Back
Poster Session D
Myopathic rheumatic diseases (polymyositis, dermatomyositis, inclusion body myositis)
Session: (1856–1887) Muscle Biology, Myositis and Myopathies Poster II
1857: Increasing Proportion of MDA-5 Associated Conditions in a Tertiary Myositis Centre Following Onset of the Covid-19 Pandemic
Monday, November 14, 2022
1:00 PM – 3:00 PM Eastern Time
Location: Virtual Poster Hall
- JH
Jennifer Hannah, MBBS, MSc, MRCP, MA
Kings College London
Sutton, United Kingdom
Abstract Poster Presenter(s)
Jennifer Hannah1, Saadia Sasha Ali1, Sloni Arora1, John Cazabon1, James Galloway1 and Patrick Gordon2, 1King's College London, London, United Kingdom, 2King’s College Hospital NHS Foundation Trust, London, United Kingdom
Background/Purpose: Anti-MDA5 dermatomyositis is a clinical subtype of DM that is strongly associated with a rapidly progressive phenotype of interstitial lung disease resulting in a high morbidity and mortality. MDA5 is an intracellular sensor of viral RNA that triggers an innate immune response in the healthy host important in upregulating a type1-IFN response. Viral infections have been considered as a possible trigger for anti-MDA5 DM and case reports have linked Covid 19 infection and Covid-19 vaccination with the subsequent development of anti-MDA5 DM. (Gonzalez et al, 2022) One study showed that Anti-MDA5 antibodies were prevalent in COVID 19 patients, and a higher titre of the antibody was associated with unfavourable outcomes. (Wang et al, 2021). Our aim was to assess whether the incidence of Anti-MDA5 DM increased following the onset of the Covid 19 pandemic at our large tertiary myositis centre.
Methods: A retrospective analysis of all myositis specific antibody tests was performed at King's College Hospital between January 2017 and April 2022 as part of a service usage evaluation. Inclusion criteria included a positive MDA-5 antibody on myositis blot ( >6 units as per manufacturer guidelines) or positive immunoprecipitation result. In the instance of multiple tests on the same patient the earliest result was used. The rate at which MDA-5 Ab was detected and trends over time was analysed using logistic regression and two-sample test of proportions to compare rates prior to the pandemic and subsequently using date Covid-19 first described in UK as 29th/Jan/2020.
Results: 2,627 patients underwent extended nuclear antigen myositis blot or immunoprecipitation. There has been a slight increase in the number of tests performed over time. There was a fall in testing immediately at the beginning of the pandemic, but this has returned to pre-pandemic levels (Graph 1). Pre-pandemic an average 480 tests per year were carried out, compared to 518 tests per year since. The total proportion of patients testing positive for any MSA or MAA was 38.28% and is not significantly different between pre and post pandemic (37.25% vs 39.62% p=0.22).
Overall, 1.67% of samples test positive for MDA5 (n=44). Pre-pandemic 1.15% were MDA5 positive, compared to 2.23% since (p=0.021 by two-sample test of proportions) (Table 1). Graph 2 shows changing pattern over time. Proportion of MDA5 positive tests has increased by a co-efficient of 0.0049 (95%CI 0.0016-0.0082) per year with test for trend p=0.01.
Conclusion: Despite the dramatic fall in testing during the peak of the pandemic, just over 2 years later antibody testing is increasing at this tertiary centre again, with a higher burden of disease being anti-MDA-5 positive than prior to the pandemic. Given MDA-5 is associated with worse outcomes in idiopathic inflammatory myopathies and a higher burden of interstitial lung disease, further research is warranted to elucidate the clinical relevance of increasing presence of anti-MDA5 and identify if Covid-19 infection or vaccination could be a trigger for this disease.
