lpr.Podo-Cre + IL-23R f/f mice had significantly decreased glomerular crescent formation, lymphocytic infiltration, tubular changes and perivascular infiltrates in the kidney parenchyma compared to MRL/lpr.Podo-Cre - IL23R f/f mice (score 4 vs. 20.5 respectively). MRL/lpr.Podo-Cre + IL-23R f/f mice had less ptoteinuria compered to their controls (82± 4 vs. 335± 32 μg/mg). The level of dsDNA antibodies and the spleen size were similar in the two groups. As expected, confocal immunofluorescence studies in the kidney biopsies of MRL/lpr.Podo-Cre - IL23R f/f mice had increased IgG deposition and expression of CaMK4, that has been linked previously to podocyte injury. Unexpectedly, MRL/lpr.Podo-Cre + IL-23R f/f, had significant IgG deposition in the glomeruli but decreased CaMK4 expression (Fig.1). Electron microscopy showed less subendothelial electron dense deposits, normal foot processes, reduced mesangial cell proliferation and membrane thickening (Fig.1).
Conclusion: IL-23R is significantly increased in the kidneys of patients with active LN compared to those with inactive disease. Deficiency of IL-23R specifically in podocytes of the lupus-prone MRL/lpr mouse, although it did not affect the peripheral autoimmunity, it abrogates the development of LN, despite the fact that IgG was deposited in the glomeruli.
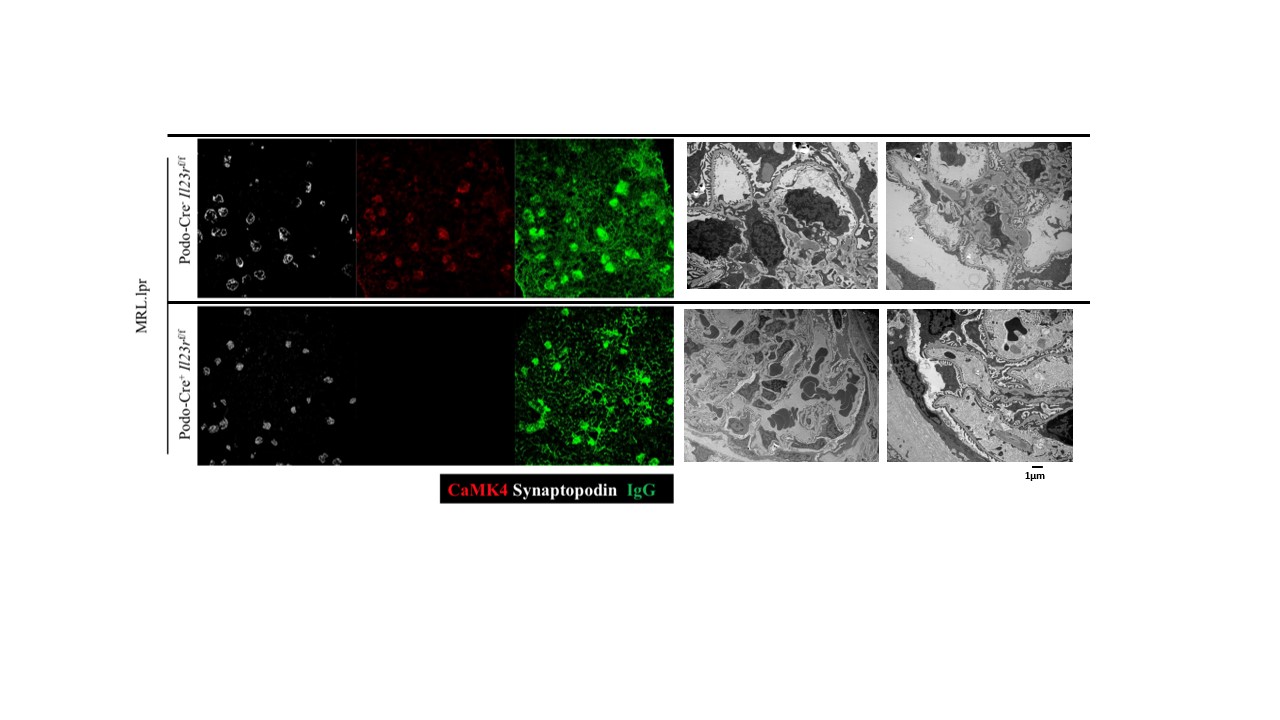 Fig. 1. Immunofluorescent staining (left) and electron microscopy study (right) of glomeruli of MRL/lpr.Podo-Cre negative IL23R f/f mice (top row) and MRL/lpr. Podo-Cre positive IL-23R f/f mice (bottom row).
Fig. 1. Immunofluorescent staining (left) and electron microscopy study (right) of glomeruli of MRL/lpr.Podo-Cre negative IL23R f/f mice (top row) and MRL/lpr. Podo-Cre positive IL-23R f/f mice (bottom row).Disclosures: A. Boulougoura, None; H. Li, None; R. Bhargava, None; W. Pan, None; A. Satyam, None; I. Stillman, None; G. Tsokos, None.

