Back
Abstract Session
Osteoarthritis (OA) and related disorders
Session: Abstracts: Orthopedics, Low Back Pain, and Rehabilitation (0503–0505)
0503: The Effect of Social Isolation on 1-Year Outcomes After Surgical Repair of Low Trauma Hip Fracture
Saturday, November 12, 2022
3:00 PM – 3:10 PM Eastern Time
Location: Room 122
- RL
Robyn Lipschultz, BA
New York University Grossman School of Medicine
New York, NY, United States
Presenting Author(s)
Robyn Lipschultz1, Dina Sheira1, Marianna Frey2, Mangala Rajan3, Joseph Lane1 and Lisa Mandl1, 1Hospital for Special Surgery, New York, NY, 2University of Rochester School of Medicine and Dentistry, New York, NY, 3Weill Cornell Medicine, New York, NY
Background/Purpose: Hip fractures are a serious public health issue with a significant population burden, especially among those over 65 years old. Social isolation—how integrated a patient is into their community—is a novel and potentially modifiable risk factor for poor health outcomes after low trauma hip fracture. This study evaluates the association of pre-operative social isolation with patient-reported functional recovery in elderly patients 1 year after surgical repair of low-trauma hip fracture.
Methods: Patients ≥ 65 years at a single center who underwent surgical repair of a low trauma hip fracture were enrolled. Patients with active cancer, dementia, previous or bilateral hip fracture, or a non-U.S. address were excluded. Patient reported outcomes (PROMs) including the Lubben Social Networks Scale, a validated instrument designed to measure social isolation in the elderly, PROMIS-29, and the Lower Extremity Activity Scale (LEAS), were asked 2-4 days post-operatively to assess pre-fracture status, and then again 1-year later. A Lubben score of 36 is considered socially isolated. Multivariable exact logistic regression was used to generate estimates of association between pre-operative social isolation and outcomes at 1 year. Multivariable linear models, controlling for age, sex, education, and BMI were performed separately for each outcome of interest.
Results: 325 patients were enrolled: 1 died and 4 withdrew before submitting data. Mean age 81.0 years (SD: 8.2), 70.9 % female, 85.9% white, 65.9% finished college or more. 31.6% of patients enrolled were socially isolated at time of fracture (Table 1). 291/320 (90.9%) were confirmed alive at 1 year; 20 died, 9 lost to follow up. Of those confirmed alive, 29 withdrew, 31 could not be reached at home/assisted living, 9 were too cognitively impaired to respond. The remaining 222/291 (76.2%) provided 1-year PROMs. Controlling for age, sex, education, and BMI, those who were socially isolated at time of fracture had significantly worse function, (β= -3.83 p= 0.0012) ability to participate in social roles (β= -4.84 p= 0.0002) and depression (β= 2.32 p= 0.0.461) at time of fracture (Table 2). Similar multivariable models showed that being socially isolated was significantly associated with clinically meaningfully worse function (β= -8.02 p= 0.0003) and ability to participate in social roles (β= -9.79 p= 0.0002) at 1 year.
Conclusion: Being socially isolated at the time of first low trauma hip fracture is associated with worse function and social participation 1 year later. Given the dearth of modifiable risk factors in elderly hip fracture patients, future studies are needed to evaluate whether improving social connections could improve outcomes in this rapidly growing demographic.
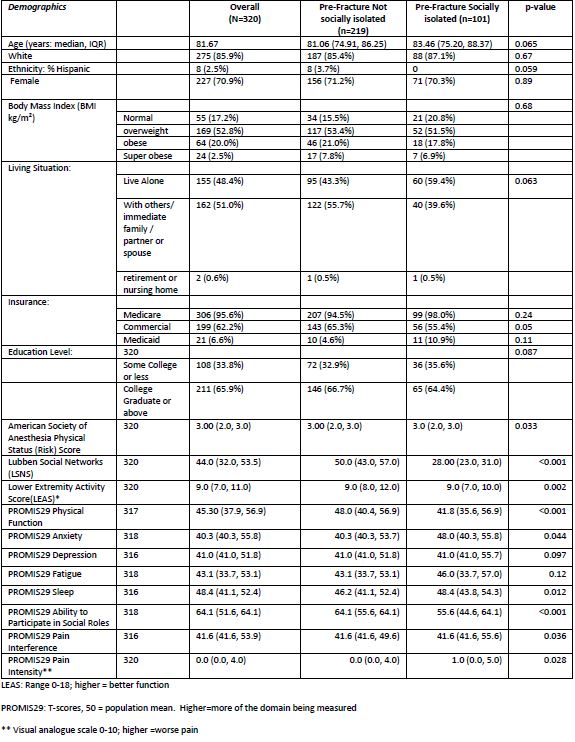 Table 1: Baseline Characteristics and Patient Reported Outcome Measures (PROMs) Stratified on Social Isolation
Table 1: Baseline Characteristics and Patient Reported Outcome Measures (PROMs) Stratified on Social Isolation
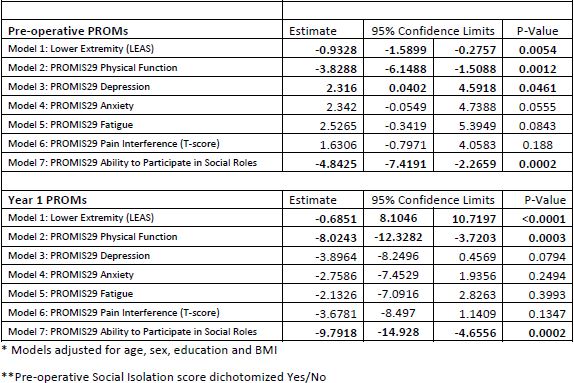 Table 2: Association of Pre-Operative Social Isolation with Patient-Reported Outcome Measures (PROMs)
Table 2: Association of Pre-Operative Social Isolation with Patient-Reported Outcome Measures (PROMs)
Disclosures: R. Lipschultz, None; D. Sheira, None; M. Frey, None; M. Rajan, None; J. Lane, None; L. Mandl, Pfizer.