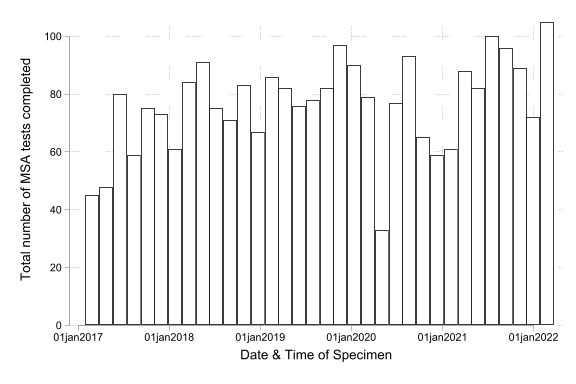 Graph 1. Histogram showing number of MSA tests reported over duration of study
Graph 1. Histogram showing number of MSA tests reported over duration of study
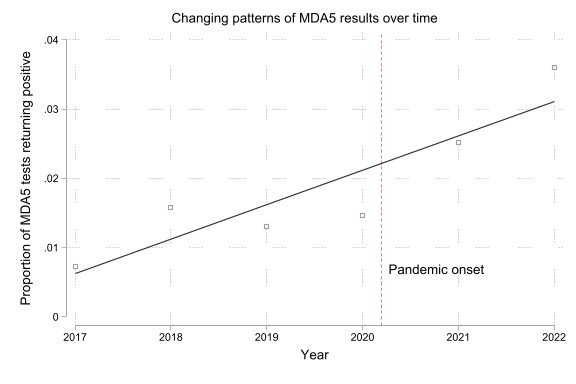 Graph 2. Proportion of MSA tests showing a positive MDA-5 result over time with dotted line demonstrating time pandemic onset
Graph 2. Proportion of MSA tests showing a positive MDA-5 result over time with dotted line demonstrating time pandemic onset
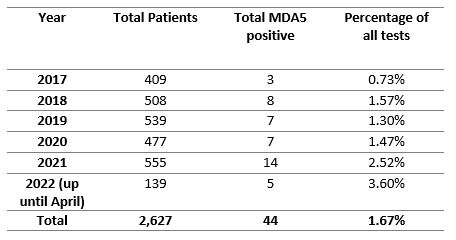 Table 1. Table showing number of MDA5 positive patients per year since 2017. Note that 2022 results only include test up to 31/Mar/2022
Table 1. Table showing number of MDA5 positive patients per year since 2017. Note that 2022 results only include test up to 31/Mar/2022
Disclosures: J. Hannah, None; S. Ali, None; S. Arora, None; J. Cazabon, None; J. Galloway, AbbVie, AstraZeneca, Biogen, Celgene, Galapagos, Gilead, Janssen, Medicago, Lilly, Novartis, Novavax, Pfizer, Roche, UCB; P. Gordon, Eli Lilly, UCB, Corbus, Galapagos.
Background/Purpose: Anti-MDA5 dermatomyositis is a clinical subtype of DM that is strongly associated with a rapidly progressive phenotype of interstitial lung disease resulting in a high morbidity and mortality. MDA5 is an intracellular sensor of viral RNA that triggers an innate immune response in the healthy host important in upregulating a type1-IFN response. Viral infections have been considered as a possible trigger for anti-MDA5 DM and case reports have linked Covid 19 infection and Covid-19 vaccination with the subsequent development of anti-MDA5 DM. (Gonzalez et al, 2022) One study showed that Anti-MDA5 antibodies were prevalent in COVID 19 patients, and a higher titre of the antibody was associated with unfavourable outcomes. (Wang et al, 2021). Our aim was to assess whether the incidence of Anti-MDA5 DM increased following the onset of the Covid 19 pandemic at our large tertiary myositis centre.
Methods: A retrospective analysis of all myositis specific antibody tests was performed at King's College Hospital between January 2017 and April 2022 as part of a service usage evaluation. Inclusion criteria included a positive MDA-5 antibody on myositis blot ( >6 units as per manufacturer guidelines) or positive immunoprecipitation result. In the instance of multiple tests on the same patient the earliest result was used. The rate at which MDA-5 Ab was detected and trends over time was analysed using logistic regression and two-sample test of proportions to compare rates prior to the pandemic and subsequently using date Covid-19 first described in UK as 29th/Jan/2020.
