Back
Poster Session B
Systemic lupus erythematosus (SLE)
Session: (0974–1003) SLE – Treatment Poster II
0995: Association of Glucocorticoid Use with Healthcare Utilization Among Persons with Systemic Lupus Erythematosus
Sunday, November 13, 2022
9:00 AM – 10:30 AM Eastern Time
Location: Virtual Poster Hall
.jpg)
Patricia Katz, PhD
UCSF
San Rafael, CA, United States
Abstract Poster Presenter(s)
Patricia Katz1, Sofia Pedro2, Jiyoon Choi3 and Kaleb Michaud4, 1UCSF, San Rafael, CA, 2Forward, The National Databank for Rheumatic Diseases, Wichita, KS, 3Bristol Myers Squibb, Lawrenceville, NJ, 4University of Nebraska Medical Center, Omaha, NE
Background/Purpose: Glucocorticoids (GCs) have long been a mainstay of treatment for systemic lupus erythematosus (SLE). While GCs do provide benefit, there are potential side effects which increase with dose and duration. GC-associated adverse events have been linked to significant increased health care costs7, although excess healthcare utilization due to GC events has not been examined in SLE. In these analyses, we examine the association of GC use and healthcare utilization.
Methods: Data are from FORWARD, The National Data Bank for Rheumatic Diseases, questionnaires collected from participants