Background/Purpose: Hip fractures are a serious public health issue with a significant population burden, especially among those over 65 years old. Social isolation—how integrated a patient is into their community—is a novel and potentially modifiable risk factor for poor health outcomes after low trauma hip fracture. This study evaluates the association of pre-operative social isolation with patient-reported functional recovery in elderly patients 1 year after surgical repair of low-trauma hip fracture.
Methods: Patients ≥ 65 years at a single center who underwent surgical repair of a low trauma hip fracture were enrolled. Patients with active cancer, dementia, previous or bilateral hip fracture, or a non-U.S. address were excluded. Patient reported outcomes (PROMs) including the Lubben Social Networks Scale, a validated instrument designed to measure social isolation in the elderly, PROMIS-29, and the Lower Extremity Activity Scale (LEAS), were asked 2-4 days post-operatively to assess pre-fracture status, and then again 1-year later. A Lubben score of 36 is considered socially isolated. Multivariable exact logistic regression was used to generate estimates of association between pre-operative social isolation and outcomes at 1 year. Multivariable linear models, controlling for age, sex, education, and BMI were performed separately for each outcome of interest.
Results: 325 patients were enrolled: 1 died and 4 withdrew before submitting data. Mean age 81.0 years (SD: 8.2), 70.9 % female, 85.9% white, 65.9% finished college or more. 31.6% of patients enrolled were socially isolated at time of fracture (Table 1). 291/320 (90.9%) were confirmed alive at 1 year; 20 died, 9 lost to follow up. Of those confirmed alive, 29 withdrew, 31 could not be reached at home/assisted living, 9 were too cognitively impaired to respond. The remaining 222/291 (76.2%) provided 1-year PROMs. Controlling for age, sex, education, and BMI, those who were socially isolated at time of fracture had significantly worse function, (β= -3.83 p= 0.0012) ability to participate in social roles (β= -4.84 p= 0.0002) and depression (β= 2.32 p= 0.0.461) at time of fracture (Table 2). Similar multivariable models showed that being socially isolated was significantly associated with clinically meaningfully worse function (β= -8.02 p= 0.0003) and ability to participate in social roles (β= -9.79 p= 0.0002) at 1 year.
Conclusion: Being socially isolated at the time of first low trauma hip fracture is associated with worse function and social participation 1 year later. Given the dearth of modifiable risk factors in elderly hip fracture patients, future studies are needed to evaluate whether improving social connections could improve outcomes in this rapidly growing demographic.
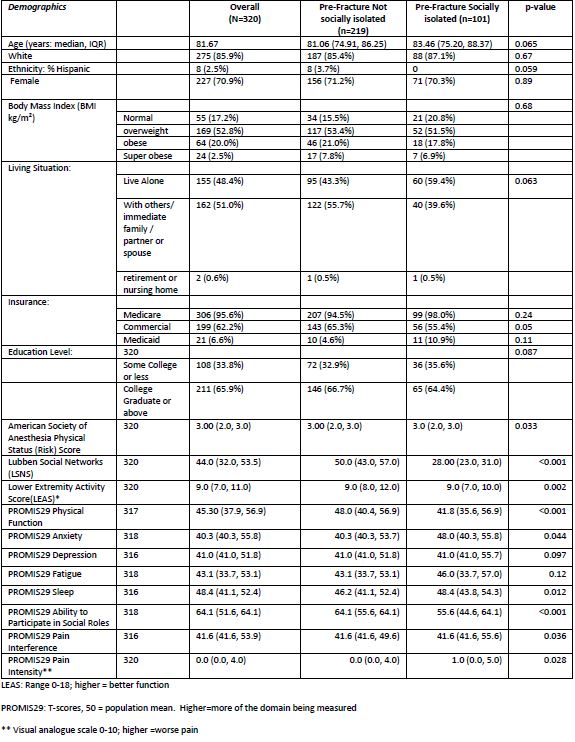 Table 1: Baseline Characteristics and Patient Reported Outcome Measures (PROMs) Stratified on Social Isolation
Table 1: Baseline Characteristics and Patient Reported Outcome Measures (PROMs) Stratified on Social Isolation 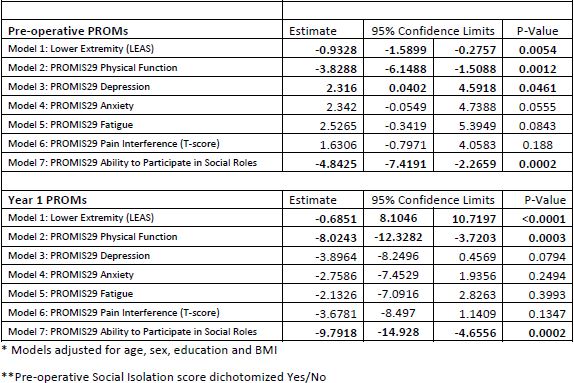 Table 2: Association of Pre-Operative Social Isolation with Patient-Reported Outcome Measures (PROMs)
Table 2: Association of Pre-Operative Social Isolation with Patient-Reported Outcome Measures (PROMs)Disclosures: R. Lipschultz, None; D. Sheira, None; M. Frey, None; M. Rajan, None; J. Lane, None; L. Mandl, Pfizer.