Results: 2,627 patients underwent extended nuclear antigen myositis blot or immunoprecipitation. There has been a slight increase in the number of tests performed over time. There was a fall in testing immediately at the beginning of the pandemic, but this has returned to pre-pandemic levels (Graph 1). Pre-pandemic an average 480 tests per year were carried out, compared to 518 tests per year since. The total proportion of patients testing positive for any MSA or MAA was 38.28% and is not significantly different between pre and post pandemic (37.25% vs 39.62% p=0.22).
Overall, 1.67% of samples test positive for MDA5 (n=44). Pre-pandemic 1.15% were MDA5 positive, compared to 2.23% since (p=0.021 by two-sample test of proportions) (Table 1). Graph 2 shows changing pattern over time. Proportion of MDA5 positive tests has increased by a co-efficient of 0.0049 (95%CI 0.0016-0.0082) per year with test for trend p=0.01.
Conclusion: Despite the dramatic fall in testing during the peak of the pandemic, just over 2 years later antibody testing is increasing at this tertiary centre again, with a higher burden of disease being anti-MDA-5 positive than prior to the pandemic. Given MDA-5 is associated with worse outcomes in idiopathic inflammatory myopathies and a higher burden of interstitial lung disease, further research is warranted to elucidate the clinical relevance of increasing presence of anti-MDA5 and identify if Covid-19 infection or vaccination could be a trigger for this disease.
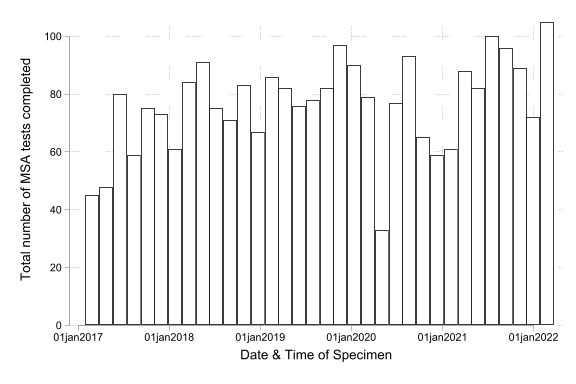 Graph 1. Histogram showing number of MSA tests reported over duration of study
Graph 1. Histogram showing number of MSA tests reported over duration of study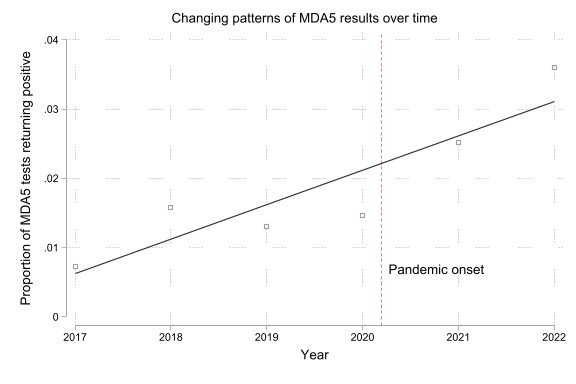 Graph 2. Proportion of MSA tests showing a positive MDA-5 result over time with dotted line demonstrating time pandemic onset
Graph 2. Proportion of MSA tests showing a positive MDA-5 result over time with dotted line demonstrating time pandemic onset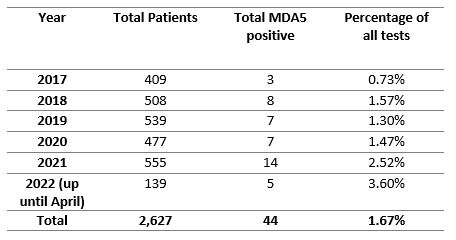 Table 1. Table showing number of MDA5 positive patients per year since 2017. Note that 2022 results only include test up to 31/Mar/2022
Table 1. Table showing number of MDA5 positive patients per year since 2017. Note that 2022 results only include test up to 31/Mar/2022Disclosures: J. Hannah, None; S. Ali, None; S. Arora, None; J. Cazabon, None; J. Galloway, AbbVie, AstraZeneca, Biogen, Celgene, Galapagos, Gilead, Janssen, Medicago, Lilly, Novartis, Novavax, Pfizer, Roche, UCB; P. Gordon, Eli Lilly, UCB, Corbus, Galapagos.