with physician-diagnosed SLE and no concomitant RA at 6-month intervals during July 2015 – July 2020. Respondents provided comprehensive health information including GC use and dosage and healthcare use during the prior 6 months. Analyses examined 6-month utilization according to GC use/non-use, as well as by GC dose (0, 1- < 5 mg, 5- < 10 mg, ≥10 mg). For GC users, data were drawn from the questionnaire in which GCs were first reported during the analysis period. Data for non-users were drawn from the first questionnaire completed during the observation period. Adjusted analyses used double selection LASSO1 to form the best fitting model considering the following co-variates: age, sex, race, BMI, comorbidities, education level, smoking, SLE duration, self-reported lupus disease activity, SLE organ damage measured by BILD (Brief Index of Lupus Damage), and other medications. Results of LASSO analyses are reported as incidence rate ratios (IRRs).
1Belloni A, et al. J Economic Perspectives 2014; 28:29.
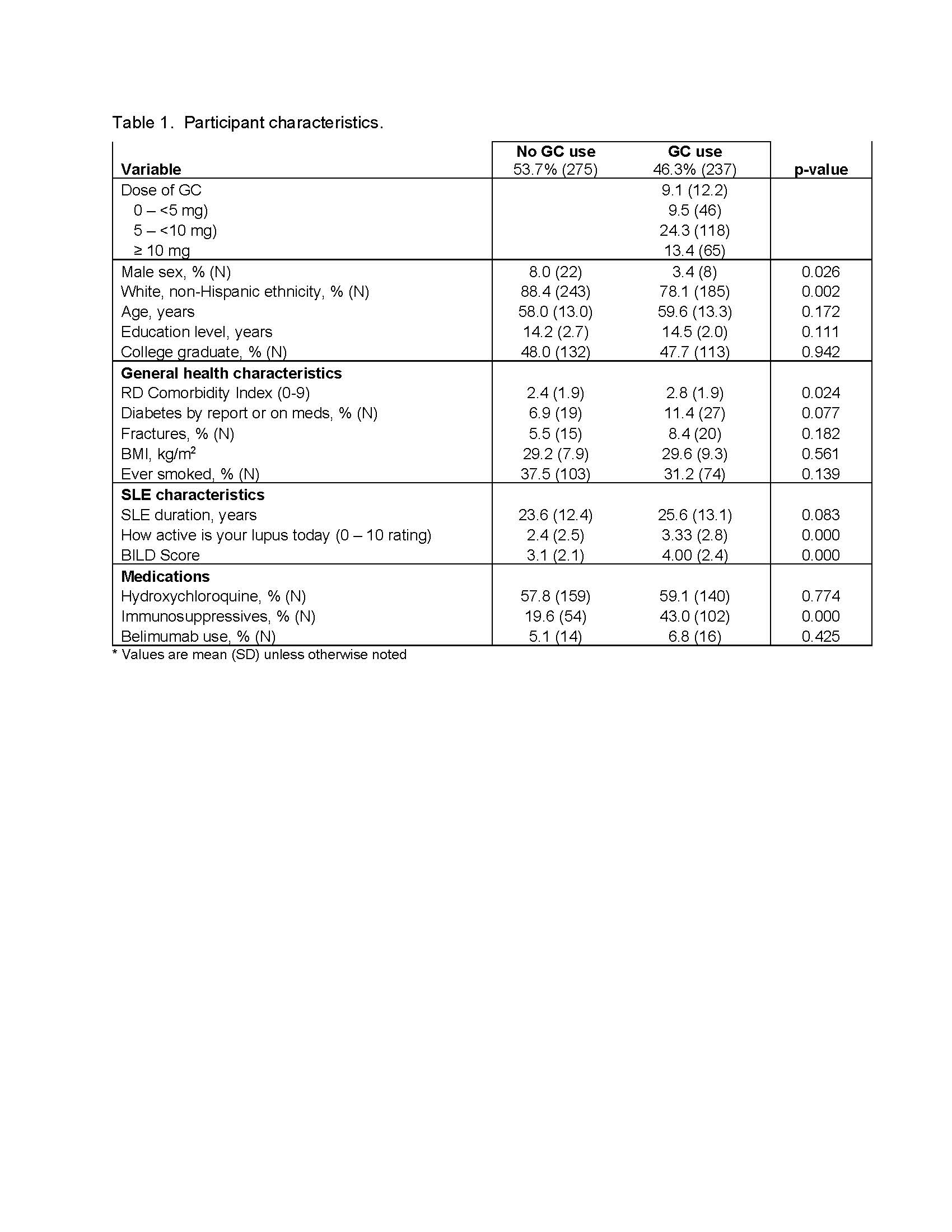
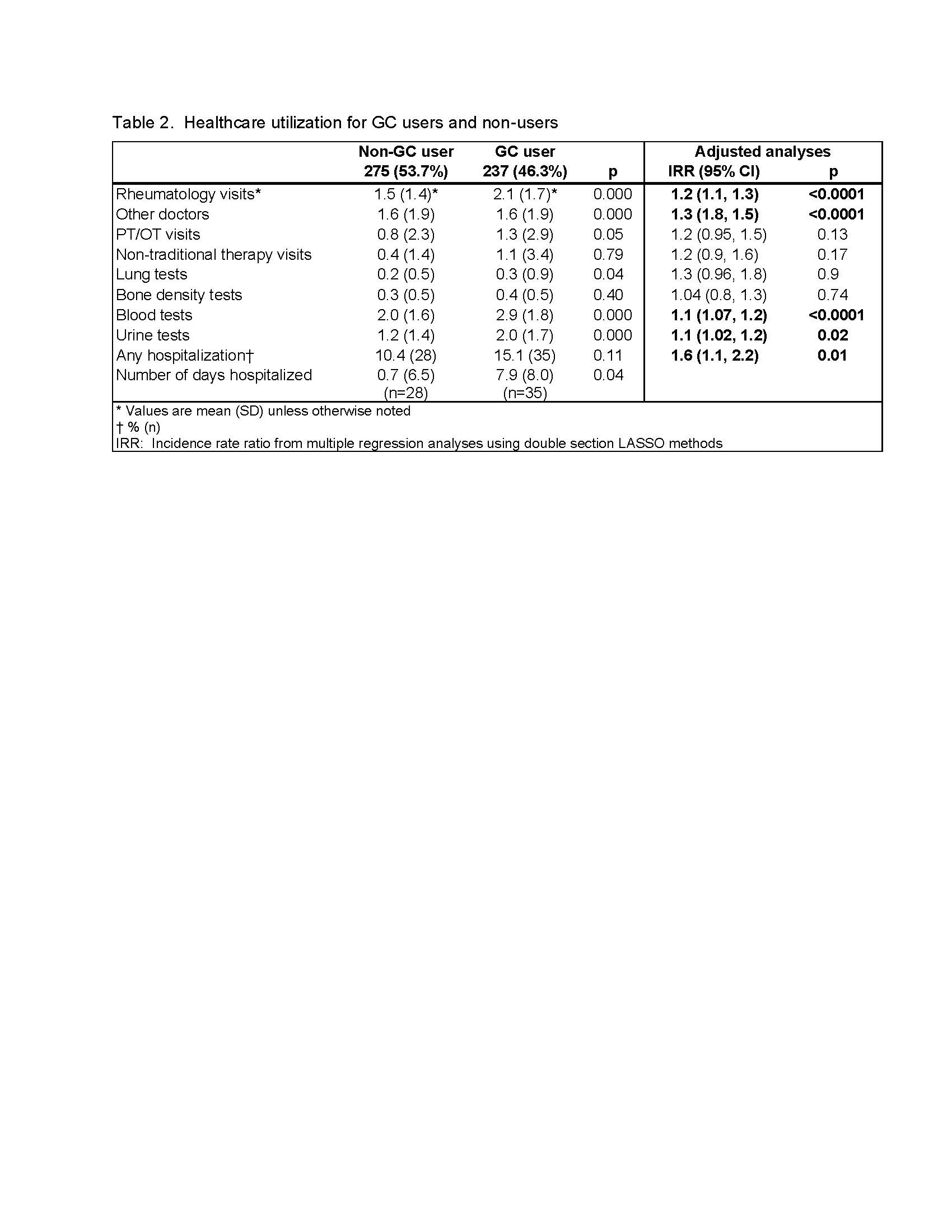
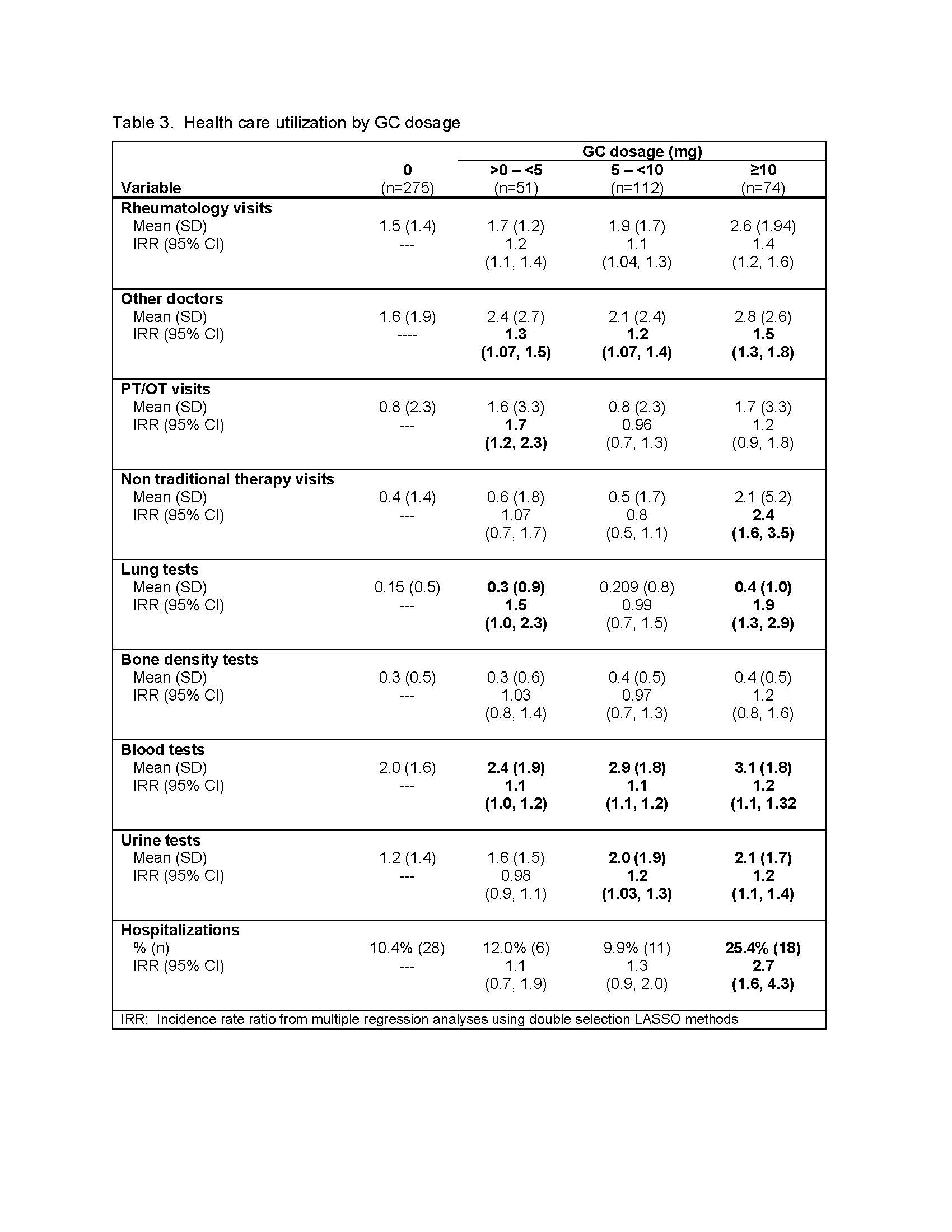
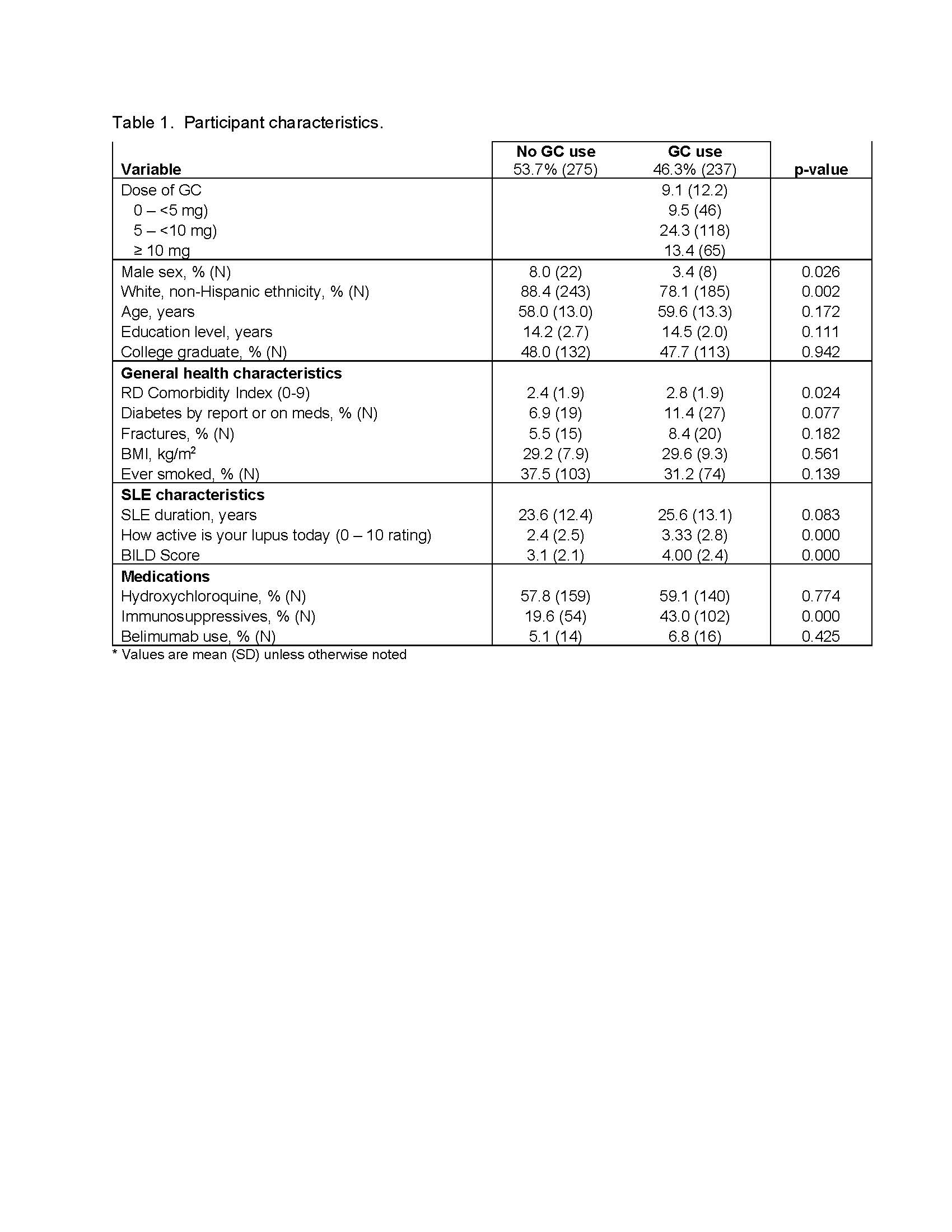
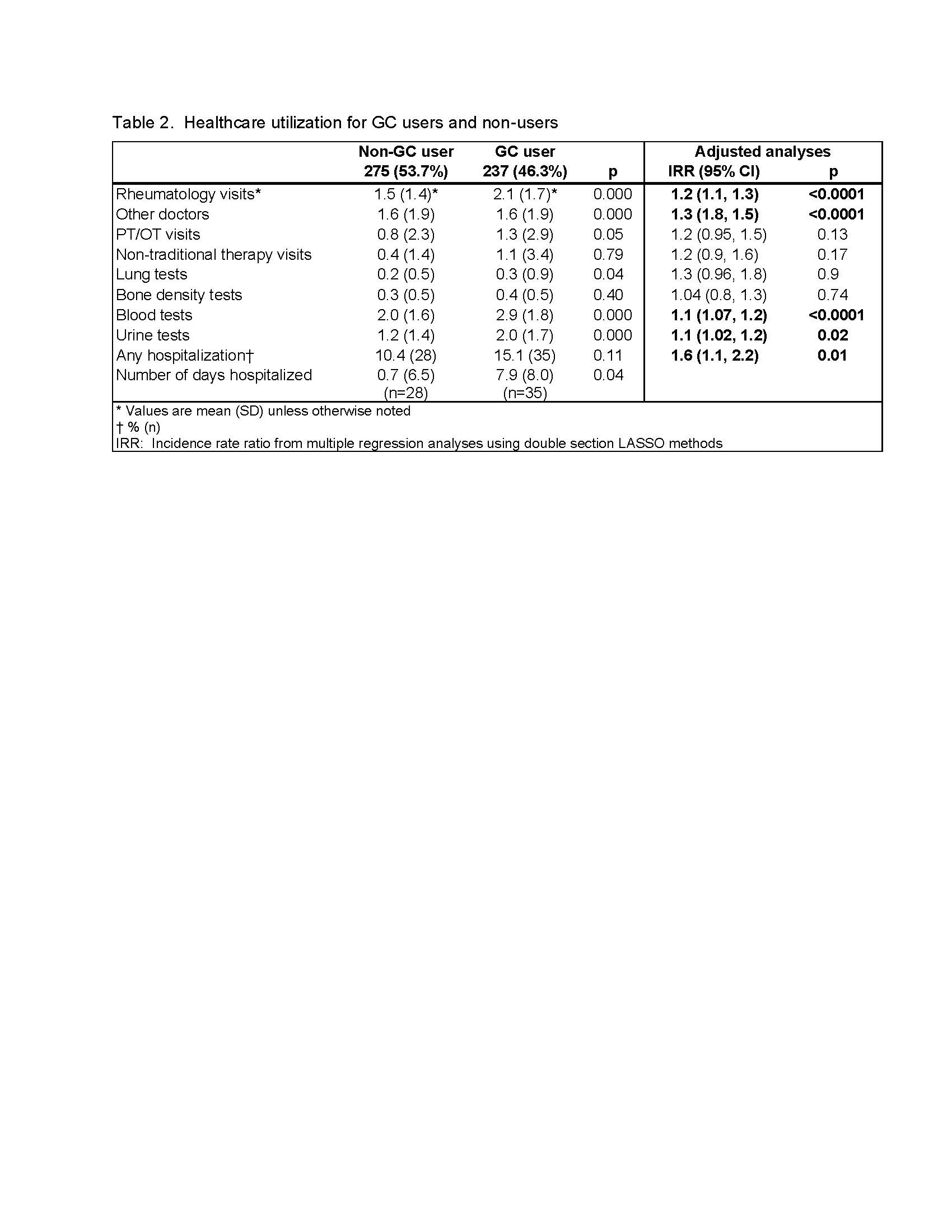
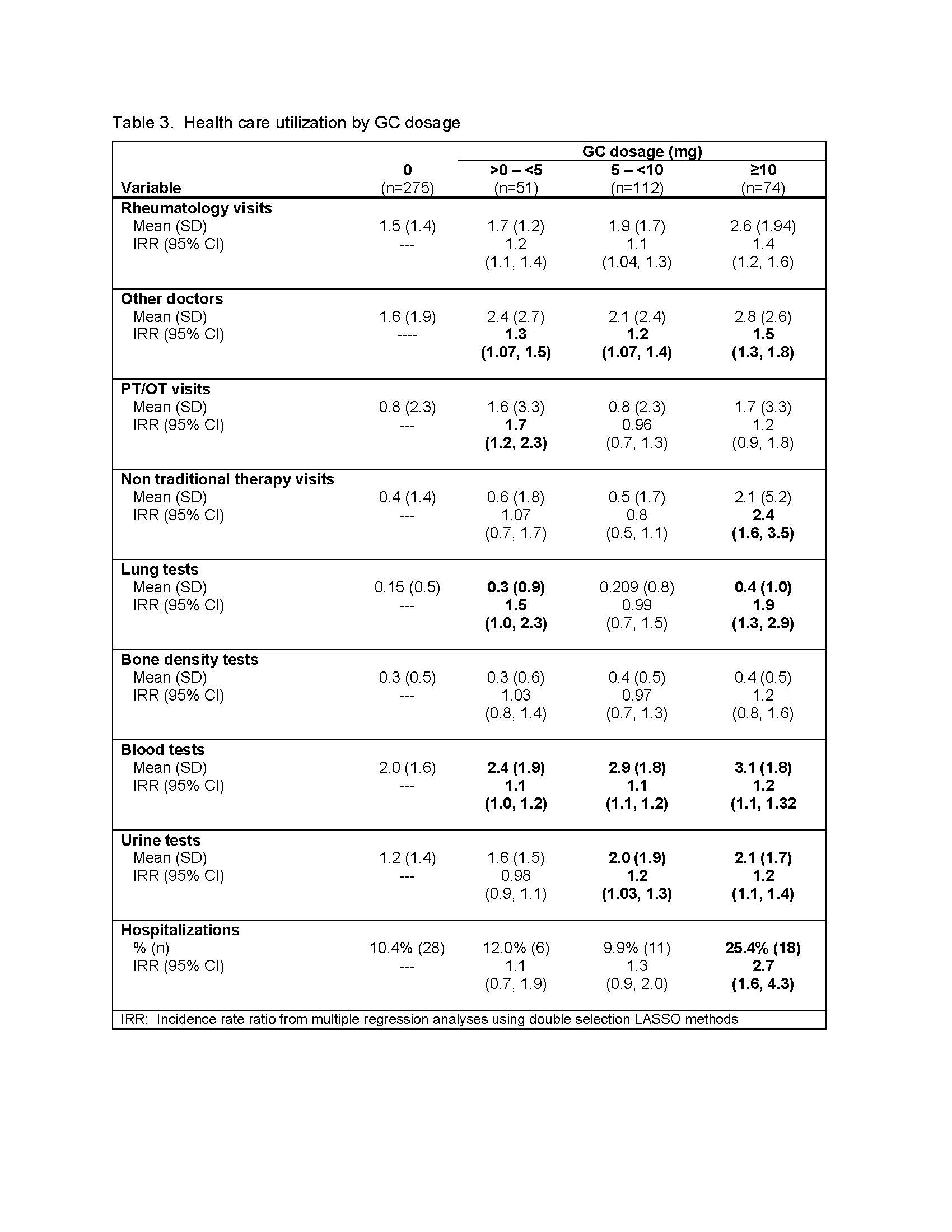
Results: 512 participants qualified for the analysis; 46.3% reported GC use in at least one 6-month period (Table 1). GC users were less likely to be male or white, had more comorbidities, had lupus of greater duration, were more likely to also be taking immunosuppressive medications, and reported more active SLE and greater disease damage (BILD). In bivariate analyses (Table 2), GC users reported significantly more rheumatology and other doctor visits, and more PT/OT visits. They also reported more lung function, blood, and urine tests. There was no difference between GC users and non-users in the occurrence of a hospitalization, but users had significantly longer hospitalizations. The multivariable LASSO regression analyses (Belloni A, et al. J Economic Perspectives 2014; 28:29) revealed similar results, with significantly IRRs for GC users for rheumatology and other visits, blood and urine tests, and hospitalizations. In analyses based on GC dosage (Table 3), IRRs for rheumatology visits, other medical visits and blood tests were significantly elevated for each dosage group compared to the no-GC group; the highest GC dosage group also had significantly elevated IRRs for lung and urine tests and hospitalizations.
Conclusion: GC use is associated with greater healthcare utilization among this cohort with SLE, even after adjusting for a wide range of sociodemographic and disease-related factors. Additional analyses are needed to explore whether greater GC use reflects more severe disease, and/or whether GC use itself leads to increased healthcare utilization.
Disclosures: P. Katz, None; S. Pedro, None; J. Choi, Bristol-Myers Squibb(BMS); K. Michaud, None.
Background/Purpose: Glucocorticoids (GCs) have long been a mainstay of treatment for systemic lupus erythematosus (SLE). While GCs do provide benefit, there are potential side effects which increase with dose and duration. GC-associated adverse events have been linked to significant increased health care costs7, although excess healthcare utilization due to GC events has not been examined in SLE. In these analyses, we examine the association of GC use and healthcare utilization.
Methods: Data are from FORWARD, The National Data Bank for Rheumatic Diseases, questionnaires collected from participants with physician-diagnosed SLE and no concomitant RA at 6-month intervals during July 2015 – July 2020. Respondents provided comprehensive health information including GC use and dosage and healthcare use during the prior 6 months. Analyses examined 6-month utilization according to GC use/non-use, as well as by GC dose (0, 1- < 5 mg, 5- < 10 mg, ≥10 mg). For GC users, data were drawn from the questionnaire in which GCs were first reported during the analysis period. Data for non-users were drawn from the first questionnaire completed during the observation period. Adjusted analyses used double selection LASSO1 to form the best fitting model considering the following co-variates: age, sex, race, BMI, comorbidities, education level, smoking, SLE duration, self-reported lupus disease activity, SLE organ damage measured by BILD (Brief Index of Lupus Damage), and other medications. Results of LASSO analyses are reported as incidence rate ratios (IRRs).
1Belloni A, et al. J Economic Perspectives 2014; 28:29.
Results: 512 participants qualified for the analysis; 46.3% reported GC use in at least one 6-month period (Table 1). GC users were less likely to be male or white, had more comorbidities, had lupus of greater duration, were more likely to also be taking immunosuppressive medications, and reported more active SLE and greater disease damage (BILD). In bivariate analyses (Table 2), GC users reported significantly more rheumatology and other doctor visits, and more PT/OT visits. They also reported more lung function, blood, and urine tests. There was no difference between GC users and non-users in the occurrence of a hospitalization, but users had significantly longer hospitalizations. The multivariable LASSO regression analyses (Belloni A, et al. J Economic Perspectives 2014; 28:29) revealed similar results, with significantly IRRs for GC users for rheumatology and other visits, blood and urine tests, and hospitalizations. In analyses based on GC dosage (Table 3), IRRs for rheumatology visits, other medical visits and blood tests were significantly elevated for each dosage group compared to the no-GC group; the highest GC dosage group also had significantly elevated IRRs for lung and urine tests and hospitalizations.
Conclusion: GC use is associated with greater healthcare utilization among this cohort with SLE, even after adjusting for a wide range of sociodemographic and disease-related factors. Additional analyses are needed to explore whether greater GC use reflects more severe disease, and/or whether GC use itself leads to increased healthcare utilization.
Disclosures: P. Katz, None; S. Pedro, None; J. Choi, Bristol-Myers Squibb(BMS); K. Michaud, None.

